IABP
TandemHeart™
Impella 2.5®
Mechanism
Pneumatic displacement
Centrifugal flow
Axial flow
Femoral artery access
7–8F
15–17F
13F
Placement time (approx.)
5 min
15 min
30 min
Duration of use
2–5 days
14 days max
6 h max
Additional flow (L/min)
<0.5
4.0–5.0
2.5
Physiologic timing required
Yes
No
No
MAP
↑
↑↑
↑↑
CI
↑
↑↑↑
↑↑
CPO
↑↑
↑
Intra-aortic Balloon Pump
The intra-aortic balloon pump (IABP), initially introduced in the 1960s [23], is the most commonly used mechanical support device and has remained a staple in the interventionalist’s arsenal [24]. IABPs work by increasing coronary blood flow [25]. Diastolic balloon inflation tends to increase antegrade flow (systemic perfusion), as well as retrograde flow (coronary and cerebral perfusion). Systolic deflation results in decreased afterload and decrease in myocardial oxygen demand. While IABPs do tend to decrease myocardial oxygen demand, there is only a minimal increase in cardiac output, estimated to be about 0.5 L/min [26]. Alleviation of myocardial ischemia thus appears to be the principal benefit accrued from IABP insertion. The IABP is dependent on a minimal baseline left ventricular pump function as well as a stable electrical milieu in order to provide hemodynamic support. Cardiogenic shock is the most common reason for the insertion of IABPs, accounting for about 20 % of all IABP procedures [27]. ACC/AHA and ESC guidelines strongly favor the use of an IABP in cardiogenic shock [28, 29]. Nevertheless, the evidence supporting the use of IABPs in cardiogenic shock is fragile, despite it having become the de facto standard of care for the treatment of cardiogenic shock. Registry data from the National Registry of Myocardial Infarction (NRMI)-2 as well as from the SHOCK (Should We Emergently Revascularize Occluded Coronary Arteries in Shock) trial suggested decreased mortality in cardiogenic shock patients who received IABP and thrombolytics as opposed to just thrombolytics [30, 31]. However, when including PCI, the patients with IABP did not have any benefit in NRMI-2 registry. A recent meta-analysis of randomized and observational date found a similar lack of benefit from the IABP, especially in the setting of optimal care [32]. In one of the earlier reports from the Benchmark Counterpulsation Outcomes Registry, the incidence of both major limb ischemia (0.9 %) and major bleeding (0.8 %) was acceptable compared to much higher prior numbers [33]. Limitations of the IABP lead directly to the development of the novel percutaneous assist devices. The strongest application of the IABP would be in resides in situations requiring reduction in oxygen demand is needed. The results of the CRISP-AMI trial revealed that IABP was not useful in addition to primary PCI for the treatment of STEMI without shock [34]. The recent IABP SHOCK II trial has called the effectiveness of routine IABP use in the setting of cardiogenic shock in question [35]. This randomized, open-label clinical trial evaluated 600 patients presenting with acute myocardial infarction and cardiogenic shock divided into patients receiving and not receiving intra-aortic balloon counterpulsation with intent for early revascularization and optimal medical support. IABP did not reduce mortality (39.7 % vs. 41.3 %, P = NS) or major predefined secondary endpoints. While limitations exist within this investigational setting, this trial supports the need for improved methods to manage this critical patient subset.
Percutaneous Left Ventricular Assist Devices (LVADs)
As opposed to the IABP, percutaneous LVADs provide active hemodynamic support with demonstrable difference in hemodynamic parameters. The two most commonly used percutaneous left ventricular assist devices (LVADs) in the USA are the TandemHeartTM and the Impella®. The TandemHeartTM (TandemHeart, Cardiac Assist, Pittsburgh, PA, USA) is a left atrial-to-femoral artery LVAD, driven by a continuous low-speed centrifugal pump [36]. The Impella® (Impella, Abiomed Europe GmbH, Aachen, Germany) is catheter-based axial-flow pump that pumps blood directly from the left ventricle into the ascending aorta [37]. A meta-analysis of three recent trials of IABP vs. the TandemHeartTM (two trials) and the Impella® (one trial) showed that while these newer devices had better hemodynamic parameters, they did not necessarily improve survival at 30 days [37–39]. Moreover, the TandemHeartTM was found to be associated with significantly worse bleeding and limb ischemia. The recently concluded PROTECT II trial showed in a priori analysis that the Impella® device was similar to the IABP in terms of major outcomes in elective high-risk PCI. It is important to remember that both the TandemHeart and the Impella devices are about ten times as expensive as the IABP. IABPs currently use a 7.5F or 8F sheath, while the Impella requires a 13F arteriotomy and the TandemHeart requires a 17F arteriotomy.
TandemHeartTM
The TandemHeartTM is a percutaneous left atrium to iliac artery bypass device. Powered by a centrifugal pump, it can provide up to 4 L/min in forward flow. Insertion technique required venous access and transseptal puncture, with a 21F inflow cannula. Using arterial access a 15F or 17F outflow cannula is placed in the ipsilateral common iliac artery. In the initial human pilot studies, the TandemHeart decreased LV end-diastolic pressure and oxygen demand while simultaneously increasing mean arterial pressure [36]. A small multicenter randomized trial followed comparing the device to the IABP [39]. However, a subsequent meta-analysis of two trials did not show any difference in mortality [32].
Given the demands of transseptal puncture and the large cannulas insertion times in excess of 30 min have been reported in literature [40]. In addition to bleeding and limb ischemia, specific complications of the TandemHeart include arrhythmias, tamponade, atrial perforation, as well as residual atrial septal defects. Specific contraindications include a ventricular septal defect as well as aortic insufficiency or severe peripheral vascular disease. With worsening LV function, hemodynamic support becomes an overriding concern, and it is in this situation that the TandemHeart has definitive indications. The Impella 5.0 may deliver as much support as the TandemHeart but cannot be inserted percutaneously.
Hemodynamic effects of the TandemHeart device include augmentation of both cardiac output as well as blood pressure, effectively raising the cardiac power output. In simulated models, the CPO from a TandemHeart is between the Impella 2.5 and the Impella 5.0 devices, irrespective of the hemodynamic status [41]. Oxygen consumption is directly lowered by the device. In cardiogenic shock the increase in afterload would counter the decrease in myocardial oxygen demand thereby leading to a net neutral effect on myocardial oxygen demand. In animal models of acute myocardial infarction, the device has been demonstrated to restore epicardial as well as microvascular blood flow [42].
At the time of this writing, the US Food and Drug Administration is reviewing a proposal to study the ability of TandemHeart to reduce infarct size when it is placed prior to primary PCI. The TandemHeart to Reduce Infarct Size (TRIS) trial will assign STEMI patients randomly to primary PCI with or without TandemHeart support prior to recanalization of the culprit vessel. Shock patients will be excluded from this trial, but if results are encouraging, additional study in the shock population would be pursued (personal communication, 2011, Howard A. Cohen MD).
Impella®
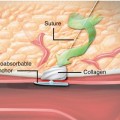
The Impella consists of a small axial-flow pump that directly unloads the left ventricle by attaching to a pigtail catheter and moving blood from the left ventricle into the ascending aorta. Two devices are currently available with maximal flow rates of 2.5 L/min (Impella 2.5) or 5 L/min (Impella 5.0). The Impella requires a single femoral arteriotomy and the insertion of a 13F (Impella 2.5) catheter. After crossing the aortic valve, an exchange length 0.018″ stiff wire is used to place the device in the LV. Implantation times around 10 min have been documented [43]. A complication specific to the Impella device is hemolysis that can occur in 5–10 % of patients [44]. Aortic valve disease and LV thrombi are specific contraindications to insertion of the Impella device. The Impella has more supportive clinical data for efficacy in the failing ventricle than does the TandemHeart. The first US feasibility trial (PROTECT I) was a multicenter study of 20 sequential patients treated with Impella 2.5 device in a nonrandomized fashion [44]. All patients had poor left ventricular function (ejection fraction ≤35 %) and underwent PCI on an unprotected left main coronary artery or last remaining patent coronary conduit. Patients with acute myocardial infarction or cardiogenic shock were excluded from this study. Two patients died at days 12 and 14, and two patients developed transient hemolysis. The European AMC MACH I trial produced very similar results [37]. The AMC MACH 2 trial looked at patients who were experiencing an acute anterior wall myocardial infarction without cardiogenic shock. Compared to IABP, improvement in the LVEF was noted [43]. The ISAR SHOCK trial randomized patients with an acute anterior wall myocardial infarction with cardiogenic shock and demonstrated improved hemodynamics when compared to the IABP [45]. In the PROTECT II trial, the Impella 2.5 device was compared to IABP in patients with low LV ejection fractions undergoing non-emergent but high-risk PCI with an expectation that benefit would be seen, using a large composite endpoint made up of ten individual clinical outcomes. [46] The study was terminated prematurely because of futility. An a priori analysis showed no difference in mortality between the Impella and the IABP. Despite these disappointing findings, some investigators and many operators appear to believe the results were confounded, as evidenced by the continued (indeed, expanding) use of this device in such patients. In the Europella registry, the Impella device was used in elderly patients with an ejection fraction of less than 30 %. Mortality at 30 days was 5.5 % and hemolysis was seen in about 1 % of patients [47]. It should be noted that the majority of the clinical data are derived from the Impella 2.5 device and that the surgically placed Impella 5.0 device has yet to be subjected to rigorous clinical trial analysis. The IMPRESS in STEMI (European Impella vs. IABP Reduces Infarct Size in STEMI Patients Treated with Primary PCI) is an ongoing clinical trial that compares the Impella 2.5 with the IABP in pre-shock STEMI patients. Although these studies do not target overt heart failure or cardiogenic shock patients specifically, the results of these trials will help determine the best populations to target for use of these advanced devices.
Conclusion
Inotrope and vasopressor therapies have been demonstrated to adversely impact infarct size and long term survival in return for a modest increase in short-term survival. Earlier institution of mechanical support devices may allow the heart to rest while simultaneously preserving systemic perfusion. Preliminary study indicates that such a strategy should decrease final infarct sizes, particularly if implemented early, and would lower mortality rates. Clinical trials are ongoing.