Fig. 5.1
Axial section gray-scale 3D image, transducer 8838. Symphysis pubis (“gothic arch”)—reference points of symmetry in axial section for transducers 8848, 2050, and 2052 (B–K Medical). SP symphysis pubis, RP Retzius plexus, U urethra, RS rhabdosphincter, T transducer in vagina, VH vaginal hammock, LA levator ani, A anal canal
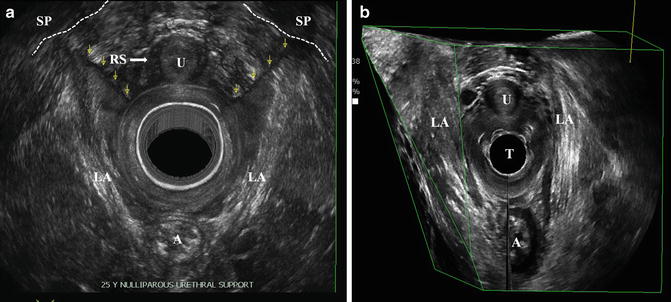
Fig. 5.2
Axial section render mode, transducer 2052 (B–K Medical) (a). Levator ani and anterior vaginal wall attachments to symphysis pubis (SP). U urethra, RS rhabdosphincter, SP symphysis pubis, LA levator ani, A anal canal; Multisurface 3D reconstruction, transducer type 8838 (B–K Medical) (b). Attachments of levator ani fibers to symphysis pubis are well demonstrated on oblique sections. U urethra, T transducer in vagina, LA levator ani, A anal canal
The main advantage of the transducer is a large region covered during acquisition (360°, all compartments) which provides a very good overview of all pelvic floor organs making the transducer universal for many specialties and many purposes. An important prone is also a wide selection of scanning time and the quality of obtained image. The universal character of the 2050/2052 transducer makes it a gold standard diagnostic tool in proctology [6, 7] and for pelvic floor diagnostics, as described in 2009 by Santoro et al. [4, 5, 8].
The main limitation of this technology is the total length of the transducer of 54 cm which is not particularly handy, difficult for operation, hard to be kept in a stable position, and also often recognized by patients as extremely long which creates an extra anxiety for the patient. From the methodological point of view mechanical character of the transducer does not allow to obtain the same resolution in all sections, only the axial section (the section of acquisition) has the best quality and all other sections coming from post-processing of the 3D volume dataset have lower resolution.
The 8848 Transducer
This is an electronic biplane, high frequency 5–12 MHz, multielement high-resolution transducer, working both in 2D and 3D modes with 6.5 cm linear and convex views transducer (See specifications in the chapter on instrumentations and techniques). The transducer has the focal range from 3 to 60 mm and contact surface in axial section of 127 mm2, in sagittal section 357 mm2. High frequency provides high resolution of examined organs allowing for very good assessment of urethral morphology. It gives the best broad view of anterior and posterior compartments for functional and anatomical studies. This transducer requires an external mover to obtain reliable 3D volumes. Obtained 3D volume dataset of the anterior compartment of pelvic floor may be analyzed in midsagittal, axial, coronal, and oblique sections.
Sagittal Section
The reference organ to maintain symmetry in the sagittal section is the visualization of the urethral lumen on the entire length from the bladder neck to the external orifice (Fig. 5.3). A longitudinal array enables to obtain 2D and 3D volume dataset in a sagittal section as a free-hand acquisition, during maximum time of 13.4 s with minimal spacing of 0.2 mm. Free-hand acquisition may be connected to artefacts due to uneven move of the hand in time, which may distort the anatomy and create an artificial nonexisting asymmetrical position of urethra and the pelvic floor structures and their abnormal shape. Free-hand acquisition may be however performed on a normal flat couch. Reproducible 3D studies may be performed with external mover. The examination can be performed both in B-mode and in Color/Power Doppler modes.
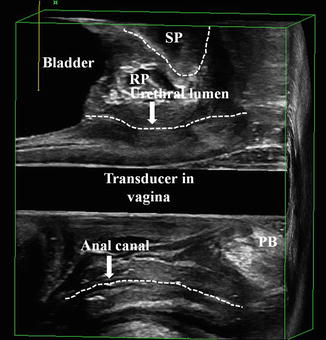
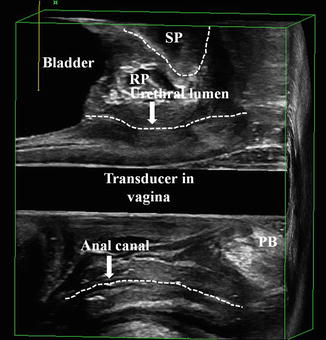
Fig. 5.3
Sagittal section 3D gray-scale image with a biplane 12-MHz transducer (type 8848, B–K Medical). Entire urethral lumen from the bladder neck to the external orifice as reference point of symmetry in sagittal section for transducers 8848, 8838, 2050, and 2052 (B–K Medical). SP symphysis pubis, RP Retzius plexus, PB perineal body
To avoid artefacts connected to free-hand acquisition the examination may be performed with the use of automatic external mover (as described in the chapter on 3D/4D instrumentation and techniques). In order to safely use the mover the examination must be performed on a gynaecological chair. With the use of the mover the ultrasound acquisition may be performed in a maximum of 179°, during 46.5 s in B-mode and in 51.2 s in Color Doppler.
Axial Section
The reference points to maintain symmetry of the image in the axial section is the “gothic arch” the same as in 2050/2052 transducer (Fig. 5.1). Any asymmetrical insertion of the transducer to the vagina may cause bias in the obtained image, in the echostructure of the examined organs and their dimensions and measurements.
The length of acquisition may be selected by operator. In axial section choosing minimal spacing of 0.2 mm the acquisition time of 11.91 s covers 6 cm. The button placed on the transducer switches the image between the two arrays.
The 3D acquisition in axial section may be only free-hand, which may result in inappropriate urethral measurements due to distorted 3D anatomy. This section in 2D and the offline analysis of the 3D volume dataset allows for differentiation of various parts of the urethra such as intramural anatomical elements (layer structure of the trigone, trigonal ring), mid-urethra (differentiation for rhabdosphincter, longitudinal and circular smooth muscle, submucosal venous plexus) and the distal urethra (fibers of the compressor urethra) and reliable assessment of the urethral relations to external anatomical structures such as vaginal wall or attachments of levator ani muscle fibers to the symphysis pubis.
Transducer Type 8838
This is an electronic transducer, for endovaginal and endoanal/endorectal imaging, with automatic high resolution 3D acquisition transducer (See specifications in the chapter on instrumentations and techniques). Built-in linear array rotates 360° inside the transducer with no need for additional accessories or external mover. It enables both dynamic 2D and 3D scanning at wide frequency range from 6 to 12 MHz. Its slim diameter (16 mm) is more comfortable for the patient, easy to hold and manipulate for the operator. Two-dimensional scanning plane is controlled remotely from the system keyboard. The image field of 65 mm is covering the entire urethra from the bladder base to the external orifice. Two-dimensional acquisition can be obtained only in longitudinal (sagittal) section. The reference section to obtain symmetry is the lumen of the urethra visualized on the entire length similarly as in the sagittal section with use of 8848 transducer (Fig. 5.3). The urethra may be assessed as a separate organ with a small region of interest (ROI) e.g., 45° or as a part of the entire overview examination of all pelvic floor in a 3D file of almost 360° (with a tiny blank stitch) with the time of acquisition at maximal length equaling 41.9 s with spacing of 0.4°. The spacing may be changed which influences the examination time. Electronic character of the transducer allows assessing the vascularity and flow in Power and Color Doppler modes. The Doppler assessment may be performed either as a 2D examination and can be recorded as a video life file on a selected section or as a static 3D volume dataset.
The axial section may be obtained only in post-processing from the 3D volume dataset. Lack of axial acquisition limits the possibility to use the symphysis pubis (“gothic arch”) as a reference point of symmetry. Inappropriate position of the transducer and B-mode obtained only in sagittal section may result in asymmetry of the organs in a 3D file (Table 5.1).
Table 5.1
Endovaginal (EVUS) 2D/3D of the urethra—characteristics of the transducers and reference points
Transducer | Arrays | Sections of acquisition | Type | Frequency (MHz) | Doppler | 3D acquisition | Reference points | Range of view |
|---|---|---|---|---|---|---|---|---|
2050/2052 | Two arrays (low and high frequency crystals) | Axial | Mechanical | 9–16 | No | Automatic built-in | Gothic arch (axial) | 360° |
8848 | Two arrays (linear multielement, transverse multielement) | Axial | Electronic | 5–12 | Yes | Free-hand or external mover | Gothic arch (Axial) | 180° |
Sagittal | Urethral lumen (sagittal) | |||||||
8838 | Linear multielement array | Sagittal | Electronic | 6–12 | Yes | Automatic built-in | Urethral lumen (sagittal) | 360° (tiny blank stitch) |
5.2.4 Vascular Render Mode and Maximum Intensity Projection
Volume render mode is a technique for the analysis of the information inside 3D-volume by digital enhancing of individual voxels (Fig. 5.2a, b). It is currently one of the most advanced and computer-intensive rendering algorithm available for computed tomography and can also be applied to high-resolution 3D-US data volume [9]. The typical ray/beam-tracing algorithm sends a ray/beam from each point (pixel) of the viewing screen through the 3D space rendered. The beam passing through the volume data, reaches the different elements (voxels) in the data set. Depending on the various render mode settings, the data from each voxel may be stored as a referral for the next voxel and further used in a filtering calculation, may be discarded or may modify the existing value of the beam. The final displayed pixel color is computed from the color, transparency, and reflectivity of all the volumes and surfaces encountered by the beam. The weighted summation of these images produces the volume-rendered view [9]. Vascular render mode refers to the application of render mode to 3D-data volume with Color Doppler acquisition to provide the visualization of the spatial distribution of the vascular networks.
Maximum intensity projection (MIP) is a 3D visualization modality involving a large amount of computation. It can be defined as the aggregate exposure at each point, which tries to find the brightest or most significant color or intensity along an ultrasound beam. Once the beam is projected through the entire volume, the value displayed on the screen is the maximum intensity value found (the highest value of gray or the highest value associated with a color). The application of MIP in a 3D color mode reduces the intensity of the gray-scale voxels so that they appear as a light fog over color information, which is in this way highlighted. In a color volume the colors are mapped to a given value in the volume.
Urinary Bladder
Specific features of each of the transducers parameters condition the range of obtained anatomical information. However, none of the described transducers is appropriate for the assessment of the entire urinary bladder due to endovaginal access and the beam formation perpendicular to the organ. The bladder may be visualized only partially, in the range depending on bladder filling. The assessment of the entire bladder has to be performed by transabdominal ultrasound or with the use of endovaginal end-fire transducers used widely in gynecology or urology.
5.3 Anatomy of Female Urethra and Bladder
5.3.1 Ultrasound Morphology
Endovaginal insertion of the transducer can influence the position of examined organs and may limit the reliability of the dynamic studies such as Valsalva and squeeze maneuvers. Stankiewicz et al. proved that in incontinent women with no coexisting POP both ultrasound methods (TPUS and EVUS) have the same accuracy in the measurements of urethral complex and bladder-symphysis distance (BSD) at rest and during Valsalva maneuver. The study demonstrated that in females suffering from stress urinary incontinence (SUI) and coexisting POP, the endovaginal examination is not reliable in the assessment of the urethral mobility due to alterations of anatomical relations that result from introduction of the transducer into the vagina. Endovaginal approach is more appropriate for detailed assessment of urethral morphology (Fig. 5.4), while TPUS is the method of choice for dynamic assessment [8].
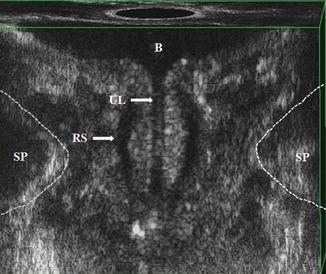
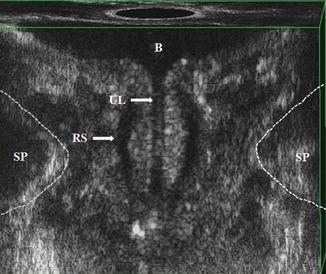
Fig. 5.4
Coronal 3D section showing bladder neck and urethral lumen with a transducer type 2050 (B–K Medical). B bladder, UL urethral lumen, RS rhabdosphincter, SP symphysis pubis
All described transducers used in EVUS allow proper assessment of ultrasound morphology of the pelvic floor organs including the urethra and the surrounding structures on different pelvic floor sections and levels as previously defined by Santoro et al. [5, 10]:
Level I: the highest level visualizing the bladder base on the screen at 12 o’clock position and the inferior third of the rectum at 6 o’clock position;
Level II: corresponds to the bladder neck, the intramural region of the urethra, and the anorectal junction;
Level III: corresponds to the mid-urethra and to the upper third of the anal canal. To facilitate the assessment of the position of these structures, a geometric reference point, termed as the “gothic arch,” was defined at 12 o’clock position, specifically at the point where the inferior branches of the pubic bone join at the symphysis pubis (SP). At this level, the pubovisceral muscle (PVM) (synonymous with the term pubococcygeus/puborectalis muscle) can be completely visualized as a multilayer highly echoic sling lying posteriorly to the anal canal and attaching to the pubic bone;
Level IV: the outer level, the superficial perineal muscles, the perineal body, the distal urethra, and the middle and inferior third of the anal canal can be evaluated. To visualize these structures in their entirety, the reconstructed axial section should be tilted from the most protruding surface of the SP anteriorly to the ischiopubic rami laterally. In the same scan the urogenital hiatus (UGH) can be evaluated.
The following measurements of the urethra may be performed (Table 5.2) (Fig. 5.5):
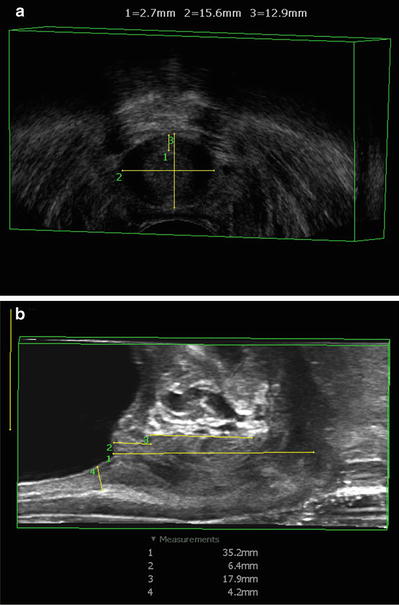
Table 5.2
Measurements of the urethral structures obtained by 3D-EVUS taken by three observers
Observer 1 | Observer 2 | Observer 3 | ICC (95 % CI) | |
|---|---|---|---|---|
Mean (SD) | Mean (SD) | Mean (SD) | ||
BSD (mm) | 34.01 (5.1) | 33.9 (5.05) | 33.9 (5.2) | 0.964 (0.931–0.983) |
Urethra length (mm) | 41.2 (5.6) | 40.9 (4.56) | 40.7 (5.2) | 0.975 (0.918–0.980) |
Urethra width (mm) | 13.1 (1.44) | 13.24 (1.5) | 13.1 (1.45) | 0.892 (0.801–0.947) |
Urethra thickness (mm) | 11.6 (1.3) | 11.02 (3.2) | 11.4 (1.25) | 0.848 (0.697–0.929) |
Urethra volume (ml) | 4.99 (1.3) | 5.12 (1.38) | 4.82 (1.32) | 0.925 (0.86–0.964) |
Intramural length (mm) | 7.3 (1.7) | 7.3 (1.25) | 7.5 (1.5) | 0.870 (0.764–0.936) |
RS length (mm) | 18.6 (2.9) | 19.1 (2.6) | 19.0 (2.6) | 0.942 (0.889–0.972) |
RS width (mm) | 35.3 (4.07) | 35.2 (4.1) | 34.3 (3.9) | 0.85 (0.728–0.926) |
RS thickness (mm) | 2.4 (0.21) | 2.47 (0.23) | 2.4 (0.24) | 0.611 (0.390–0.789) |
RS volume (ml) | 1.27 (0.35) | 1.28 (0.38) | 1.24 (0.32) | 0.909 (0.829–0.957) |
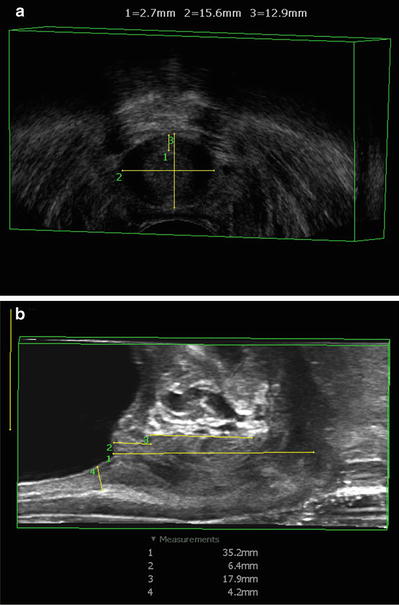
Fig. 5.5
Axial (a) and sagittal (b) section, 3D gray-scale mode with a transducer type 8848 (B–K Medical) demonstrating measurements of the urethra performed in the 3D viewer
In midsagittal plane
1.
Urethral length (Ul) measured from the bladder neck to the external meatus along the urethral longitudinal axis.
2.
BSD measured from bladder neck to the lowest margin of the symphysis pubis. According to Wieczorek et al. [11] frequency the mean value of the BSD varied from 33.9 to 34.01 mm for depending on the observer.
3.
Rhabdosphincter length (RSl) measured in anterior part of the urethra.
4.
The distance between bladder neck and rhabdosphincter corresponding to the intramural part of the urethra.
In axial plane of the mid-urethra
5.
Urethral complex width (Uw).
6.
Urethral complex thickness including Rhabdosphincter (Ut).
7.
Width of the rhabdosphincter measured along its external border, where it is attached with the smooth muscle to the rhabdosphincter raphe—a tissue connection to the anterior vaginal wall (RSw); this is a summing value of the linear measurements performed by the use of tools available in B–K 3D Viewer. Rhabdosphincter appears in the axial section as a slightly hyperechoic (compared with urethral smooth muscle) structure surrounding ventral and lateral sides of the mid-urethra and forming a raphe connected to the anterior vaginal wall. Thus, rhabdosphincter has its typical omega shape [11].
According to integral theories described by Petros and Ulmsten between the mid-urethra and the vaginal anterior wall there are pubourethral ligaments and the suburethral vaginal hammock [1, 2]. This hammock is attached to the endopelvic fascia, and laterally the urethra is limited by periurethral space including Retzius vascular plexus, and by the elements of levator ani. On the section when levator hiatus is well visible also the paravaginal spaces can be determined, located between the lateral border of the vaginal wall and the medial border of the PVM. Shobeiri et al. demonstrated levator ani subdivisions visible on endovaginal three-dimensional ultrasonography at three levels, where level 2 contained the attachment of the pubovaginalis, puboperinealis, puboanalis, puborectalis, and iliococcygeus to the pubic bone [12]. It is possible to explain deterioration of continence with time in terms of age-related connective tissue laxity of the vaginal hammock. Improvement in continence after anti-continence surgery with time can be explained by tightening of the hammock via paraurethral scar contraction with time [13].
The review of the literature shows significant differences in the assessment of the anatomy of the urethra, its dimensions and volume [4, 5, 11, 14–17]. Santoro et al. in the study performed with high-resolution three-dimensional EVUS 2050 transducer demonstrated urethral length of 38.2 mm, urethral volume of 3.06 ml, and rhabdosphincter volume of 0.45 ml [5]. The results published by Wieczorek et al. [11] performed with the same type of transducer (2050) where urethral length was reported at 41.0 mm, urethral volume 4.9 ml, and rhabdosphincter volume 1.2 ml. The difference between rhabdosphincter volume between Santoro and Wieczorek results most probably from different mathematical algorithm used for calculating the volume and also unclear borders in sagittal section which may be interpreted differently by various operators. Similar results were presented also by Shobeiri et al. in the study on anterior and posterior compartment 3D EVUS with 8848 probe based on direct histologic comparison where urethral length was reported as 36.0 mm [18]. Additionally Shobeiri et al. obtained the following mean measurements of other pelvic floor structures: striated urogenital sphincter area 0.6 cm2; longitudinal and circular smooth muscle area 1.1 cm2; urethral complex width 14 mm; and urethral complex area 1.3 cm2. The agreement for visualization of structures was as follows: vesical trigone 96 %, trigonal ring 94 %, trigonal plate 84 %; longitudinal and circular smooth muscle 100 %; compressor urethra 97 %; and striated urogenital sphincter 97 % [18].
The above results are concordant also with those obtained by Kondo et al., where morphology obtained in transvaginal ultrasonography was confirmed on cadaver specimens. The rhabdosphincter (peripheral zone) thickness was reported in various patients’ groups: continent, patients with SUI and UUI as 2.78 mm, 2.14 mm, and 2.87 mm, respectively [19]. Above results are also accordant to those obtained by Macura et al. in the MR study on urethral morphology [20]. These results are slightly different to those obtained by Umek et al. who presented sagittal urethral diameter of 8.4 mm if measured in endovaginal access and 11.5 mm measured from endoanal access, urethral volume of 1.6 ml (both anatomical accesses) and rhabdosphincter volume of 0.7 and 0.8 ml accordingly [16]. In the study performed by Santoro et al. with 2050 transducer [4] involving the interobserver, intra and interdisciplinary reproducibility of pelvic floor measurements the sole urethral dimension measured was urethral thickness. The results were concordant with urethral dimensions obtained in all the above studies [4]. Moreover, as the study focused mainly on the reproducibility of the performed measurements in EVUS among various specialties (urogynecologists, colorectal surgeons, radiologists) and different experience in ultrasound diagnostics of operators and the conclusions from the study were that 3D-EVUS yields reproducible measurements of levator hiatus dimensions and urethral thickness in asymptomatic nulliparous women. Agreement was best where landmark edges were well defined (LH dimensions) and acceptable where more reader judgment was needed (urethral thickness in the oblique axial plane). Using standardized criteria, the evaluation of these pelvic floor structures appeared to be independent from the different background training of the readers. The method appeared a reproducible technique for urethral measurements [4].
The rhabdosphincter may be also evaluated during intraurethral ultrasound as reported by Frausher et al. This technique provides excellent high-resolution images and allows for real-time visualization of the sphincter mechanism [21]. The rhabdosphincter thickness for patients with urge incontinence and for patients with combined stress and urge incontinence was reported as 3.2 mm.
However, the volumes of rhabdosphincter given generally in the literature seem to be significantly lower than reported by Digesu et al. [14] and Derpapas et al. [17]. The study by Digesu et al. demonstrated the rhabdosphincter volume of 3.79 ml in patients with successful surgical procedure due to SUI, while in patients with failures 1.09 ml. In the paper by Derpapas et al. the rhabdosphincter volume was 8.88 ml in black women and 5.97 ml in white females. Both studies were performed from transperineal (TPUS) access: the study by Digesu et al. with the use of sector, endovaginal transducer and the study by Derpapas et al. with 3D/4D curved array probe [14, 17].
The differences may result from the various nomenclature of urethral anatomy treated differently by different authors. There are many controversies in female urethral anatomy which have a significant impact for understanding urinary continence [22]. Variability of obtained results among authors may also result from various frequencies of the transducers used, different anatomical accesses, and various patient groups (age, race, BMI, parity, etc.). The differences in urethral morphology and physiology between black and white women have been already reported in the literature [17, 23]. Howard et al. reported that black women demonstrated difference in ultrasonically measured vesical neck mobility during a maximum Valsalva effort compared to white females (blacks = −17 mm vs. whites = −12 mm). Functional and morphologic differences exist in the urethral sphincteric and support system of nulliparous black and white women [23].
Moreover, the diagnostics of such a small organ as urethra may relatively easily result in variability of the measurements obtained in various techniques among the authors. Moreover, the review of the literature concerning 3D diagnostics of urethral complex shows that most researchers perform only one acquisition in axial plane to obtain 3D dataset, which also may potentially influence obtaining reliable measurements in all three planes.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree