© Springer International Publishing Switerzland 2016
Carsten Nieder and Johannes Langendijk (eds.)Re-Irradiation: New FrontiersMedical Radiology10.1007/174_2016_77Re-irradiation for Esophageal Cancer
(1)
Department of Radiation Oncology, S. Camillo and Forlanini Hospitals, Rome, Italy
Abstract
While recurrent esophageal cancer is a common clinical scenario, limited data exist regarding management approaches that include re-irradiation. Tremendous technological advances in the treatment planning and delivery of radiotherapy pave the way to evaluate the appropriateness of re-irradiation in the management of radio-recurrent esophageal cancer. Patients with radio-recurrent esophageal cancer may still be selected for a potentially curative treatment, especially those in good clinical condition, who may experience prolonged survival and good symptom control rates. None of the different therapeutic options is carried out without potentially life-threatening treatment-related toxicities in a relevant proportion of the patients. In this scenario, patient selection performed on individual basis could help to identify the most appropriate treatment modality, including re-irradiation with cutting-edge techniques. Enrollment of these patients in clinical trials is highly warranted.
The original version of this chapter was revised. An erratum to this chapter can be found at 10.1007/978-3-319-41825-4_78.
1 Introduction
Locoregional recurrence is still the major type of treatment failure in patients with esophageal cancer after definitive radiotherapy (RT) or radio-chemotherapy (RCT). The recurrence rate after radical RT, RCT, and surgery is more than 70 % (Fujita et al. 1994; Stahl et al. 2005) with in-field relapse after RCT in more than 20 % of patients (Haefner et al. 2015; Ordu et al. 2015). Once recurrence occurs, the 5-year survival rate drops dramatically down (Yano et al. 2006; Shioyama et al. 2007). Current NCCN guidelines recommend palliative/best supportive care (BSC) in this setting (NCCN guidelines Version 2.2016). Due to its disappointing outcomes, chemotherapy has only a palliative role and it is associated to a median survival of 5 months (Sudo et al. 2014). Salvage surgical resection can result in favorable local control (95 %) and overall survival (up to 59 months), but is hampered by high rates of anastomotic leakage (17–39 %), pulmonary complications (17–30 %), intensive care unit readmission (17–22 %), and postoperative mortality (3–15 %) (Swisher et al. 2002; Marks et al. 2012, 2014; Sudo et al. 2013, 2014), which makes this choice highly demanding and limited to a carefully selected patient population (Marks et al. 2012).
2 Re-irradiation
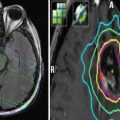
Salvage re-irradiation largely depends on the location of local failure in relation to the prior radiation field, but it is often discouraged because it infringes the basic, long-standing principle that once definitive RT has been administered, further RT cannot be given because it would likely exceed normal tissue tolerances. Indeed, with external beam radiation therapy (EBRT), it is often difficult to avoid organs that already have received tolerance doses of radiation with the primary treatment. Although re-irradiation has been proven to be feasible and effective in other tumors (Zwicker et al. 2011; Zerini et al. 2015), the advantage of this approach in the management of local tumor bed recurrence after definitive RCT remains uncertain. Advances in the treatment planning and delivery of RT have aroused interest in assessing the appropriateness of re-irradiation for various anatomical sites (Mantel et al. 2013). However, experiences with advanced forms of radiotherapy – intensity-modulated radiation therapy (IMRT) and stereotactic body radiotherapy (SBRT) – are sparse and limited to case reports, while only few studies have been published on salvage re-irradiation for locoregional recurrence after primary radical RCT (Yamaguchi et al. 2011; Kim et al. 2012; Zhou et al. 2015). Yamaguchi et al. (2011) reported on 31 patients with recurrent or persistent squamous cell carcinoma of the esophagus treated with re-irradiation to a dose of 36–40 Gy in 2-Gy fractions using 3-dimensional conformal RT. Among them, 27 patients received concurrent chemotherapy, and 14 patients underwent regional hyperthermia during the re-irradiation course. Despite the lower radiation doses used, severe toxicities were not uncommon, with 6 patients (20 %) who suffered from grade 3 esophageal perforation. Zhou et al. (2015) reported on the largest studied cohort retrospectively analyzing a total of 114 patients with locally recurrent esophageal squamous cell carcinoma after initial radical RCT. Fifty-five patients underwent salvage RT with a median dose of 54 Gy (range 18–66 Gy), 1.8–2.0 Gy per fraction, 5 days/week, and 59 patients received BSC only. After a median follow-up period of 20 months (range 8–70 months), those who received the active treatment reported a 6-month and 1-year survival rate after recurrence of 41.8 % and 16.4 %, respectively. The same features in the non-salvage cohort were 11.9 % and 3.4 %, respectively (p < 0.001). However, treatment-related toxicity was relevant, with 3 (5.5 %) and 11 (20.0 %) patients from the active group who experienced ≥ grade 3 radiation pneumonitis and esophageal fistula/perforation, respectively, compared to none and 8 patients (13.6 %) from the BSC group. At multivariate analysis, a salvage radiation dose >50 Gy and late recurrence (>12 months) were associated with a better prognosis. Due to its intrinsic dose distribution, brachytherapy (BT) may be considered in place of EBRT to restore the integrity of the lumen by the use of appropriate applicators which can decrease an excessive dose deposition on mucosal surfaces (Harms et al. 2005). Nevertheless, also salvage BT is carried out with significant risk of severe (grade ≥ 3) toxicities, mainly consisting in perforation, hemorrhage, and fistula formation, observed in up to 30 % of the patients (Homs et al. 2004). A further option in this patient population is represented by proton therapy (PT), which may offer an advantage over photon therapy, as the proton beam deposits most of its energy at a specific depth, so the radiation dose beyond that target is negligible. Fernandes et al. (2016) reported on a series of 14 patients with a history of thoracic radiation and newly diagnosed or locally recurrent esophageal cancer who were offered proton beam re-irradiation on a prospective trial. The median re-irradiation prescription dose was 54.0 Gy (relative biological effectiveness [RBE]) (50.4–61.2 Gy [RBE]), and the median interval between radiation courses was 32 months (10–307 months). Eleven patients received concurrent chemotherapy. After a median follow-up of 10 months (2–25 months), the median overall survival was 14 months and among the 10 patients who presented with symptomatic disease, 4 had complete resolution of symptoms, and 4 had diminished or stable symptoms. Late grade 3 toxicities and late grade 5 esophageal ulcer occurred in four and one patients, respectively. Although the differential diagnosis between tumor progression and late adverse reactions appears difficult, it is undeniable that treatment-related toxicities may occur in spite of the use of such advanced forms of RT.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree