Fig. 21.1
Value of PET-CT in diagnosis. (a) Intense 18F-FDG activity in both tonsils, more on the right side, in a patient who was initially thought to have tonsillar carcinoma. (b) 18F-FDG avidity is seen also in multiple cervical, axillary, and inguinal nodes suggesting this is more likely to be lymphoma. This was proven on lymph node biopsy
Cancers of salivary gland origin such as adenoid cystic carcinoma and mucoepidermoid carcinoma account for about 1 % of all H&N cancers. They may present as a painless hard mass in the salivary glands. Unless there is facial nerve palsy and enlarged lymph nodes that may suggest malignancy, differentiation between benign and malignant disease is not possible by clinical examination alone. Due to the presence of between 500 and 1,000 minor salivary glands in the palate, oral cavity, nose, paranasal sinuses, larynx, and hypopharynx, salivary gland cancers may also manifest in the mucosa of the upper aerodigestive tract as an aggressive-looking mass that is indistinguishable from SCC on clinical and imaging evaluation.
Olfactory neuroblastoma, plasmacytoma, chondrosarcoma, chordoma, and melanoma are encountered on rare occasions.
Imaging helps in the staging of cancer so that appropriate therapeutic decisions can be made for the patient. It is also used for the follow-up of the patient following treatment. In those who have been cured of cancer, imaging is performed at longer intervals for surveillance.
21.2 Choice of Imaging Modality and Technique
For imaging to be beneficial, one must be aware of the advantages and disadvantages of the available imaging options in the light of the specific clinical problem. The decision is best made on joint consultation between the clinician and the radiologist. It is dictated by the location of the lesion, the patient’s general condition, and cost.
The appropriate choice of scan parameters is important. However, no CT or MRI protocol is robust enough to be employed successfully in every patient. It is important that we understand the clinical problem that we have to address. When there is insufficient clinical information, it would be extremely helpful for the attending radiologist or the radiographer to talk to the patient and make a quick visual inspection. Some superficial tumors, especially oral cancers, although obvious on visual inspection, cannot be seen on imaging, and a cursory clinical examination would save us hours of agony later on when reading the study.
Imaging is useful in showing the deep extent of tumor (Fig. 21.2a, b), particularly in areas that are hidden from clinical examination, e.g., skull base, parapharyngeal space, paraglottic space, and retropharyngeal space. Imaging is also useful for the detection of nodal disease in the neck, particularly in the obese and in the difficult-to-examine posttreatment neck. Most scans of the H&N are done with quiet breathing with occasional special maneuvers like the puff-cheek technique (Fig. 21.3a, b) or the open-mouth technique. It is best for the radiographer to spend a few seconds rehearsing these maneuvers with the patient prior to the scan.
Fig. 21.2
Role of imaging in neoplastic disease. (a) Clinical finding of oral cancer in the left mandibular alveolus and floor of mouth. (b) Axial CT image shows the deep extent of tumor and frank erosion of the mandible
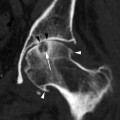
Fig. 21.3
Carcinoma of the alveolar ridge. (a) Axial CT image with the puff-cheek technique shows the tumor (white arrows) in the anterior maxillary alveolus outlined by air. (b) Coronal CT image shows tumor (white arrow) eroding the palate
The commonest cause of motion artifacts is swallowing during the scan. Swallowing motion may result in spurious diagnosis of a pharyngeal mass (Fig. 21.4a, b). They can be recognized by their accompanying streak artifacts. Care must be taken to avoid swallowing. This is best done by asking the patient to swallow multiple times prior to the start of the scan acquisition. Elderly patients with physical impairment may face difficulty undergoing the examination and care should be taken to ensure they are comfortable during the time of scanning. Apart from fragile veins and easy bruising that necessitate the use of the scan pad, there is also the higher incidence of renal impairment in the elderly which may limit the use of contrast medium. However, unless absolutely contraindicated, it is better to do the imaging study using a contrast agent in order to get a good quality diagnostic examination. For the cancer patient, a nondiagnostic study may be more detrimental than the perceived risks associated with the examination.
Fig. 21.4
Artifacts from swallowing motion on axial CT images. (a) Contraction of the nasopharynx during swallowing mimics a mass. Note the streak artifact (white arrow) in the nasopharyngeal wall indicating that this is due to motion. (b) Repeat scan on the same day shows the nasopharynx to be normal
21.2.1 Computed Tomography
The complex anatomy of the H&N region calls for evaluation by cross-sectional imaging. A contrast-enhanced CT examination from the skull base to the clavicles is a useful test for diagnosis, staging, and follow-up of head and neck cancers. The inclusion of the skull base is important for the detection of perineural spread along cranial nerves. CT is fast and it shows good anatomical detail through multiplanar reconstructions, allowing for the detection of the tumor beyond what is seen on clinical examination. Deep lesions of the H&N that are beyond the reach of ultrasound scanning can be biopsied under CT guidance (Fig. 21.5). CT is also used routinely in radiotherapy planning.
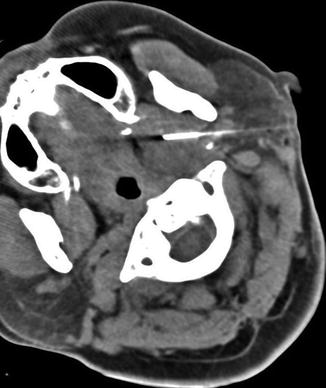
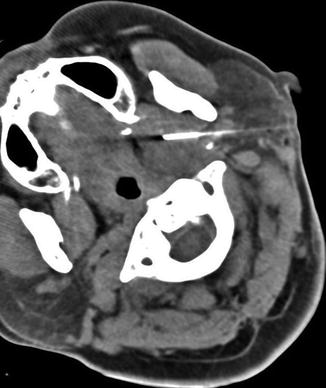
Fig. 21.5
CT-guided core biopsy of a parapharyngeal mass via a retromandibular approach
21.2.1.1 CT Technique
Intravenous iodinated contrast agent using a multislice CT scanner.
Special maneuvers like puff cheek or open mouth, when necessary.
Axial and coronal reconstructions with 5 mm sections are routinely performed. Sagittal reconstructions for midline skull base or base of tongue lesions.
Additional 2.5 mm thin section reconstructions for small lesions and for the assessment of laryngeal cancers.
Artifacts from dental amalgam may preclude imaging evaluation of tongue cancers but this can be overcome by repeat scan over the tongue with the mouth open. The puff-cheek technique is helpful in showing buccal-gingival lesions (Fig. 21.3a, b).
21.2.2 Magnetic Resonance Imaging
In the H&N region, MRI allows for more accurate delineation of tumor from normal soft tissue. It also allows separation of tumor from secretions in the paranasal sinuses (Fig. 21.6a, b). The better contrast resolution allows for the better detection of perineural spread which confers poorer outcome. Until recently, it was generally accepted that CT was superior to MRI in demonstrating skull base involvement, while MRI was better in delineating soft tissue abnormality. It is now known that MRI is more sensitive than CT in identifying skull base involvement (Fig. 21.7a, b). Bones forming the skull base (clivus and petrous apex) contain marrow. Although cortical erosion is more confidently diagnosed on CT, infiltration of the marrow spaces is better delineated on MRI (Chong et al. 2002a). CT often underestimates the frequency and extent of skull base involvement.

Fig. 21.6
Maxillary sinus SCC. (a) IV contrast-enhanced coronal CT image shows a large mass (asterisk) in the medial left maxilla causing obstruction and expansion of the left maxillary sinus. It is unclear whether the tumor has reached the anterior skull base (arrow). (b) Coronal T2-weighted MRI shows the tumor (asterisk) outlined by high-intensity fluid in the left ethmoid and maxillary sinuses. It has not reached the anterior skull base (arrow)

Fig. 21.7
Radiation-induced sarcoma of the skull base: assessment of bone by MRI. (a) CT shows soft tissue mass with bone destruction in the right body of the sphenoid and intracranial extension (white arrow). (b) Gadolinium-enhanced coronal fat-saturated T1-weighted MRI shows the extent of marrow involvement (white arrow) beyond what is shown on CT
Recently, new MRI techniques such as dynamic contrast-enhanced MRI, diffusion-weighted MRI, and proton MR spectroscopy have shown promising results in the differentiation of benign and malignant tumors of the salivary gland. Diffusion-weighted MRI is helpful in the evaluation of intracranial and skull base lesions, allowing for detection of acute brain infarcts, for differentiation between arachnoid cyst and epidermoid in the middle cranial fossa, and for differentiation between abscess and tumor in the brain. In evaluation of H&N tumors, the apparent diffusion coefficient as the quantitative parameter of diffusion-weighted imaging has been found to be significantly smaller in lymphomas than in carcinomas. At present, MR spectroscopy and diffusion-weighted imaging are research tools for the H&N region. They are not routinely used in clinical practice.
There is growing interest in using whole-body MRI for both the staging and follow-up evaluation of pediatric and young adult cancer patients so as to avoid the radiation risk from repeated CT examinations. Whole-body MRI is less helpful for the elderly patients as the examination time is long, often between 60 and 90 min. Some of the routine H&N MRI scans can pose a challenge for the elderly patients, in particular those with swallowing difficulty. The pooling of saliva in the pharynx causes much discomfort leading to motion artifacts. These patients will benefit more from a CT examination. MRI is increasingly used in radiotherapy planning due to the need for accurate delineation of the tumor margin for 3D conformal radiotherapy and intensity-modulated radiotherapy. The MRIs obtained in the treatment position with a dedicated flat table and a dedicated H&N coil are fused with the treatment-planning CT images.
21.2.2.1 MRI Technique
Routine axial and coronal scans using a dedicated H&N coil. Sagittal sequences are used for the midline skull base or base of tongue lesions.
Sequences.
T1-weighted spin echo.
T2-weighted spin echo with fat saturation.
Gadolinium-enhanced T1-weighted spin echo with fat saturation.
The uneven contour of the neck contributes to field inhomogeneity and uneven fat saturation in the supraclavicular fossa with the fast spin-echo technique. This is only a minor setback as the supraclavicular is easily assessed by clinical examination and there are the non-fat-saturated T1-weighted images available for reading. The Dixon technique may help overcome some of the inhomogeneity.
21.2.3 Positron-Emission Tomography-CT
PET became available in the early 1990s, and it provided significant improvements to cancer care by showing metabolically active tumor (Fig. 21.6a, b). However, as the images were two-dimensional, there was difficulty in localizing the tumor. With PET-CT, we are able to get functional information of glucose metabolism as well as accurate anatomical information from CT. The 18F-FDG uptake has been reported to correlate well with tumor grade. However, it is costly and therefore should be used selectively.
For local staging of the primary tumor, there is no advantage over CT or MRI when the primary tumor was already seen by CT or MRI. Moreover, the CT images from a PET-CT study are not of diagnostic quality as they are performed using a low-dose CT technique. Images of the lung are often of poor quality as they are done without breath hold. PET-CT is most useful in locating the unknown primary. It is also superior to CT alone for detection of metastatic disease allowing for more accurate staging of cancer. PET-CT is particularly helpful in evaluating the posttreatment neck for tumor recurrence, as most studies showed improved detection of recurrence by PET-CT (Lowe et al. 2000). PET-CT may also be used with CT and MRI for radiotherapy planning.
21.2.3.1 PET-CT Technique
Patients fast for at least 6 h prior to intravenous injection of 18F-FDG. Serum glucose level should be <120 mg/dL prior to injection. Whole-body scanning is performed after an interval of at least 60 min following the injection. PET-CT images are presented at 3–5 mm slice thickness for viewing.
21.2.4 Ultrasonography
Many of the H&N lesions are superficial and they can be seen on ultrasound using a high-frequency probe. It is particularly useful for evaluating thyroid nodules, neck nodes, and the parotid and submandibular glands. The ability to show the image in real time allows for quick and accurate guidance of needle biopsy procedures in the neck. Cervical lymph nodes and parotid masses can be sampled with fine needle aspiration (FNA) for cytology. Excisional or incisional biopsy of cancer may compromise ideal treatment strategies, and therefore, FNA is preferred in most cases. However, if there is suspicion of lymphoma, a larger tissue sample is required for proper characterization, and a core biopsy can be performed.
Due to the limited coverage of the ultrasound examination and its inability to show the deep tissue spaces, its utility in the staging and follow-up imaging of H&N cancer is limited. However, it is inexpensive compared to CT or MRI, and it may be a useful tool for the evaluation of the neck in resource-poor countries.
21.2.5 Radiography
Radiographs such as dental radiographs and orthopantomograms have limited roles in the evaluation of the alveolus and the mandible. CT is preferred as it provides greater soft tissue detail and greater coverage for staging assessment.
21.3 Anatomy and Diagnosis of Benign and Malignant Neoplasia
In evaluating the H&N by imaging, the primary role of a radiologist is to assess disease extent and not to make a histological diagnosis. As there is overlap in the imaging appearance of benign and malignant masses, there is often the need for a biopsy to establish the diagnosis. However, one should be able to recognize normal variations in anatomy and some benign conditions so that we can avert an unnecessary biopsy whenever possible. Knowledge of staging according to the American Joint Committee on Cancer (AJCC) (Edge et al. 2010) is important so that the pertinent findings are communicated. T staging (staging of the primary site) is dependent on the size of the lesion and spread to adjacent structures. N staging (nodal staging) is based on the size, number, and location of metastatic lymph nodes. For M staging (metastasis), common sites of metastasis from H&N cancer are in the lungs, liver, and bone. Radiologists should also be familiar with clinical pathways for treating H&N cancer according to the National Comprehensive Cancer Network (NCCN) clinical practice guidelines so that we understand the impact of our interpretation of the scans.
21.3.1 Oral and Oropharyngeal Tumors
21.3.1.1 Anatomy of the Oral and Oropharyngeal Area
The oral cavity (Fig. 21.8) comprises the lips, buccal space, the gingiva, tongue, hard palate, and floor of mouth. It is separated from the oropharynx by the anterior tonsillar pillar. The anterior two-thirds of the tongue or the oral tongue is the portion that is anterior to the circumvallate papillae. Within the tongue are intrinsic muscles and four pairs of extrinsic tongue muscles: the genioglossus, hyoglossus, palatoglossus, and styloglossus. The extrinsic muscles provide a pathway for tumor extension from the tongue to its insertion.
Fig. 21.8
MRI shows anatomy of oral cavity and pharynx. The rectangular boxes show the boundary of the oral cavity (OC), nasopharynx (N), oropharynx (O), hypopharynx (H), base of tongue (BOT), and palatine tonsil (asterisk). (a) Sagittal T1-weighted MRI. (b) Axial T1-weighted MRI
The retromolar trigone is a triangular-shaped mucosal space lying posteriorly to the last mandibular molar and anterior to the ascending ramus of the mandible. The floor of mouth lies beneath the oral tongue. It is supported by the mylohyoid muscle sling. Within the floor of mouth are the sublingual glands, the submandibular duct, root of the tongue, and the neurovascular bundle of the tongue. The lingual nerve, hypoglossal nerve, submandibular duct, and lingual vessels run within the neurovascular bundle. It is located in the posterior floor of mouth between the mylohyoid and the hyoglossus muscles.
The oropharynx is the pharyngeal space that spans from the hard palate to the level of the hyoid bone. It includes the posterior third of the tongue, the palatine tonsils, the soft palate, and the uvula. The posterior third is also called the base of tongue. On T2-weighted and T1-weighted gadolinium-enhanced MRI, both the tonsils and the base of tongue show increased intensity compared with the oral tongue. This is due to the presence of lymphoid tissue.
21.3.1.2 Benign Lesions and Pseudomass of the Oral Cavity and Oropharynx
A tortuous carotid artery may be developmental or acquired due to atherosclerotic disease. The artery runs in an unusually medial course causing a pulsatile mass on the oropharyngeal wall (Fig. 21.9a, b). The anomaly is well shown on CT or MRI, sometimes as an incidental finding, and it is good practice to highlight this in the radiology report to alert the unwary clinician who may otherwise be tempted to biopsy the mass.
Fig. 21.9
Pulsatile oropharyngeal mass due to a tortuous internal carotid artery. (a) Coronal T1-weighted MRI shows a tortuous right internal carotid artery with a medial bend (white arrow) towards the pharynx. (b) Gadolinium-enhanced coronal fat-saturated T1-weighted MRI in a more anterior location shows the medial bend of the right internal carotid artery (white arrow) causing a bulge in the oropharyngeal lumen
Torus mandibularis and torus palatinus are bony exostoses arising from the inner cortex of the mandible and hard palate. Patients present clinically with a long-standing history of submucosal bulge in the floor of mouth or palate. On imaging, there is continuity of the exostosis with the cortical bone (Fig. 21.10a, b). Occasionally, a tumor can develop over the mucosa of the torus (Fig. 21.10c).


Fig. 21.10
Torus mandibularis. (a) Axial CT image shows a row of calcified masses in the floor of mouth parallel to the alveolus. (b) Coronal CT image shows these masses to be in continuity with the inner cortex of the mandible (white arrows). (c) Coronal CT image of another patient shows erosion of the left torus palatinus by SCC (white arrow)
Pleomorphic adenoma and Warthin tumor can arise from minor salivary glands in the palate (Fig. 21.11). A detailed discussion is found in the salivary gland section of this chapter. On clinical examination and imaging, there is a smooth submucosal mass in the palate that may be associated with bone thinning in the palate.


Fig. 21.11
Pleomorphic adenoma of the palate. Axial CT image shows a well-defined smooth soft tissue mass in the left half of the palate (white arrows)
Lingual thyroid is a rare developmental anomaly which occurs when there is arrested descent of the thyroid gland, resulting in ectopic thyroid tissue in the tongue at the foramen caecum. Clinically, there is a submucosal midline lump at the border between the oral tongue and the tongue base. The patient is usually euthyroid and asymptomatic but hypothyroidism, bleeding, dysphagia, and neoplasm have been reported. On CT, a lingual thyroid is hyperdense due to the high iodine content of the gland (Fig. 21.12), and there is strong enhancement with intravenous contrast. There is absence of normal thyroid gland in front of the thyroid cartilage. The lesion shows avidity with technetium 99 m.


Fig. 21.12
Lingual thyroid. Non-contrast CT image shows a high-density mass in the foramen caecum due to the high iodine content of thyroid tissue
Hypoglossal nerve palsy produces unilateral atrophy of the tongue on the ipsilateral side. On imaging with CT, the tongue on the affected side may appear enlarged (Fig. 21.13a) with narrowing of the oropharyngeal airway. This is due to the decreased muscle tone. On MRI, there is fat infiltration of the affected half of the tongue (Fig. 21.13b).
Fig. 21.13
Hypoglossal nerve palsy. (a) Axial CT image shows spurious enlargement of the right half of the tongue (white arrow) due to decreased muscle tone. (b) Axial T1-weighted MRI shows the typical fat replacement in the paralyzed right half of the tongue (white arrows)
21.3.1.3 Malignant Lesions of the Oral Cavity and Oropharynx
The strong association with alcohol and tobacco consumption and the higher incidence of SCC in the dependent parts of the oral cavity, i.e., lower lip, oral tongue, and floor of mouth, could be related to prolonged contact with carcinogenic agents in saliva pools in these sites. The incidence of SCC decreases in the posteriorly located oropharynx and hypopharynx. In general, oropharyngeal SCC has a less favorable prognosis as it is usually detected late and there is higher incidence of nodal disease due to the richer lymphatic network there.
Cancer of the oral tongue usually presents with a nonhealing ulcer. Pain and dysarthria are late symptoms.
In the imaging evaluation, look out for:
Extent of tumor, whether it has crossed the midline
Extrinsic muscle involvement (Fig. 21.14a, b) as this is considered T4a disease
Fig. 21.14
SCC of the tongue. (a) Axial T1-weighted MRI shows a small 2 cm tumor in the right lateral tongue but with deep extension (white arrow). (b) Axial T1-weighted MRI at a lower level shows involvement of the hyoglossus, making this a T4a tumor (white arrow). Note the normal left hyoglossus (white arrowhead) and the normal genioglossus (asterisk)
Extension to the floor of mouth
Bone involvement
Cancer of the lip and alveolar ridge may present with a nonhealing ulcer or loosening of tooth or change in the fit of the dentures.
In the imaging evaluation, look out for:
Extent of bone involvement as this will determine the type of mandibulectomy or maxillectomy (Fig. 21.3a, b)
Cancer of the retromolar trigone tends to be detected late as clinical assessment of this area is difficult and is dependent on imaging for management. Within the retromolar trigone, the pterygomandibular raphe provides an important pathway for tumor spread. The pterygomandibular raphe is a fibrous band that runs between the hamulus of the medial pterygoid plate and the medial body of the mandible. Both the buccinator and the superior pharyngeal constrictor muscles are attached to the pterygomandibular raphe.
In the imaging evaluation, look out for:
Extent of the tumor, whether it has reached the pterygopalatine fossa, buccal space, oropharynx, mandible, or floor of mouth
Extent of bone involvement in the mandible, pterygoid plate, and maxilla (Fig. 21.15a, b)

Fig. 21.15
Retromolar trigone SCC. (a) CT image shows tumor eroding the ramus of the mandible (white arrow) with posterior extension to the oropharynx (dotted arrow). (b) CT image taken at a more cranial level shows superior extension of tumor along the pterygomandibular raphe to involve the maxillary tubercle (white arrow)
Cancer of the floor of mouth usually presents with a nonhealing ulcer. This may be preceded by long-standing leukoplakia.
In the imaging evaluation, look out for:
Extent of the tumor, whether it has crossed the midline
Neurovascular bundle involvement (Fig. 21.16a, b)
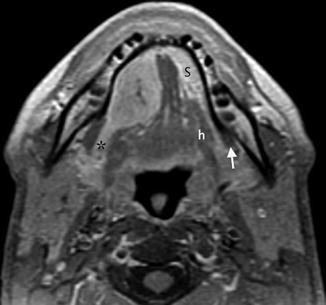
Fig. 21.16
Adenocarcinoma of the sublingual gland. Axial T1-weighted MRI shows the right sublingual gland is enlarged due to tumor and there is posterior extension to the neurovascular bundle of the tongue (asterisk). The normal left submandibular gland (s) and the normal left neurovascular bundle are seen between the mylohyoid (white arrow) and hyoglossus muscles (h)
Mandibular involvement (Fig. 21.2b)
Cancer of the Tonsils
SCC arises most commonly in the anterior tonsillar pillar or from epithelial remnants of the palatine tonsil. They are sometimes occult, presenting with cervical lymph node metastasis. The appearance of a single level II cystic node may fool the inexperienced radiologist into diagnosing a branchial cleft cyst, and this contributes to a delay that may eventually lead to unfavorable outcome for the patient. In the elderly patient, this is far more likely to be nodal metastasis from either cancer of the tonsils or papillary thyroid cancer.
In the imaging evaluation, look out for:
Extension of the tumor along the palatoglossus superiorly to involve the soft palate
Extension of the tumor inferiorly to the tongue base
Extension of the tumor anteriorly into the retromolar trigone and buccal space
Cancer of the Base of Tongue
The base of tongue is also a common site for occult malignancy due to difficulty in performing the clinical examination. Moreover, imaging studies of this area can be hard to interpret as normal lymphoid tissue in the base of tongue (lingual tonsils) can resemble tumor on CT, MRI, or PET-CT. They enhance with intravenous contrast agent and they are hyperintense on T2-weighted MRI. Large and laterally located tumors can be detected based on asymmetry. Conversely small and centrally located tumors of the base of tongue are easily missed on imaging.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree