Confirmation of the presence of an intrauterine pregnancy
Evaluation of a suspected ectopic pregnancy
Defining the cause of vaginal bleeding
Evaluation of pelvic pain
Estimation of gestational (menstrual) age
Diagnosis or evaluation of multiple gestations
Confirmation of cardiac activity
Imaging as an adjunct to chorionic villus sampling, embryo transfer, and localization and removal of an intrauterine device
Assessing for certain fetal anomalies, such as anencephaly, in high-risk patients
Evaluation of maternal pelvic masses and/or uterine abnormalities
Measuring the nuchal translucency (NT) when part of a screening program for fetal aneuploidy
Evaluation of a suspected hydatidiform mole
Timing of First-Trimester Ultrasound
The first trimester is defined as a gestational age of up to 13 6/7 menstrual weeks of gestation. The embryonic period encompasses the first 10 menstrual weeks, and some guidelines state that the term “embryo” should be used before 10 weeks and “fetus” thereafter. For some indications and purposes, the timing of the ultrasound requires more specific limits. For example, aneuploidy screening and evaluation of fetal gross anatomy should be performed between 11 and 13 6/7 weeks of gestation, and pregnancy dating is more accurate earlier in the first trimester [5, 13].
Content of the Examination
Components of a standard first-trimester examination are assessment of pregnancy location, fetal number, fetal viability, measurements, determination of gestational age, and assessment of other intrauterine and extrauterine structures. Assessment of fetal anatomy and fetal aneuploidy assessment may be appropriate for some patients.
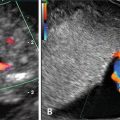
Pregnancy Location
The location of the pregnancy should be determined and documented. A definitive diagnosis of intrauterine pregnancy can be made when an intrauterine gestational sac containing a yolk sac or embryo/fetus with cardiac activity is visualized. Follow-up sonography and/or serial determination of maternal serum human chorionic gonadotropin levels are appropriate in pregnancies of undetermined location (see also Chap. 10) [1].
Fetal Number
Although the visualization of multiple sacs early in the first trimester is suspicious, the diagnosis of a multiple pregnancy requires visualization of multiple embryos/fetuses. The first trimester is the optimum time to determine chorionicity and amnionicity, which are critical for management of multi-fetal pregnancies. The presence of separate sacs, the thickness of the intervening membrane, and the shape of its junction with the placenta should be assessed [2] (Fig. 6.1). Early in the first trimester, an intervening amnion may not be visible in diamniotic–monochorionic twins [2]. Amnionicity and chorionicity should be stated in the ultrasound report.
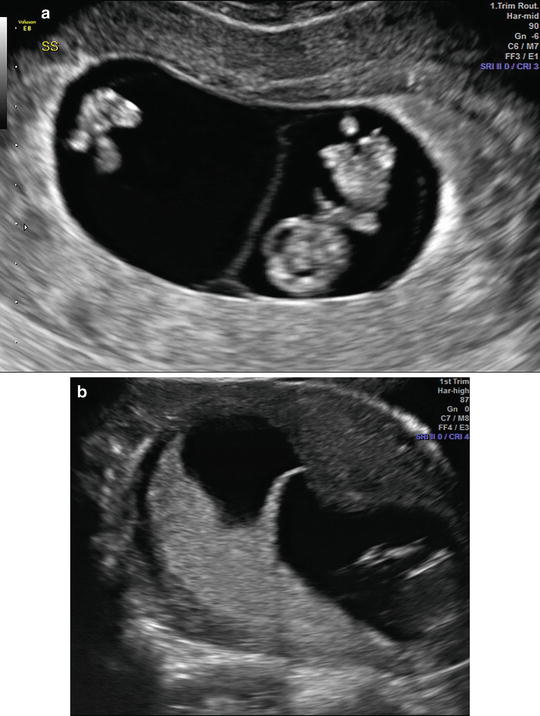
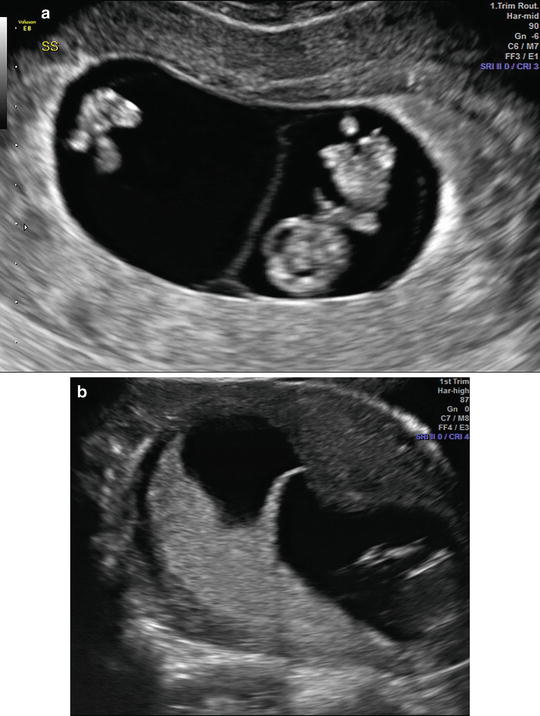
Fig. 6.1
(a) Monochorionic twin pregnancy at 9 weeks of gestation. Note the thin intervening membrane with no placental tissue. (b) Dichorionic twin pregnancy at 12 weeks of gestation. Note the thick intervening membrane with placental tissue (“twin peak” sign)
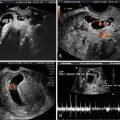
Assessment of Viability
Although the term “viability” implies the ability to live independently outside of the uterus, from an ultrasound perspective, the term is used to describe the presence of an embryo with cardiac activity at the time of the examination [5]. An alternative definition, proposed by the SRU, is a pregnancy that can potentially result in a liveborn baby. Updated diagnostic criteria for pregnancy viability have recently been published by the SRU due to occurrences of women diagnosed with miscarriage or ectopic pregnancy that resulted in damaging interventions to potentially normal pregnancies [10]. Findings diagnostic of pregnancy failure using transvaginal ultrasound include a crown-rump length (CRL) of ≥7 mm and no heartbeat, mean sac diameter (MSD) of ≥25 mm and no embryo, absence of an embryo with a heartbeat ≥2 weeks after a scan that showed a gestational sac without a yolk sac, and absence of an embryo with a heartbeat ≥11 days after a scan that showed a gestational sac with a yolk sac. Findings suspicious for, but not diagnostic of, pregnancy failure using transvaginal ultrasound include a CRL of <7 mm and no heartbeat, MSD of 16–24 mm and no embryo, absence of an embryo with a heartbeat 7–13 days after a scan that showed a gestational sac without a yolk sac, absence of an embryo with a heartbeat 7–10 days after a scan that showed a gestational sac with a yolk sac, absence of an embryo ≥6weeks after LMP, empty amnion (amnion seen adjacent to yolk sac, with no visible embryo), enlarged yolk sac (>7 mm), and a small gestational sac in relation to the size of the embryo (<5 mm difference between MSD and CRL). This group has also proposed that specific terminology be used, as summarized in Table 6.2.
Table 6.2
Terminology used early in the first trimester of pregnancya
Terminology | Comments |
|---|---|
Viable | A pregnancy is viable if it can potentially result in a liveborn baby |
Nonviable | A pregnancy is nonviable if it cannot possibly result in a liveborn baby. Ectopic pregnancies and failed intrauterine pregnancies are nonviable |
Intrauterine pregnancy of uncertain viability | A woman is considered to have an intrauterine pregnancy of uncertain viability if transvaginal ultrasonography shows an intrauterine gestational sac with no embryonic heartbeat (and no findings of definite pregnancy failure) |
Pregnancy of unknown location | A woman is considered to have a pregnancy of unknown location if she has a positive urine or serum pregnancy test and no intrauterine or ectopic pregnancy is seen on transvaginal ultrasonography |
Early Pregnancy Measurements
The MSD and CRL should routinely be measured and reported. The MSD is the average of three orthogonal measurements of the fluid filled space within the gestational sac (Fig. 6.2). The CRL is the maximum length of the entire embryo or fetus measured as a straight line in a true midsagittal plane (Fig. 6.3). Later in the first trimester, care should be taken to ensure that the fetus is not flexed by looking for the presence of fluid between the fetal chin and chest (Fig. 6.4). The ISUOG guidelines state that the biparietal diameter (BPD) and head circumference (HC) may also be measured after 10 weeks of gestation [5].
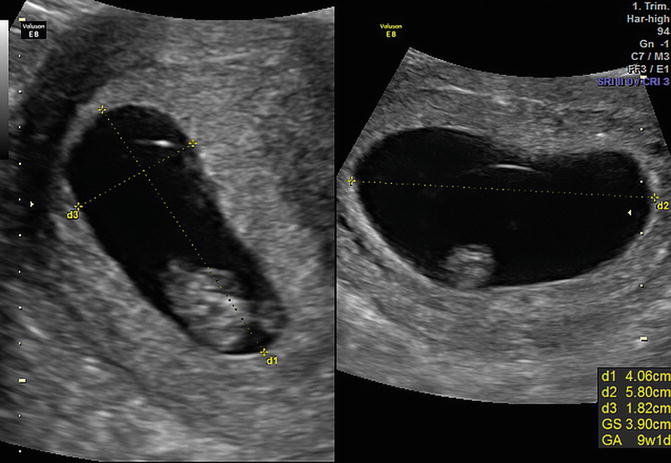
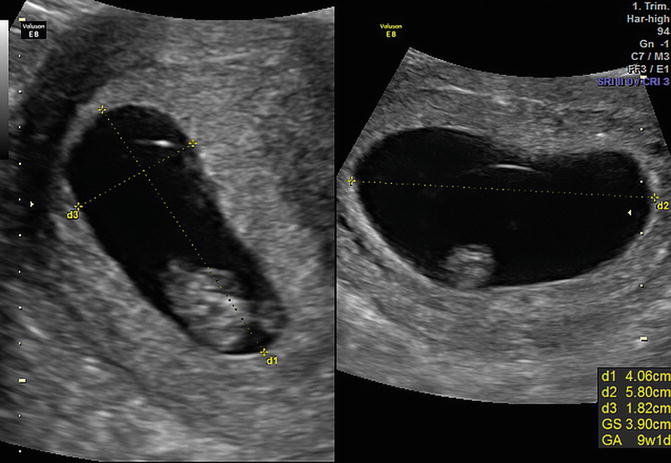
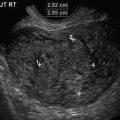
Fig. 6.2
Measurement of the mean gestational sac diameter in three orthogonal planes at 9 weeks of gestation