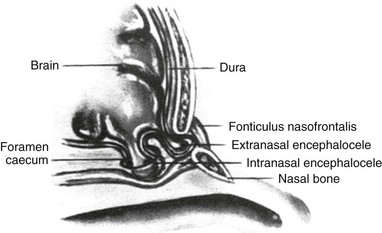
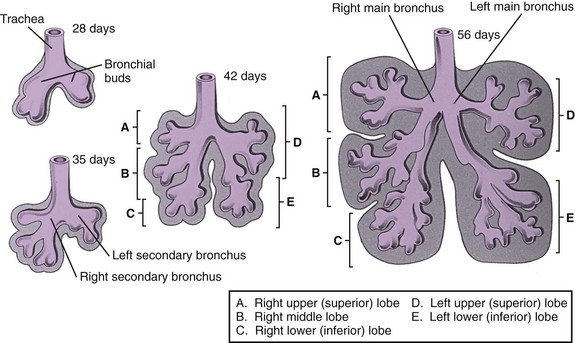
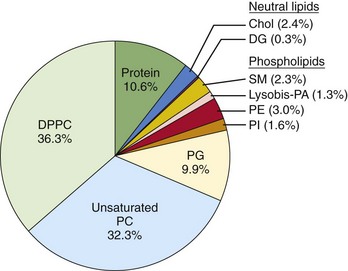
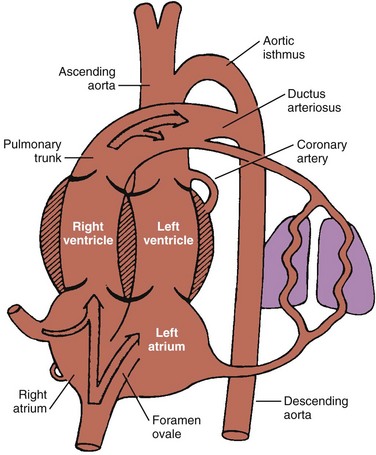
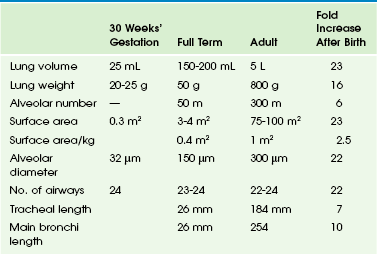
Chapter 48 From a structural and functional perspective, the respiratory system is most logically considered as having conducting and gas exchange components, with the bifurcating airways and accompanying pulmonary arteries (PAs) conducting air and blood to peripheral capillary-lined airspaces for gas exchange. Clements and Warner1 and more recently Bush2 encourage consideration of the lung as a set of branching trees that include the airways, the pulmonary vasculature (arterial and venous), the systemic vasculature (arterial and venous), and the lymphatics. This approach assists the radiologist in understanding accurate descriptions of each of these components in congenital malformations and other pathologic processes. This chapter reviews the developmental biology and clinical anatomy of the respiratory system. The neonatal airway is composed of the nose, pharynx, larynx, trachea, and bronchi. The nasal structures, which are derived from ectoderm, begin developing during the fourth week of gestation.3,4 The olfactory placodes, which are evident as early as the third fetal week, eventually become the nasal pits, which separate into paired medial and lateral boundaries of the nasal walls. The medial portion of the nasal wall fuses during the formation of the nasal septum and central upper lip. The medial and lateral nasal processes fuse with the maxillary processes of the mandibular arch. The nasal cavity extends posteriorly, thinning the oronasal membrane, which eventually ruptures to form the choanae. Persistence of the oronasal membrane leads to choanal atresia.3,5 Incomplete closure of the foramen caecum during the third week of fetal development leads to the formation of gliomas or nasal encephaloceles. Neural tissue remains attached to epidermal elements, preventing normal migration of mesenchymal elements that will form the cartilaginous structures of the midface. This process leads to the presence of a bony defect through which brain tissue may herniate (e-Fig. 48-1). Gliomas have lost their central nervous system attachment, although 15% have a fibrous stalk connecting to the subarachnoid space. Encephaloceles maintain their central nervous system connection.5 Nasal dermoid cysts are benign masses with ectodermal and mesodermal elements. They present as masses on the dorsum of the nose and may have a fistulous opening on the skin or a sinus tract extending into the deep nasal elements. Nasal dermoid cysts are the result of faulty closure of the foramen caecum with invagination of dermal tissue between the developing nasal bones and cartilage.5 The larynx, trachea, and bronchi embryologically arise from a ventromedial diverticulum of the foregut that is known as the laryngotracheal groove. The proliferation of the laryngeal mesenchyme results in the arytenoid swellings that grow toward the tongue, converting the primordial glottis into a T-shaped laryngeal inlet. By 8 weeks, the larynx is usually sufficiently formed. In the infant, the larynx is high in location, with its inferior border located at the C4 level. During childhood, the lower border of the larynx descends and eventually reaches its adult location at the C6-C7 level by age 15 years. Functions of the larynx include breathing, phonation, and protection of the lower airway against aspiration.4,6,7 The laryngotracheal groove grows caudally, forming the trachea. It lies ventral and parallel to the dorsal foregut, which eventually becomes the esophagus. The separation of the trachea and esophagus progresses cranially and is complete by 6 weeks’ gestation. The endodermal lining will produce the epithelium and glandular structures of the trachea, whereas the connective tissue, cartilage, and smooth muscle come from the surrounding splanchnic mesenchyme.4,6,7 Faulty separation of the trachea and esophagus gives rise to esophageal atresia/tracheoesophageal fistula. Disproportionate growth of the esophagus at the expense of the trachea may give rise to tracheal stenosis or, in the most severe form, tracheal agenesis. The lung bud arises from the caudal end of the laryngotracheal groove by the end of the fourth week and soon divides into two bronchial buds.4,8,9 The bronchial buds grow laterally into the pericardioperitoneal canals. Early in the fifth week, the connection of the bronchial buds to the trachea enlarges to form the main stem bronchi. The right main stem bronchus bifurcates into a superior secondary bronchus, supplying the right upper lobe and an inferior secondary bronchus. The inferior bronchus subdivides into two bronchi, supplying the right middle and lower lobes. The left main stem bronchus divides into two secondary bronchi that supply the upper and lower lobes of the left lung. The bronchi continue to divide, and all airway divisions are complete by 16 weeks’ gestation (Fig. 48-2). Cartilage appears at 10 weeks in the trachea and is found in the segmental bronchi by 16 weeks. Unequal growth of the lung buds can lead to the development of unilateral pulmonary agenesis or hypoplasia. Prolonged oligohydramnios or space-occupying thoracic lesions are associated with pulmonary hypoplasia.4,8 Lung development has been divided into five stages (Table 48-1). The embryonic (26 to 52 days) and pseudoglandular (52 days to 16 weeks) stages have been described previously. During the canalicular stage (17 to 28 weeks), the bronchi and terminal bronchioles become larger. The capillary bed begins to approximate the future air spaces, and gas exchange is possible. Type I and type II pneumocytes can be identified in the fetal lung by 20 to 22 weeks, but the capillary-alveolar interface is not adequate for extrauterine survival until 23 to 24 weeks of gestation.4,8,9 The saccular stage (29 to 36 weeks) is characterized by the development of terminal air sacs with flattening of the epithelium in the distal air spaces. The type II pneumocytes produce surfactant, which is stored as lamellar bodies. During the alveolar stage (36 weeks to infancy), the size and number of alveoli increase. When birth occurs at full term, it is estimated that 50 million alveoli are present. Alveolar development continues postnatally, and the mature human lung ultimately has 300 million alveoli (Table 48-2). Table 48-1 Classification of Phases of Human Intrauterine Lung Growth From Thurlbeck WL. Lung growth and development. In Thurlbeck W, Churg AM, eds. Pathology of the lung. 2nd ed. New York: Thieme Medical Publishers; 1995;38. Table 48-2 Changes in Lung Size With Growth From Hodson WA: Normal and abnormal structural development of the lung. In Polin RA, Fox WW, eds. Fetal and neonatal physiology, ed 2, Philadelphia, 1998, WB Saunders, p 1037. Surfactant is composed of phospholipids, protein, and neutral lipids (e-Fig. 48-3). Surfactant lines the alveoli and decreases surface tension, which leads to decreased work of breathing and stabilizes the terminal air spaces, especially at low lung volumes.10 Surfactant can be detected as early as 24 to 26 weeks’ gestation, although mature surfactant usually is not present until 34 to 36 weeks’ gestation. Surfactant maturation can be affected by a variety of substances. Insulin delays surfactant maturation, whereas other substances, such as glucocorticoids and thyroid hormone, accelerate it.11 Administration of glucocorticoid to mothers 24 to 48 hours before preterm delivery accelerates surfactant maturation and results in a significant decrease in the incidence and severity of hyaline membrane disease (HMD). HMD is the result of surfactant deficiency and is characterized clinically by cyanosis, tachypnea, and retractions within a few hours of delivery. Tracheal instillation of exogenous surfactant can ameliorate the natural course of HMD significantly.12 The fetal lung is filled with fluid during gestation. This fluid is produced by pulmonary epithelial cells, and its composition is different from that of amniotic fluid.13 As the fetus matures, surfactant can be found in this lung fluid. Fetal lung liquid is under higher pressure than amniotic fluid, and efflux of lung liquid into the amniotic fluid occurs, which is the basis of amniotic fluid analysis for surfactant to determine fetal pulmonary maturity. The fetal lung is the only organ that does not perform its postnatal function before birth. No reason exists for cardiac output to go to the fetal lungs because all gas exchange occurs via the placenta. Oxygenated blood returns to the fetus via the umbilical vein to the inferior vena cava (IVC) and right atrium (RA). Approximately two thirds of the IVC return entering the right atrium crosses the foramen ovale into the left atrium. The remaining one third of the IVC return and all of the superior vena cava (SVC) return enter the right ventricle. Most of the right ventricle output crosses the ductus arteriosus (DA) into the aorta. These shunts at the foramen ovale and DA result in most of the fetal cardiac output bypassing the lungs (Fig. 48-4).14
Embryology, Anatomy, and Normal Findings
Developmental Biology
Lungs
Phase
Time of Occurrence
Significance
Embryonic
26-52 days
Development of trachea and major bronchi
Pseudoglandular
52 days to 16 wk
Development of remaining conducting airways
Canalicular
17-28 wk
Development of vascular bed, framework of acinus; flattening of epithelium
Saccular
29-36 wk
Increased complexity of saccules
Alveolar
36 wk to term
Presence and development of alveoli
Surfactant
Fetal Lung Liquid
Pulmonary Vasculature/Circulation
Embryology, Anatomy, and Normal Findings