Fig. 1
(a–f) DWI shows the extension of the ischemic core

Fig. 2
(a, b) MR angiography shows the presence of a proximal carotid occlusion associated with M1 intracranial occlusion (tandem occlusion)

Fig. 3
(a, b) DSA shows the occlusion of the cervical carotid artery due to an atherosclerotic plaque. (c, d) DSA shows the intracranial M1 occlusion; the angiographic run was performed with a coaxial catheter navigated through the proximal stenosis
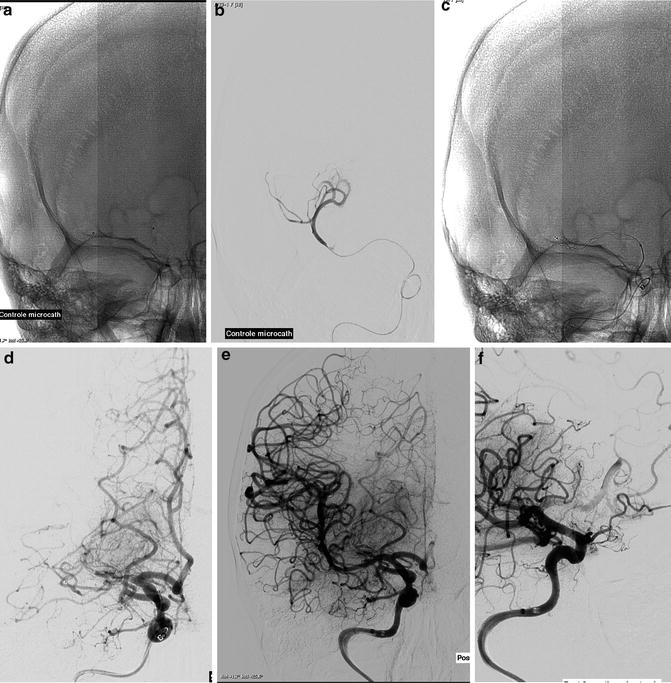
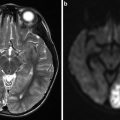
Fig. 4
(a, b) DSA run performed with a micro-catheter navigated within the M1 occlusion. (c, d) DSA run performed after deployment of the stent retriever. (e, f) DSA run performed after retrieving of the stent retriever: complete reopening of M1, presence of an embolic occlusion of the anterior cerebral artery
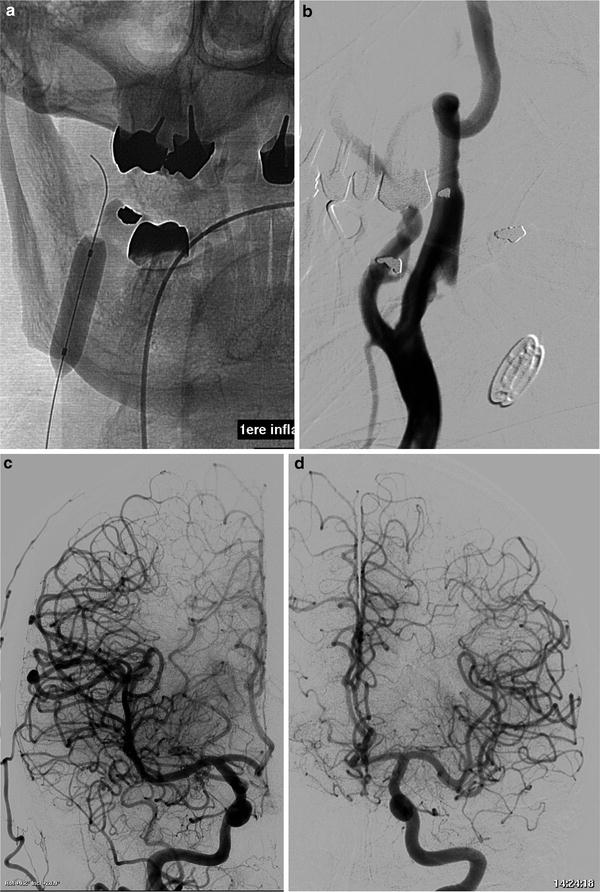
Fig. 5
(a, b) Stand-alone angioplasty of the proximal cervical carotid stenosis. (c, d) Final DSA control shows reopening of the right anterior cerebral artery

Fig. 6
(a–d) Stenting of the cervical stenosis performed 15 days after the acute phase initial treatment
Rationale for Endovascular Treatment of Tandem Occlusions
Tandem occlusions have been previously treated by stand-alone intravenous fibrinolysis. Nevertheless, efficacy of such approach in comparison with cases of isolated M1 occlusions seems to be reduced [18, 19]. Tandem occlusion is an independent risk factor for poor clinical outcome for patients treated exclusively with intravenous fibrinolysis [20]. Furthermore, intravenous fibrinolysis presents reduced efficacy also in cases of carotid bifurcation “T” occlusions [21]. In cases of tandem occlusion, prompt intracranial recanalization is related to improved clinical outcome regardless of persistence of the proximal cervical occlusion [22].
Ozdemir et al. [23] published results of a study involving eight patients presenting with tandem occlusion strokes. In this series the intracranial clot was treated by local injection of rt-PA released through a micro-catheter navigated via the communicating artery system to the intracranial thrombus. The proximal cervical occlusion of patients of this series was not treated and the vessel remained occluded. This technique led to intracranial recanalization only in two out of eight patients, in spite of low rate of cerebral revascularization; all patients with a functioning communicating artery system had favorable outcome at 3 months. Nevertheless, the persistence of the cervical thrombotic occlusion could be a source of potential new emboli; this is an independent risk factor for early re-occlusion after rt-PA [21]. Lavalée et al. [24] reported on a series of ten patients presenting with tandem occlusion strokes due to cervical carotid dissection. Among them, four out of ten patients received intravenous rt-PA, while six patients underwent mechanical clot fragmentation. In all patients treated by mechanical approach, a complete recanalization of the involved vessel was achieved. Authors stated that endovascular treatment seems to be more effective than the standard intravenous treatment. They did not specify whether this approach would be effective also in cases of tandem occlusions due to cervical carotid atherosclerotic plaques.
Malik et al. [25] reported a series of 27 patients presenting with tandem occlusions treated by intra-arterial administration of rt-PA performed prior to stenting of the cervical carotid. In this series clot removal/disruption was performed with different techniques and tools: Merci clot retrieval device, Penumbra system, or by angioplasty and/or stent stenting. Patients of this series were treated under systemic heparinization. Moreover, patients received a bolus of intravenous eptifibatide upon stent deployment and, after the procedure, double antiplatelet regimen with clopidogrel and aspirin. Complete proximal and distal recanalization was obtained in 75.3 % of patients; hemorrhagic complications were recorded in 10.4 % of the subjects, while the mortality rate of this series was 24.6 %. A favorable clinical outcome was recorded in 41.6 % of patients. Authors stated that the reopening of the cervical carotid allows immediate intracranial revascularization and a better positioning of the guiding catheter. At the same time, the stent deployed at the level of the proximal stenosis jails the thrombus, reducing the risk of distal embolization. By the way the authors state that this approach could require prolonged time for stent placement and that the dual antiplatelet therapy could result in hemorrhagic transformation especially in patients with a large stroke extension or ineffective intracranial clot removal. The authors suggest that a tapered stand-alone cervical stenosis angioplasty could reduce the risk of hemorrhagic complications.
Srinivasan et al. [26] reported a series of seven patients presenting with tandem occlusion strokes. In five out of seven cases, the proximal occlusion was due to thrombosis developed on an atherosclerotic plaque. In the other two cases the proximal occlusion was due to a dissection and to the consequences of an endoartherectomy. Six patients presented a concomitant M1 occlusion. Complete recanalization was obtained in all cases of M1 occlusion by “in situ” rt-PA injection performed through a micro-catheter navigated within the cervical occlusion. Management of the proximal occlusion varied depending on the type of underlying cause. Patients with cervical atherosclerotic plaque received angioplasty and stenting. In the case of cervical dissection, the artery was treated by deploying two covered stents along the dissected segment. Four out of six patients of this cohort showed a good clinical outcome at 1-month follow-up examination. The authors claim that in tandem occlusion stroke, the first target to be treated should be the intracranial occlusion because it is the cause of the neurological symptoms. They agree with such aptitude because in their opinion, the first purpose of the endovascular approach to tandem occlusions should be the prompt and complete recanalization of the intracranial vessel [27–30]. The first approach to the cervical carotid is performed in order to navigate the guiding catheter above the proximal occlusion. Thereafter, the intracranial occlusion is treated by using clot retriever device. Finally, the carotid cervical occlusion/stenosis is treated by medical management, stand-alone angioplasty, or angioplasty and stenting. Acute stenting is performed in cases of dissection, without collateral supply, or unstable, occlusive atherosclerotic plaque. In such instance, patient is given intravenous aspirin (250–500 mg) just upon stent placement. Stand-alone angioplasty seems to be the best approach in cases of nonocclusive thrombus. The stenting of the cervical carotid or the surgical treatment is in this case performed a few days (10–15) after the acute phase. This staged approach may reduce the risk of hemorrhagic transformation and leads to a better antiplatelet preparation of the patient.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree