Ergonomic Practices for Abdominal Imaging
Susan Raatz Stephenson
|
OBJECTIVES
Recognize factors, both professional and personal, that increase the risk of developing musculoskeletal disorders (MSKDs).
Classify symptoms of MSKD into three categories.
Adapt the environment to reduce MSKD.
Discuss correct and incorrect postures.
Demonstrate exercises and stretches that aid in reducing repetitive stress injuries.
KEY TERMS
abduction
ergonomics
extension
flexion
hyperextension
musculoskeletal disorders (MSKDs)
neutral position
repetitive stress injury
workstation
GLOSSARY
abduction moving away from the center of the body
ergonomics the creation of a safe workplace that involves the sonographer and ultrasound system positioning
extension a position that increases the angle of a joint (e.g., the unbending of the elbow, straightening of the spine)
flexion the decrease of an angle of a joint (i.e., bending of the elbow, curling of the spine)
hyperextension movement beyond the normal range of a joint
neutral position body position without flexion or extension
posture the position of the body
repetition repeated movements. When coupled with force and awkward body positions, repetition increases the risk of musculoskeletal disorders
repetitive stress injury cumulative injury because of repeated movement of a musculoskeletal structure
risk factor any behavior that increases the chances of developing musculoskeletal disorders
static posture fixed or unchanging position
workstation work area encompassing the equipment (i.e., ultrasound system, patient bed)
Musculoskeletal disorders (MSKDs)—injury to the muscles, nerves, ligaments, and tendons—result in a decrease in the ability to participate in both daily and work activities. Though often thought to be the result of work tasks, personal habits and life events change the risk. These include life changes such as pregnancy,1 results of aging and disease treatment (i.e., use of statins),2 and injury because of life activities (i.e., softball).
Work-related musculoskeletal disorders (WRMSKDs) occur in over half of working adults over 18 years, with the costs increasing with medical care, lost wages, and legal fees. A reduction in the accompanying symptoms can be anticipated upon retirement (>65 years); however, 40% of the time, problems continue.3 Most medical professionals report working in pain because of the varied risk factors, resulting in the development of WRMSKDs.3, 4, 5, 6, 7, 8, 9 and 10 Sonographers
seldom anticipate that helping diagnose and ease patient suffering could lead to their own. Clinicians using an ultrasound system have indicated that the shoulder is the most common location for pain, closely followed by the lower back and wrist.11,12 Table 3-1 provides a comparison of MSKDs for various medical professions, and Table 3-2 summarizes the days of work lost by sonographers because of varied symptoms.
seldom anticipate that helping diagnose and ease patient suffering could lead to their own. Clinicians using an ultrasound system have indicated that the shoulder is the most common location for pain, closely followed by the lower back and wrist.11,12 Table 3-1 provides a comparison of MSKDs for various medical professions, and Table 3-2 summarizes the days of work lost by sonographers because of varied symptoms.
PHYSICAL RISK FACTORS FOR WORK-RELATED MUSCULOSKELETAL DISORDERS
The reasons for the development of WRMSKDs are as varied as the person with complaints. Any movement or task creating an imbalance between a person and their environment describes a risk factor.13 Usually associated with the work environment, many activities outside of work also contribute to MSKDs, thus adding to the cumulative injuries.
WRMSKD development depends on multiple factors, but there are key factors contributing to musculoskeletal problems. In this chapter, the focus is on work tasks that increase the risk of developing WRMSKD in sonographers. To begin, attention is paid to activities that increase risks:
Force is the work needed to grasp, lift, or move an item. Examples include the tightness of grasp on the transducer or effort needed to hold and use a biopsy needle.
Vibration refers to repeated, fast movement in any direction. Imaging systems vibrate while being pushed (force) during portable exams and some mechanical 3D transducers also vibrate.
Sustained body positions are those that move out of a neutral position, thus fatiguing muscles and joints. When scanning a patient with the arm behind the body or with a head moved away from the central axis, the body placement is in a non-neutral position.
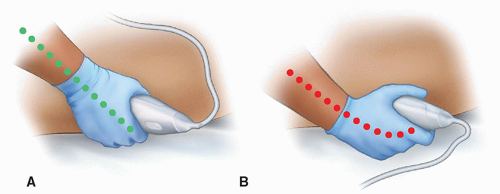
Contact pressure of a body part against hard or sharp edges—for example, when the ventral wrist is placed on the desk while completing patient exams, the risk for developing carpal tunnel syndrome increases.
Frequent repetitive movements using the same muscle groups or joints describe a repeated movement. This often occurs when a mouse is used to complete the tasks.
Temperature is a final consideration because muscles that are cold have the potential to fail sooner than those used after a warm-up session.
TABLE 3-1 Percentage of Medical Professionals Working with Pain | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
TABLE 3-2 Nonfatal Occupational Injuries and Illnesses Resulting in Days Away from Work, by Nature of Injury, Private Industry, 2011 | ||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||||
The focus on WRMSKDs often falls on the physical risk factors, the interaction of stressors, and social setting. In the work environment, the inability to change task demands also increases the risks. These include the following:
Lack of control over job tasks
Increased production demands
Communication failures
Missing task variety resulting in boredom
Lack of management support
Job insecurity
CUMULATIVE MUSCULOSKELETAL DISORDER SIGNS AND SYMPTOMS
MSKDs are the result of accumulated trauma over a prolonged time; however, human bodies provide warning signs related to the severity of the injuries. Repeated exposure to a task reduces the body’s ability to recover and repair itself. As a result, an injury is often not recognized or the cause of the symptoms is unable to be identified. The duration, signs, and symptoms provide clues to whether the pain is due to early-, intermediate-, or late-stage injuries.
An early-stage injury presents with aching, fatigue, stiffness, or discomfort in a muscle or joint. For example, the back or hand may ache; however, stretching and rest will resolve the symptoms. There will be no reduction in the ability to complete work or personal tasks. In essence,
the work a body does is being balanced with contracting stretches, exercises, and rest.
the work a body does is being balanced with contracting stretches, exercises, and rest.
As an injury progresses to the intermediate stage, pain is accompanied by the early-stage symptoms of aching and fatigue. In the event of a work injury, symptoms continue outside of the working environment and the advantages of structured stretching decrease. At this stage, the MSK injury begins to restrict activities, bringing lives out of “balance” even with stretching and rest. Commonly, pain disturbs sleep, and repetitive tasks—such as sewing, typing, and playing an instrument—become difficult.
Chronic injury adds another symptom, weakness or dropping of objects. At this stage, sleeping becomes difficult because of persistent pain. The work-life balance has become weighted toward the symptoms of pain, tiredness, aching, and weakness, with stretching, rest, and exercise having little effect. At this stage, work and personal life are restricted, with the possibility of surgery, physical therapy, and medication as the only methods of relief. Failure of treatment methods to help may result in disability.14 MSKD may progress through these stages, and everyone has a different development of symptoms—highlighting the importance of reporting symptoms.
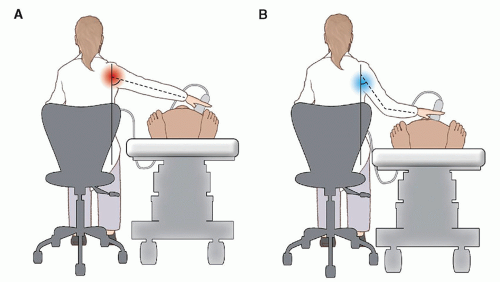
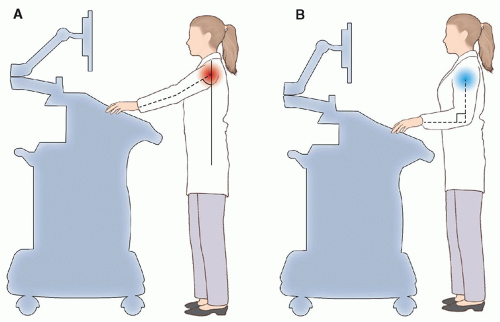
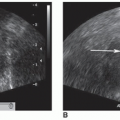
UNDERSTANDING NEUTRAL BODY ALIGNMENT
Maintaining awkward body positions is one of the greatest risk factors encountered by scanning clinicians. The requirement for repeated, static contraction of muscles results in early fatigue, muscle integrity changes, circulation reductions, and buildup of metabolic waste. In preparing for exams, a neutral spine and arm position, decreased reach, and organization of work tools should be ensured (i.e., gel bottle and ultrasound system) (Figs. 3-1 and 3-2).
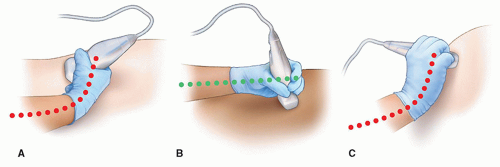
The Neutral Wrist
No Pinch Zone
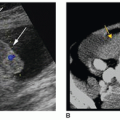
One of the tools used during ultrasound exams is the transducer that is transmits and receives the ultrasound signals. Used during each exam, awareness should be on the grip because the amount of force used may determine the development of MSK injuries to the upper extremity.11,16 The global increase in patient obesity has led to the use of increasing axial force to acquire images.11,16 Repetitive stress injuries any time similar muscle groups are used repeatedly, with wrist stress increasing the risk of developing carpal tunnel syndrome and de Quervain syndrome (Fig. 3-5).17 Table 3-3 lists WRMSKDs of the upper body.
FITTING THE WORKSTATION
The evolution of the ultrasound system has allowed for a decrease in the size and weight of not only the system but also the transducers. Even with lighter equipment, a suboptimal room setup decreases the benefits of the workstation. It is well worth the extra time to set up the tools before beginning the exam.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree