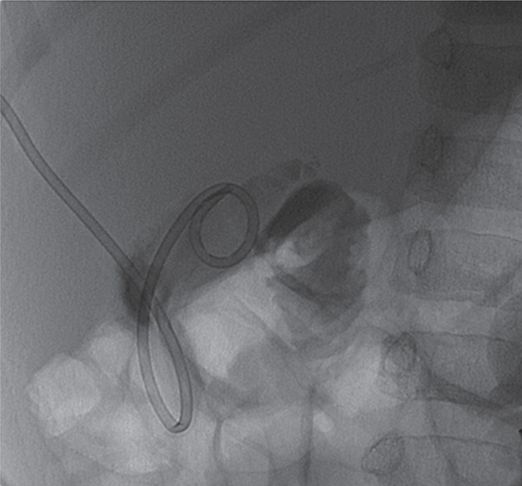
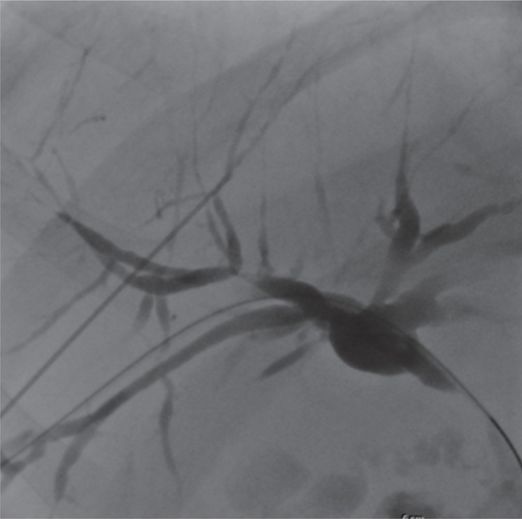
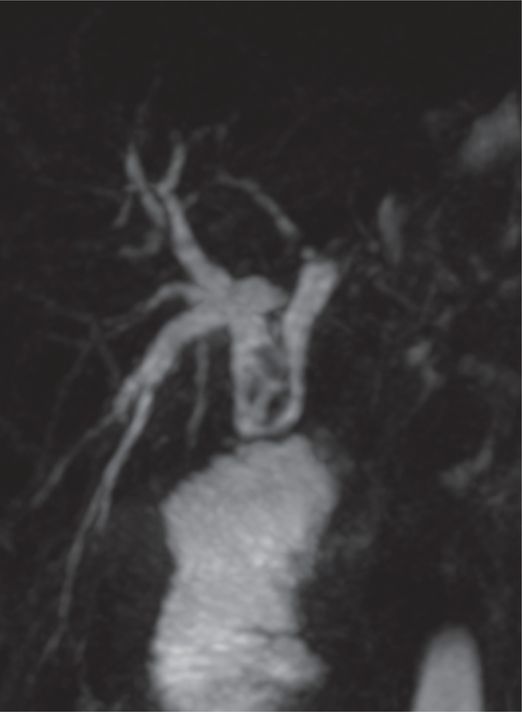
A dilated duct was identified with US just superficial to a portal vein. In this image, the 22-gauge needle (arrowhead) is advanced into the dilated duct.
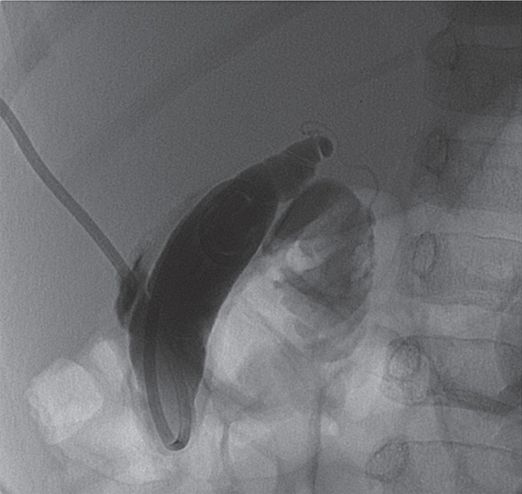
Initial cholangiographic injection shows only filling of irregular and severely attenuated right lobe ducts.
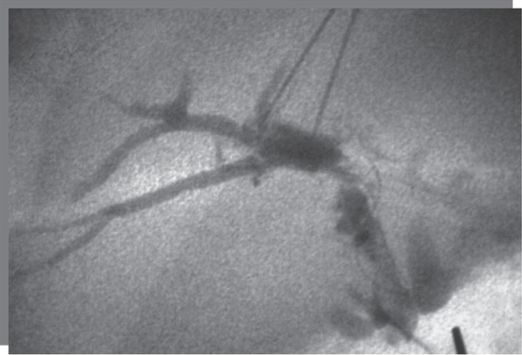
After two years treating multiple strictures in a number of intrahepatic ducts, contrast injection shows a tightly strictured right hepatic duct (arrow), resistant to numerous attempts at cholangioplasty.
A 4 mm × 2 cm cutting balloon was inflated across the right hepatic duct stricture.

Contrast demonstrates improved flow of contrast into right lobe ducts.
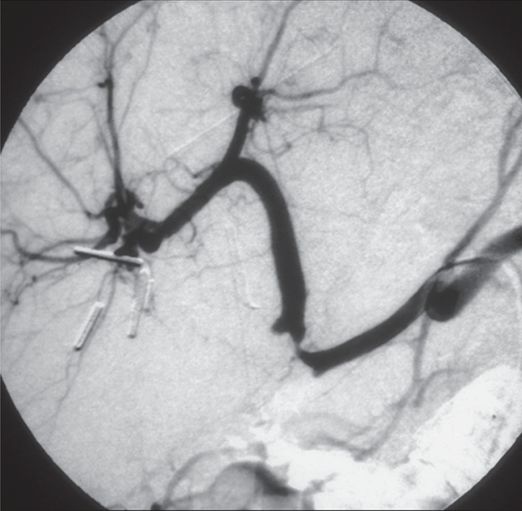
Two drains were left to stent-treated ducts from the left: one with the pigtail removed and extra side holes across the right hepatic duct, and a second drain across the common duct in the small bowel. The drains were subsequently removed and the patient has avoided need for retransplantation.
The patient is positioned and prepared as already described. Real-time US can be used to facilitate puncture of dilated peripheral ducts while avoiding vascular structures. It is our practice to use a freehand technique with a sterilely draped high-frequency (12 to 17 MHz) linear transducer with excellent near-field resolution and good penetration. A micropuncture kit with a 22-gauge Chiba needle is the workhorse of biliary access. Under certain conditions a 20-gauge sheathed needle with a 4 or 5 French sheath may be useful to enter a dilated biliary system, providing a larger lumen with which to aspirate thick bile avoiding multiple wire exchanges. Ultrasound can be especially helpful when no ductal dilation is present because it can direct the operator to the expected position of the duct(s) in portal triads that are readily visible on US.
In adults with dilated ducts, opacification of the biliary tree occurs in 99 to 100% of cases with four to six needle passes. The success rate in puncturing ducts that are not dilated on US examination is between 60 and 80%, and in these cases more needle passes are usually required. Similar rates are achievable in children, more so because of improved visualization using US in smaller patients. If we have not opacified bile ducts within 15 to 20 passes, we abandon the procedure. In rare instances, direct puncture of larger, more central ducts may be attempted, usually with US guidance to minimize the risk of puncturing extrahepatic ducts with the attendant higher complication rate. In selected cases direct puncture of the gallbladder (see “Transcholecystic cholangiography (TCC),” below) may be considered to opacify decompressed ducts, especially when the primary purpose is diagnostic, as in most neonatal PTC.
Fluoroscopically guided access
Fluoroscopy can be used in two ways to access bile ducts. First, if contrast, including gas or air, is already filling ducts (for example, from prior access attempts, from needle access that cannot be converted for further procedural use, or from transcholecystic injection, see below), a suitable duct can be targeted for access by triangulation. Alternatively, “blind” attempts can be made to traverse a suitable duct by inserting the needle in a statistically likely orientation, then testing with gentle puffs of contrast as the needle is withdrawn until contrast fills a tubular structure with signature biliary characteristics (i.e., slow flow toward the porta hepatis). Using this method, the needle customarily enters the liver approximately one-third of the way up from the inferior margin of the liver (usually between the seventh to tenth intercostal spaces), just anterior to the mid-axillary line, and is advanced parallel to the caudal margin of the liver and toward the ipsilateral costovertebral junction. The pleural reflection in the mid-axillary line often extends as low as the level of the tenth rib, usually well below the lung in shallow respiration. This means some punctures may be transpleural but not transpulmonary. The needle should be inserted just above the superior edge of the rib in order to avoid the neurovascular bundle. The advantage to this approach is that it usually places the trajectory of the needle in line with the right lobe biliary ducts, making catheterization of the ducts more straightforward if drainage is ultimately required.
Under fluoroscopic guidance, the needle is inserted as described in the previous paragraph until the tip of the needle is just lateral to the spine. The stylet is removed and a syringe filled with dilute non-ionic contrast is attached to clear flexible tubing, which is then connected to the hub of the needle. Dilute contrast (1:1 to 2:1 contrast to saline) is used so that the contrast can be absorbed more rapidly and persistent contrast from multiple attempts does not obscure the field.
Using fluoroscopy, preferably with magnification, the needle is slowly withdrawn as contrast is steadily but very slowly injected. The goal is to “draw” a thin, continuous line of contrast behind the retreating needle, and a persistent, thin tract of contrast in the liver parenchyma should be seen as the needle is pulled back. The needle should be pulled back to the liver periphery, but not out of the capsule, in order to minimize the number of holes in the capsule and thereby reduce the risk of bleeding. If too much contrast is injected it will form “puddles” in the liver parenchyma, which can hamper later attempts to opacify the biliary ducts and potentially obscure findings once the biliary ducts are opacified.
If no contrast is seen in the bile ducts on the first pass, subsequent needle passes should be made systematically, fanning out from the first tract in the cephalo-caudad direction, staying in the same coronal plane. Caudal passes should be made cautiously in order to avoid advancing the needle too far medially where inadvertent puncture of the gallbladder, porta hepatis, vena cava, or aorta might occur or where the capsule might be punctured resulting in extrahepatic, intraperitoneal injection of contrast. The latter may be quite painful and can stimulate a vasovagal response and shortness of breath. In addition, puncture of the extrahepatic ducts in an obstructed system can lead to bile peritonitis, which is a potentially serious complication. If no ducts are opacified in the original coronal plane, then the needle should be repositioned or the angle changed in the axial plane and the process repeated until ductal opacification is seen.
Whether the access needle is positioned under US or fluoroscopic guidance, location of the tip within the lumen of a bile duct must be confirmed before the biliary tree can be filled with contrast for diagnostic imaging of further procedural guidance. When injected into the liver parenchyma contrast remains near the needle tip but as soon as the needle enters a duct or vessel the contrast flows away from the tip. Hepatic veins may be recognized by the rapid flow of contrast toward the right atrium. Portal veins and hepatic arteries are recognized by rapid flow of contrast toward the liver periphery. Differentiating portal veins from hepatic arteries may be somewhat difficult, but blood flow in hepatic arteries is somewhat slower and more pulsatile than in portal veins and results in a more intense parenchymal blush. Lymphatic vessels are identified by their small size, beaded appearance, and very slow flow of contrast toward the porta hepatis. Once lymphatic channels are filled with contrast they can remain opacified for up to ten minutes.
Bile ducts are identified by the slow movement of contrast toward the hilum and by the relatively rapid appearance of a branching pattern. With a patent biliary tree, contrast will flow into the common duct and eventually into the duodenum, or into the Roux loop or jejunum in the case of liver transplant or prior surgery. Once the biliary tree is opacified it is useful to image in multiple projections including straight anteroposterior views, AP views with cranial and caudal angulation, and both anterior oblique views. Rotational biliary angiography may be useful in certain situations to clarify anatomic relationships and to reduce the number of imaging planes, and therefore time and dose, required to answer the clinical question.
Technical variations
CO2 as a contrast agent
Because iodinated contrast has a higher specific gravity than bile, it will flow into the more dependent, posterior ducts when the patient is supine. This gravity-dependent flow may impede opacification of central ducts and almost always limits opacification of the left ducts, which are more anterior than those on the right. In order to get complete filling of the ducts several maneuvers may be used with caution. Large volumes of contrast may be injected, but this may increase the risk of septic complications. The patient may be carefully rolled onto the left side, but changing position when the patient is sedated or under general anesthesia can be challenging, and the possibility of dislodging the needle from the bile duct is high. Lowering the head of the table or tilting along the z-axis may facilitate filling of the left ducts in angiography suites outfitted with tilting tables.
Carbon dioxide (CO2) has a lower specific gravity than bile and flows readily to the anterior ducts. It can therefore be used as a contrast agent to opacify the left ducts, which can then be selectively punctured and injected with iodinated contrast. However, injection of CO2 has limitations and is not always effective. While the extrahepatic biliary system is well visualized with CO2, the intrahepatic ducts are often poorly or inadequately visualized because of their small caliber and the relatively low conspicuity of CO2. In addition, CO2 needs to be injected cautiously because the low viscosity of the gas can cause much higher flow rates than occur with liquid contrast and, because CO2 is compressed in the syringe, much higher volumes can be delivered with the risk of overdistending the biliary tree.
Left lateral (subxiphoid) approach
In certain situations, the left ducts cannot be visualized, despite the use of one or more of the various maneuvers described above. When there are separate right and left duct obstructions, or when a segmental obstruction of the left duct is known or suspected, or when performing a PTC in a recipient of a left lobe segmental graft, direct imaging of the left ducts is required. The right lateral approach may be used in the former two situations. This approach requires the needle to pass deeper into the liver and be directed more anteriorly and into the medial portion of the left lobe. In these cases a second puncture will usually be required, especially if intervention is necessary. However, in children with segmental transplants, because the cut surface of the liver is directed laterally and somewhat posteriorly and may have loops of bowel interposed between the cut surface and the abdominal wall, the right lateral approach is not used.
The alternative is an anterior, subxiphoid or subcostal approach. This is most easily achieved working from the patient’s left side. In some rooms, this may require placing the patient feet first on the table. In almost any room this requires some preprocedure planning to position personnel, supplies, anesthesia equipment, etc., most effectively. When performed with US guidance, this approach follows naturally from the location of available US windows, and is our preference. When this technique is employed under fluoroscopic guidance, the needle is inserted in the mid-epigastrium just below the xiphoid cartilage and aimed toward the patient’s right side at an angle of about 30 to 40 degrees from vertical. The needle is inserted approximately 6 to 8 cm and then is slowly withdrawn as contrast is injected, just as in the right lateral approach.
Postprocedure and follow-up care
Patients are on strict bed rest with the access site down, if possible, for four to six hours. They are observed closely in the postprocedure period, for at least four hours, for signs of septic or hypovolemic shock. Frequent vital signs are taken and a repeat hemoglobin and hematocrit are obtained four hours after the end of the procedure to look for signs of bleeding. Intravenous antibiotics are continued for at least 24 hours after the procedure.
Complications
Published series of adult patients who have undergone PTC suggest an expected rate of complication around 3 to 5% and a mortality rate of 0.1 to 0.2%. Sepsis, bile leak, and intraperitoneal hemorrhage are the most common complications, occurring in 1 to 3% of patients. Other much less frequent complications included pneumothorax, contrast reaction, vasovagal reactions, and hepatic arteriovenous fistulae. Our experience in the pediatric population has not been significantly different.
Transcholecystic cholangiography (TCC)
Introduction
If all attempts to opacify the intrahepatic bile ducts using PTC or ERCP have failed, transcholecystic cholangiography (TCC) may be attempted. Transcholecystic cholangiography has the distinction of being one of the oldest percutaneous radiologic interventions, first reported by Burkhardt and Muller in 1921. While TCC has a variable success rate in opacifying intrahepatic bile ducts in adults, in pediatric patients the intrahepatic ducts are routinely well visualized.
Indications
Besides visualization of the intrahepatic biliary tree, other indications for TCC include evaluation of the patency of the cystic duct, diagnosis of iatrogenic gallbladder or bile duct injury, evaluation of the biliary tree in patients with suspected ampullary stenosis and failed ERCP, evaluation of the distal common bile duct in cases of obstruction of the proximal common bile duct and as a prelude to gallbladder drainage (Table 5.5). In the literature most of the reported cases are in adult patients, as most of the indications for this procedure are uncommon in the pediatric population. However, TCC can be an effective way to image non-dilated biliary radicles in patients with suspected biliary disease and can be used to facilitate placement of a transhepatic biliary drainage catheter in an obstructed but non-dilated system. It can provide a very effective means for initial opacification of non-dilated ducts in neonates, facilitating subsequent selective puncture of biliary radicles using a transhepatic route. Obviously, this procedure is not applicable to transplant patients who have no gallbladder or to patients who have had a cholecystectomy. If infection of the gallbladder, biliary tree, or soft tissues of the prospective tract is known or suspected, TCC should be deferred until the infection has been cleared.
Alternative to PTC especially when ducts are small and obstructed
Determine patency of cystic duct to level of ampulla of Vater
Prelude to gallbladder drainage, e.g., acalculous cholecystitis
Opacification of biliary radicles to facilitate PTC in selected cases
Biliary atresia
Technique
Patient preparation
As with PTC, the patient receives intravenous antibiotics prior to the procedure. Anemia or coagulopathy are corrected as fully as possible.
Standard technique
There are two approaches to puncture of the gallbladder. Some interventionalists prefer the shortest, most direct route to the gallbladder, which is usually transperitoneal, from a subcostal or intercostal approach. To decrease the risk of bile peritonitis, we prefer the transhepatic route when possible. With the patient supine, an intercostal approach is used (Table 5.6). Using real-time US guidance, a 22-gauge Chiba needle or sheathed needle is inserted into the gallbladder. A darting jab is usually required to puncture the gallbladder wall, but care should be taken to try to puncture only one wall to minimize the chance for bile leak. Prior to contrast injection, a small amount of bile is aspirated in order to verify the intracholecystic position of the needle and to obtain a specimen for culture or laboratory analysis if necessary. Alternatively, introduction of a small amount of air under US visualization or contrast injection under fluoroscopy can confirm proper position of the needle within the gallbladder.
Sedation or general anesthesia
Ultrasound evaluation for route planning
Prepare and drape in sterile fashion
Local anesthesia at entry site
Ultrasound-guided puncture of gallbladder
Injection of contrast to opacify biliary tree
Imaging obtained in multiple projections
Rotational cholangiography may be helpful in route planning
Once needle position is confirmed, bile is aspirated and non-ionic contrast is then slowly injected into the gallbladder in an amount sufficient to fill the bile ducts. Overdistention of the gallbladder should be avoided. If intrahepatic ducts are not well filled, patient position may be changed or the patient may be moved into the Trendelenburg position. Intravenous injection of morphine sulfate can be used to cause spasm of the sphincter of Oddi in order to facilitate filling of intrahepatic ducts. As discussed for PTC, imaging should be obtained in multiple projections. At the end of the study the gallbladder should be decompressed as much as possible before the needle is removed.
Percutaneous cholecystostomy
Introduction
Primary biliary disease is uncommon in children, but when it does occur the gallbladder is usually involved. Acute cholecystitis in children is most often idiopathic, but may be related to infectious etiologies (usually viral, bacterial, or parasitic) or, rarely, to gallstone disease. Calculous cholecystitis in the pediatric population is seen most often in girls ages 16 to 20 years, and often associated with oral contraceptives or pregnancy. In addition, gallstones may be associated with chronic hemolytic diseases, especially sickle cell anemia, congenital biliary disease, or non-hemolytic disorders such as intrahepatic cholestasis secondary to total parenteral nutrition, dehydration, pancreatitis, and cystic fibrosis. These conditions may affect either sex. Gallbladder hydrops, which is often idiopathic and not associated with cholecystitis or gallstones, may present at any age in the pediatric spectrum, and is predominately found in males. In each of the above conditions, decompression and evacuation of the gallbladder may often be curative. Traditionally, this has been accomplished by surgical drainage or cholecystectomy in those patients medically able to tolerate the operation. Currently, interventional techniques offer a minimally invasive alternative procedure for most of these patients.
Introduced around 1978, percutaneous cholecystostomy has been performed in children since the late 1980s. Catheterization of the gallbladder has been used for diagnosis, gallbladder drainage, gallstone dissolution, gallbladder ablation, and dynamic pressure and perfusion studies, as well as a route of access for other procedures, including gallstone extraction and gallbladder biopsy. Minimally invasive approaches have been shown to be a cost-effective alternative to open cholecystectomy and offer definitive therapy for young, otherwise healthy patients who require gallbladder decompression for cholecystitis.
Percutaneous cholecystostomy also offers a safe and effective method of draining the gallbladder in patients at high risk for surgery in whom gallbladder disease is known or suspected. It may be difficult to elicit clinical signs and symptoms in such patients when they are unresponsive or on a ventilator. In these patients, the need for diagnosis is paramount. Goals of therapy include defervescence, normalization of white blood cell count, or improvement in clinical symptoms and signs within 48 to 72 hours of percutaneous drainage. Failure to achieve these goals suggests either a non-biliary source of illness, or that the benefits of cholecystostomy are being masked by other medical conditions in these complex patients. Failure to respond to percutaneous cholecystostomy is also associated with a high mortality rate. Percutaneous cholecystostomy may be definitive therapy, e.g., for patients with acalculous cholecystitis, or in combination with percutaneous lithotomy, lithotripsy, or contact solvent dissolution for children with cholelithiasis. It is also an effective temporizing therapeutic maneuver until the patient is sufficiently stable for surgical cholecystectomy. At this time, cholecystostomy is considered to be the definitive therapy for children with acalculous cholecystitis (Figure 5.2).
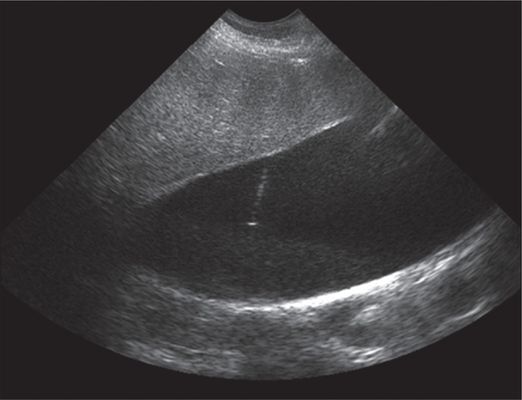
One-year-old female with severe combined immunodeficiency after bone marrow transplant with acalculous cholecystitis.
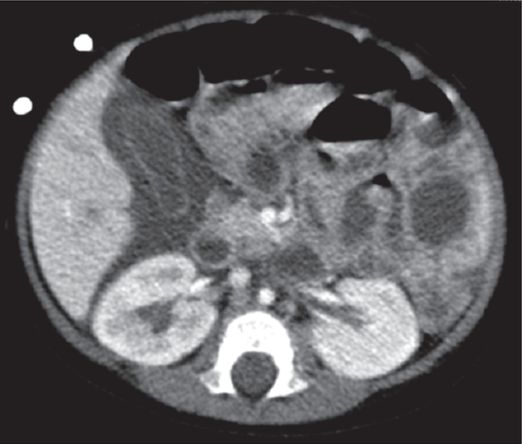
Axial contrast enhanced CT shows pericholecystic fluid with mild gallbladder wall enhancement and thickening.

Ultrasound shows gallbladder sludge prior to needle access.

Gallbladder drainage. Injection shows patent cystic duct.
Indications
Indications for percutaneous cholecystostomy include the need for decompression of the gallbladder (e.g., in calculous or acalculous cholecystitis, hydrops, empyema, or gallbladder perforation), cholangitis, biliary obstruction, the need for diagnostic imaging of the biliary tree, or as a route of access for additional interventions (Table 5.7). Percutaneous cholecystostomy should be regarded as the first-line intervention in critically ill patients in whom gallbladder disease is known or suspected. Because percutaneous drainage may often be definitive therapy in young and otherwise healthy patients, this is the procedure of choice in this population.
Gallbladder decompression
Access route for additional interventions
Reduction in serum bile salts, e.g., Alagille syndrome with pruritis
The response rate in adults is highest when clinical and radiologic signs are referable to the gallbladder and right upper quadrant, especially in the presence of a sonographic Murphy’s sign or multiple radiologic signs (i.e., gallbladder wall thickening, distention, stones, and pericholecystic fluid). Clinical signs of acute cholecystitis are generally less definitive in children than in adults. Controversy remains regarding whether to drain or aspirate the gallbladder in high-risk patients who are not critically ill. This question has not been addressed in pediatric patients. Percutaneous cholecystostomy may also be useful as an alternative to percutaneous transhepatic biliary drainage (PTD, see below) in cases where biliary radicles are not sufficiently dilated or well visualized. This is an especially effective choice for diagnostic studies in neonates and small children when biliary disease is suspected.
Technique
Equipment
The equipment necessary for percutaneous cholecystostomy is similar to that used for other simple drainage procedures (Table 5.8). The smallest catheter required to achieve adequate drainage without catheter blockage should be used. A 6 to 8.5 French pigtail drainage catheter is usually satisfactory for such interventions as decompression and contact dissolution of stones. A larger tract (up to 24 French) may be necessary when secondary procedures are contemplated, such as mechanical stone removal. Only an internally locking catheter should be used, and fixation of the catheter to the skin should be secure, due to the risk of severe complications with inadvertent dislodgment.
Materials for sterile preparation and draping
22-gauge Chiba needle (0.7 mm O.D.)
4 French or 5 French micropuncture set with 0.018-inch stiff glide wire or Roadrunner® wire and 0.035-inch stiff wire
Additional 4 French introducer sheath with metallic or plastic cannula
18-gauge Chiba needle (0.018-inch approach), Yueh sheathed needle (0.035 to 0.038-inch approach)
Connecting tubing
20 ml syringe filled with non-ionic contrast diluted 1:1 with normal saline
5 French, 6.5 French, or 8.5 French pigtail drains
Patient preparation
Preparation for percutaneous cholecystostomy is identical to PTC preparation, as described above. Any available preoperative imaging of the region should be reviewed, and US may be used during preparation for the procedure, to evaluate the gallbladder fossa for any abnormal vessels that may be at risk during the procedure. Vascular malformations are known to occur in this region and any large or abnormal vessels may affect the planned route of access.
Standard technique
We prefer to complete guide wire and catheter insertion under fluoroscopic control after obtaining access with US guidance (Figure 5.3). However, the entire procedure can be performed with US guidance alone if necessary (Table 5.9). Using US, the procedure can, on rare occasion, be performed at the bedside if the patient’s condition is too unstable for transport to the interventional suite. In cases of difficult access, such as in obese patients or when visualization of the gallbladder is otherwise poor, CT may be used for guidance.
Twenty-month male with history of Alagille syndrome with refractory pruritis and hyperbilirubinemia.
Ultrasound-guided transhepatic needle access of the gallbladder.
5 French Towbin (Duan) pigtail drainage catheter in gallbladder.
Contrast injection shows patency of the cystic duct. Pruritis improved.
General anesthesia
Intravenous antibiotics to cover enteric organisms
Ultrasound to identify the gallbladder and mark the skin entry site
Sterile preparation and draping of the operative field
Ultrasound-guided, transhepatic needle puncture of the gallbladder
Collect bile for culture and laboratory studies
Inject contrast to illustrate pathologic anatomy
Inserted a stiff guide wire, dilate tract, and insert drainage catheter
Perform a transcholecystic cholangiogram. Avoid overdistention of biliary system since bile is likely infected and can cause biliary sepsis
Following instillation of local anesthetic (if the procedure is not done under general anesthetic) either a Seldinger or a trochar technique may be used to gain initial access to the gallbladder. Specimens for bile cultures (aerobic, anaerobic, and fungal) with Gram stain should be obtained during aspiration or drainage of the gallbladder, prior to the introduction of contrast or other bacteriostatic agents. Interestingly, culture results are poorly predictive of the outcome of the intervention, and are especially insensitive in patients already receiving antibiotics. Nevertheless, if a positive culture is obtained it can be used to guide antibiotic therapy.
If a Seldinger technique is used, initial access is usually with a 21- or 22-gauge Chiba or an 18-gauge sheathed needle. The puncture site is guided by US imaging, but will usually be in the anterior axillary line in the eighth or ninth intercostal space, or, occasionally, subcostal. After passing through hepatic parenchyma (preferably through the “bare” area of the liver), the needle should enter the gallbladder between the fundus and the mid body. Small aliquots of bile should be obtained for cultures, leaving adequate bile within the gallbladder to keep it distended, facilitating coiling the guide wire and positioning of the drainage catheter. In an unobstructed system where infected bile is not suspected, a small amount of contrast may be instilled to opacify the gallbladder. Retrograde cholecystocholangiography may be performed through the drainage catheter after therapeutic levels of antibiotics have been achieved and the system decompressed, usually 48 to 72 hours following intubation.
A floppy-tipped mandril wire or other relatively stiff, non-kinkable wire (such as an angled Glidewire®) is advanced until the transition zone to the stiff part of the wire is intraluminal. The tract is dilated to the diameter of the drainage catheter, or may be overdilated by 1 to 2 French. Finally, a locking drainage catheter is inserted and the loop is formed and locked. The catheter is securely fixed to the skin, taking care not to kink the catheter at the skin exit site. The gallbladder is decompressed by aspiration through the drain, and the catheter is left to external gravity drainage to a drainage bag.
Technical variations
We prefer a transhepatic route for instrumentation of the gallbladder in order to decrease the risk of leakage and potentially lethal bile peritonitis. In fact, tracts formed via a transhepatic route mature more quickly than by a transperitoneal route (two versus three weeks, respectively). Cope offers an alternative approach, using a removable anchor suture to temporarily bring the gallbladder into apposition with the anterior abdominal wall, allowing a percutaneous subhepatic approach with low risk of leakage and avoiding the risks of traversing the hepatic parenchyma, in select cases. It should be noted that colon is often interposed between the anterior abdominal wall and at least a portion of the gallbladder fundus, so care should be taken to avoid a transcolonic puncture if a transperitoneal route is selected.
Postprocedure and follow-up care
The catheter is left in place for at least four to six weeks. Prior to removal of the catheter, with a guide wire in place, tract maturity should be confirmed with contrast injection. Also, cholecystocholangiography performed using the catheter can also help ensure that the cystic and common bile ducts are patent prior to removal. Prolonged drainage is rarely necessary, since the gallbladder is usually either ruled out as the origin of illness, the patient rapidly improves, or the gallbladder is surgically removed.
Complications
In the adult literature, about three quarters of percutaneous cholecystostomies are therapeutic. Interval cholecystectomy is required in only a quarter of these cases, despite the fact that stones are found in nearly half. Potential complications include gallbladder perforation with bile leakage or peritonitis, leakage of infected bile, pericholecystic abscess, chole-enteric fistula, severe vasovagal reaction with hypotension, bleeding, hemobilia, sepsis, pneumothorax, bowel perforation, accidental catheter dislodgment, and death. However, the expected complication rate is under 15%, with serious complications expected in about 5%.
Bile peritonitis is the most worrisome complication and may necessitate urgent cholecystectomy in a patient likely to be a poor surgical risk. In pediatric patients, the most commonly reported complication is asymptomatic extravasation of contrast into the gallbladder fossa without significant sequelae, although the number of reported procedures is too low to make broad generalizations about the relative risk of the procedure.
Percutaneous transhepatic biliary drainage (PTD)
Introduction
First described by Molnar and Stockum in 1974, PTD is useful to treat biliary obstruction or bile leaks. In the pediatric population these problems are most commonly seen following hepatic transplantation, especially with ischemic strictures related to hepatic artery thrombosis (Figure 5.4). Percutaneous therapy may obviate or postpone the need for retransplantation or surgical exploration, sphincterectomy, or partial hepatectomy. Percutaneous drainage plays a particularly useful role in patients with a hepaticojejunal (e.g., Roux-en-Y) anastomosis, and others in whom endoscopic drainage is difficult or contraindicated.
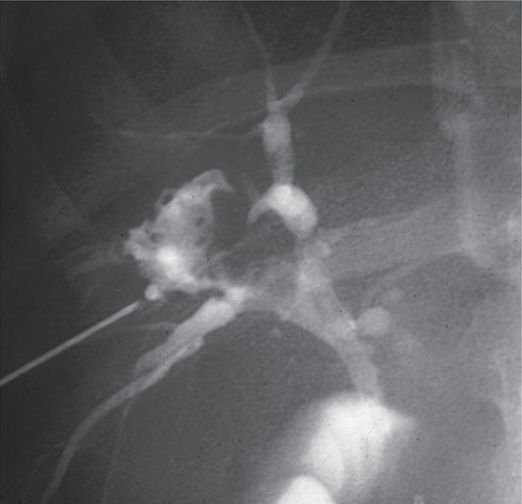
Eight-year-old female after liver transplant.
Percutaneous transhepatic cholangiography shows necrosis of the common bile duct.
Subsequent angiography revealed right hepatic artery occlusion.
Indications
As a general rule, any obstructed biliary tree should be drained. Even in patients who have multifocal obstructions, in whom biliary drainage is often challenging (Figure 5.5), even when multiple catheters are used, and who are vulnerable to recurrent bouts of cholangitis and sepsis due to bile stasis in the undrained segments, the interventionalist is often called on to attempt treatment since other therapeutic options are few and costly. In cases of partial or complete biliary obstruction, PTC should not be performed unless the operator is capable of inserting a biliary drain, because of the risk of bile peritonitis is high once the diagnostic needle has been removed.
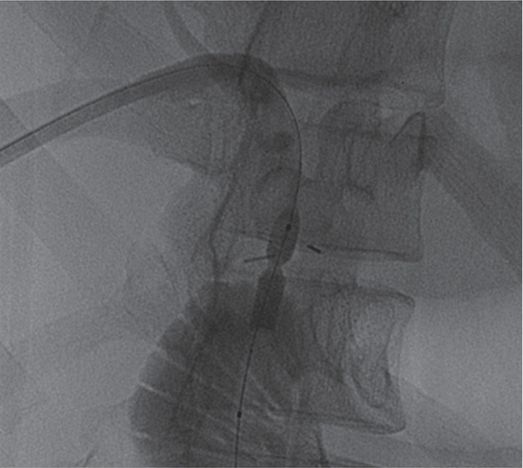
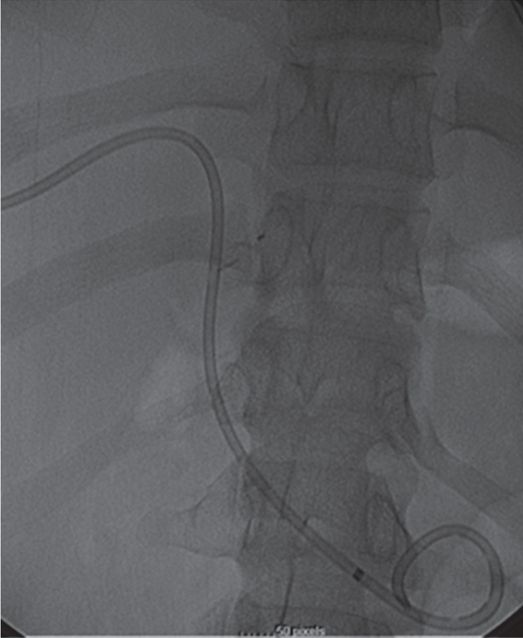
A 20-year-old female received a cadaveric whole-liver transplant in childhood. She was treated for hepatic arterial thrombosis with angioplasty by interventional radiology one month after her transplant. At age 20 she developed jaundice with an elevated gamma-glutamyl transferase (GGT) and abdominal pain.
Percutaneous transhepatic cholangiography shows a high-grade fixed stenosis (arrow) of an intrahepatic right lobe biliary duct that could not be crossed from above.
In a combined surgical-interventional procedure, the stenosis was crossed with a TIPS needle (arrow) from the small bowel through the common bile duct into the obstructed duct, and the guide wire was snared from above and exteriorized.
The stenosis was treated with a high-pressure PTA balloon.
After six months of stented drainage and serial dilations, her GGT remained normalized after removal of the catheter.
Biliary drainage is rarely needed in the pediatric population, and when needed the etiology is invariably benign (Table 5.10). Complications of liver transplantation, including anastomotic and ischemic strictures, are the most common etiologies necessitating biliary drainage. Other indications include strictures secondary to sclerosing cholangitis, postsurgical strictures (either at an anastomosis or due to ischemia) or trauma of the bile ducts, and congenital strictures (Figure 5.6). Patients with bile leaks (such as those associated with severe acute necrotizing pancreatitis) or large postoperative biliary defects will also benefit from percutaneous drainage (Figure 5.7).
Obstructed biliary system
Complication of liver transplantation
Postoperative strictures
Post-traumatic strictures
Iatrogenic strictures
Seven-year-old female with ulcerative colitis and abdominal pain who underwent CT demonstrating central intrahepatic biliary ductal dilatation.

Percutaneous transhepatic cholangiography shows a high-grade short segment stricture of the common bile duct.
Multiple intrahepatic ductal strictures, likely sclerosing cholangitis.
Five-year-old male post liver transplant with hepatic artery occlusion.
Percutaneous transhepatic cholangiography demonstrates a bile lake communicating with biliary tree.
Drainage of the bile lake.
Technique
Equipment
The PTD procedure is a modular hybrid of PTC and drainage of an abnormal fluid collection (see, for example, Chapter 4), modified for the purpose of leaving the drain in one of two places: either across the biliary–enteric connection or within the biliary tree on the access side of the stricture or obstruction. The recommended equipment requirements align with these functions (Table 5.11).
Equipment for PTC (Table 5.3)
Guide wires: 0.018-inch glide wire, mandril, tracker; 0.035-inch angled glide wire, stiff and superstiff wires
Dilators: 0.018-inch and 0.035-inch or 0.038-inch. 0.018-inch from 3 French – 5 French, and 0.035-inch or 0.038-inch from 4 French to 10 French
Locking drainage catheters: 6 French to 12 French biliary and pigtail drains
Sterile hole punch or scissors for creating side holes as needed
Biliary drainage bag
Retention device (SorbiView® SHIELD, Stat-Lock®, etc.)
Suture: 2–0, 3–0 silk
Transparent dressing
Patient preparation
Patient preparation is the same as described for PTC.
Standard technique
Single-stick method
There are two basic approaches that can be used to access the biliary tree: single stick and double stick. In the single-stick method the primary puncture of the bile duct needs to be appropriate for both opacification of the ducts and placement of a drain or stent. The biggest problem with this technique is when the primary needle puncture is within a duct that is not suitable for biliary drainage either because of its size, location, or trajectory with the common bile duct or biliary–enteric anastomosis. Often, the initial access enters a biliary radicle that is too close to the obstruction. If the guide wire cannot be maneuvered across the stenosis there may be insufficient purchase within the liver parenchyma for subsequent manipulations and placement of a drainage catheter. Also, if the biliary radicle initially entered makes an acute angle with the transhepatic tract then catheter insertion can be very difficult. In the absence of the above-mentioned technical issues, the single-stick approach is preferred. In our experience a single-needle technique is successful in most cases.
Double-stick method
In the double-stick method, opacification of the ducts is performed with the primary PTC needle puncture. The cholangiogram is used to select an appropriate duct for cannulation and a second puncture is then performed with fluoroscopic guidance. The second puncture can be done with another Chiba needle or, alternatively, if the bile duct to be entered is dilated, a larger needle (sheathed or unsheathed) that will accept a 0.035-inch or 0.038-inch guide wire can be placed. If a Chiba needle is used, a 0.018-inch flexible wire, such as an angled Glidewire® or stiff angled Glidewire® is placed into the bile duct and advanced into a stable position in the biliary tree or, if possible, beyond the stricture into the duodenum or jejunal loop of a Roux-en-Y. Guide wire position distal to the stricture is preferred when possible. A 4 or 5 French coaxial, end-hole introducer system can then be used to change from the 0.018-inch wire to a 0.035-inch or 0.038-inch wire. If the guide wire is not in the distal biliary tree or duodenum, a 4 or 5 French directional catheter (JB-1 or Kumpe) can be inserted and used to direct the wire beyond the stricture. Once the 0.035-inch or 0.038-inch wire is in a stable location the tract is dilated and a 6 or 8 French catheter, often a Ring catheter, is placed. If a stiff catheter is initially inserted, it is changed to a softer, more comfortable biliary drainage or pigtail catheter (with side holes cut into the portion of the catheter shaft that is intraductal) after five to seven days.
If in the initial drainage procedure attempts to traverse the stricture are unsuccessful, more aggressive attempts to pass the area of narrowing are not advisable. We prefer to leave a dilator, directional catheter, or straight drain carefully secured in position on the access side of the stricture. The biliary tree is drained and allowed to decompress for 48 hours or longer to allow inflammation and edema to subside. At this time, the stricture is usually more readily negotiated and a drainage catheter may be successfully placed (Table 5.12).
General anesthesia
Intravenous antibiotics to cover enteric organisms
Ultrasound to identify dilated biliary ducts and mark the skin entry site
Sterile preparation and draping of the right lateral chest
Fluoroscopic or US-guided, transhepatic needle passage with injection of dilute non-ionic contrast until a bile duct is entered
Inject contrast to illustrate pathologic anatomy
Inserted a stiff guide wire, dilate tract
If a stricture is identified, perform angioplasty
Measure tract length to understand where to place proximal drainage holes to maintain internal drainage
Insert a drainage catheter
If the child is sick one may delay performing a cholangiogram until antibiotics have a chance to sterilize the bile
Perform cholangiogram at appropriate time. Anteroposterior, right anterior oblique, left anterior oblique, and craniocaudad views in best oblique
It may be necessary to dilate the stricture to allow passage of the drainage catheter. This can be accomplished with vessel dilators or a PTA balloon catheter (Figure 5.8). In this situation the use of a stiff wire, such as a stiff Amplatz® or ultra-stiff Glidewire®, is helpful. If the stricture is so tight that a catheter cannot be passed beyond it, a drainage catheter is positioned just proximal to the stricture.
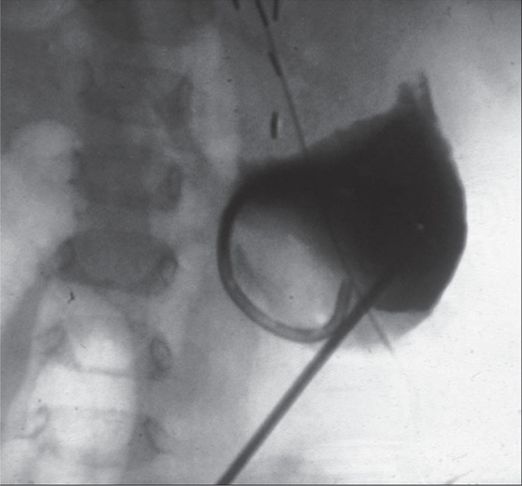
Sixteen-year-old female with history of hepaticojejunostomy and recurrent bouts of cholangitis.
Magnetic resonance cholangiopancreatography (MRCP) shows an anastomotic stricture and several large filling defects.

Percutaneous transhepatic cholangiography shows a high-grade anastomotic stricture and multiple large stones.
A percutaneous transluminal angioplasty balloon shows “waisting” at the stricture.
Biliary drain in place.
Once the catheter is in position a cholangiogram is performed to confirm the location of the side holes and the adequacy of drainage. If the catheter has successfully crossed the stricture care must be taken to have drainage holes both proximal and distal to the stricture to promote bile drainage. The position of side holes on the catheter is easily measured in one of two ways: the bent guide wire technique or a calibrated wire. With a guide catheter in position several centimeters into the duodenum the tip of a guide wire is positioned just at the catheter tip and then bent or clamped at the catheter hub. The wire is then pulled back until the tip is proximal to the stricture but still within the duct and the wire is again bent or clamped at the catheter hub. The wire is removed and the length of wire between the bends or clamps is the length of catheter where side holes need to be made.
A second technique involves the use of a wire or catheter that has radio-opaque marks at one-centimeter intervals. The tip of the measuring device is placed several centimeters into the duodenum and the distance from the tip to a point upstream of the obstruction but within the duct can be directly measured and transferred to the drainage catheter. Once the tract length has been measured and the side holes have been cut, a guide wire is inserted into the drainage catheter until the tip is at the most proximal side hole and the wire is bent at the catheter hub. After the catheter has been inserted, the premeasured wire is placed into the catheter and advanced to the bend. The tip of the wire will then indicate the position of the most proximal side hole. The position of the drainage catheter can then be adjusted accordingly so that all side holes are intraductal. It is important that none of the side holes are within the liver parenchyma to avoid bleeding into the drain.
Separate drainage of the left biliary system is indicated in some cases. The most common indications for this include unilateral obstruction of the left biliary system, independent obstructions of both right and left systems, or unfavorable anatomy on the right from previous surgery, interventions, or disease. Other indications include ascites and uncontrollable labored respiration, as the respiratory excursion of the left lobe is less than on the right.
In cases where the left ducts are to be drained a preliminary US of the liver is often desirable, as the size and morphology of the left lobe can vary greatly. This is particularly true in the case of procedures required in patients who have received segmental liver transplants. Drainage is done from a subxiphoid approach using either the single- or double-stick method. Once the PTC has been performed and the appropriate duct chosen for placement of the drainage catheter, the technical aspects of the procedure are the same as for drainage of the right system.
In general, once the initial drainage catheter is in place the procedure is terminated. This allows the parenchymal tract to mature and the biliary tree to decompress. Decompression of the system allows edema and inflammation to resolve and the ducts to return to a more normal caliber. In addition, the risk of sepsis is decreased. The catheter is fixed to the skin and placed to closed gravity drainage for at least 24 hours. Depending on the patient’s condition, the catheter may be clamped after 24 hours to allow internal drainage. Antibiotics are continued for at least 48 hours after the catheter has been placed. Further definitive intervention is usually postponed for two to five days, depending on the patient’s condition and clinical needs.
Technical variations
We have found that the most technically demanding aspect of biliary drainage in pediatric patients is the initial entry of a dilator or catheter through the wall of the biliary radicle. It is often very difficult to dilate the intrahepatic tract, penetrate the bile duct wall, and enter the lumen over a 0.018-inch guide wire. The periductal tissue is firm and a 0.018-inch wire and 3 French dilator are not rigid enough to allow significant pushing power. As a result, the catheter can buckle just outside the duct wall, within the tract, or between the surface of the liver and abdominal wall. If one is not careful, the guide wire can inadvertently be pulled out of the biliary tree or bent.
If a micropuncture set is used, the 4 French introducer dilator is well tapered for the task. Spinning the introducer while advancing into the duct will help ease it through the transitions between tissue planes. However, if the introducer cannot be advanced smoothly into the duct, coarse and forceful effort is more likely to damage the access system than to achieve success. In this event, other techniques or devices should be considered. To facilitate entry into the bile duct an 18-gauge spinal needle can be advanced over the 0.018-inch guide wire and used to make a larger hole in the bile duct wall. Alternatively, a coaxial dilator with stiffener is available or one can be fabricated by using the metal stiffener from a 5 or 6 French nephrostomy set that can be coaxially placed within a 4 French or 5 French vascular dilator that accepts at least a 0.035-inch wire (Figure 5.9). This combination is then advanced into the biliary tree over the 0.018-inch guide wire already in position. Once the tip of the system is within the bile duct the wire and stiffener are pinned as the dilator is advanced into the biliary tree. The 0.018-inch wire and the stiffener can then be removed and exchanged for a 0.035-inch or 0.038-inch wire, which is stiff enough to maintain access during subsequent dilation of the tract and placement of the drainage catheter.

Coaxial dilator with metal stiffener.
Selecting, modifying, and positioning a drainage catheter depends upon four principal factors. The first is the intended position of the catheter tip. Usually, the tip of the drainage catheter is a locking pigtail and is placed through the stricture and into the small bowel by way of the common bile duct or the biliary–enteric anastomosis, as applicable. If the stricture or the anastomosis cannot or should not be crossed during the initial procedure, and there is space in the dilated system to form a loop, then the pigtail may be left on the access side of the stricture, rather than the enteric side. Occasionally, the catheter must be advanced through the stricture in a retrograde fashion, either from the contralateral ducts or from an enteric-to-biliary approach, or left on the access side of the stricture where there may be insufficient space to form a loop (for example, when leaving a drain pulled back across a treated stricture until durable preservation of ductal diameter is proven). If the end of the drainage catheter must be left in a non-dilated duct where there is insufficient room to form a loop, the loop may be trimmed off the drainage catheter, understanding that such a modified catheter should be delivered through a sheath, to avoid traumatizing the duct with the rough-cut tip of the catheter.
The second important factor is the distance from the skin to the intended catheter endpoint. This factor will govern the necessary length of the catheter. The shortest catheter that can fulfill this requirement should be used, to minimize the external length of the catheter, and thus the opportunity for accidental dislodgment. The length of the catheter can be sized using the modified “bent guide wire” technique described in Chapter 2.
The third factor, and usually the least critical, is the optimal diameter of the drainage catheter. An 8 to 10 French catheter will suffice in most circumstances. Occasionally, a larger diameter catheter will be useful to stent a healing stricture after therapeutic interventions.
The fourth factor is the intended drainage pathway. The key to optimizing this factor is consideration of where bile is coming from and to where it should be going. If the drainage catheter is across the stricture, then side holes will be required on both sides of the stricture. If the selected catheter is not manufactured with such side holes then they must be added to the catheter shaft. This is most effectively done by creating holes no larger than the end hole of the catheter, in a spiral pattern around the shaft where it will lie on the access side of the stricture, while not extending into the hepatic parenchyma or across the capsule. If the drain is to be left on the access side of the stricture or obstruction, then side holes in the loop or end of the catheter are sufficient.
Whatever the internal configuration, the external portion of the drain should be fixed securely to the skin so as to prevent accidental dislodgment, and should be fixed in line with the access tract so as to prevent kinking of the catheter.
Postprocedure and follow-up care
The biliary drain should be flushed regularly (two to three times per day) with sterile saline. Manipulation of the catheter, including flushing, may be deferred in the initial period after accessing an obstructed system until after at least 48 hours of external drainage to reduce the risk of biliary sepsis. Daily output of any drain is monitored and recorded in the patient record. If the drain has side holes on either side of a stricture, it may be converted to a trial of internal drainage after 48 hours.
Complications
Complications of percutaneous biliary drainage may be either acute or delayed in onset. Acute complications occur in 5 to 10% of patients. Postprocedural sepsis is the most common acute complication and is due to release of bacteria and endotoxins into the lymphatic and venous circulations. The most commonly encountered bacteria are E. coli and Enterobacter, although Klebsiella, Pseudomonas, and Enterococcus are also relatively common. Prophylactic antibiotics are given prior to and for 48 hours after the procedure, as for PTC.
Hemorrhage is another potential acute complication. It is common to see blood-tinged bile immediately after the placement of a drainage catheter, which usually resolves within the first 24 hours. Bleeding may be intraperitoneal as a result of liver laceration, inadvertent puncture of extrahepatic vessels during PTC, or multiple punctures of the liver capsule. The most common manifestation results from inadvertent transgression of intrahepatic vessels, expressed as hemobilia, which can be seen as either bright-red blood through the drainage catheter or, less frequently, as hematochezia or melena. If bright-red blood is seen coming from the drainage catheter one easily remedied cause is the incorrect position of one or more side holes in the liver parenchyma in direct communication with a vascular channel. All that is required in that case is to reposition the catheter, confirming with a contrast injection that all the side holes are intraductal in position.
If the catheter is in good position then it must be assumed that the bleeding is a result of a biliary-arterial or biliary-venous fistula that occurred during catheter placement, seen in up to 33% of patients undergoing percutaneous biliary drainage. Clinical evidence of bleeding is seen in approximately 6% of these cases and is due to hepatic artery pseudoaneurysms (the most common cause), hepatic artery–portal vein fistulae, and varices along the transhepatic tract. One way to treat the hemobilia is to clamp the catheter and allow clotting within the biliary tree to tamponade the bleeding. Another approach is to change the catheter to a larger size to tamponade the tract, or in resistant cases to attempt direct tamponade of the bleeding vessel by gently inflating a PTA balloon catheter across the fistula.
If hemobilia persists or is severe, hepatic angiography with transcatheter embolization may be necessary to stop the bleeding. Procedurally, there are several measures that can be taken to reduce the risk of creating these vascular lesions. Patients with coagulopathy should be aggressively corrected prior to the procedure. The operator should attempt to puncture the duct peripherally so that the transhepatic tract, if at all possible, does not enter the more vascular central portion of the liver. While the number of passes through the liver with fine-gauge needles does not appear to affect the complication rate, multiple passes with larger gauge needles have been shown to increase the risk of both bleeding and bile leak.
Minor bile leak is probably present in most patients who have undergone PTD, but the vast majority of children remain asymptomatic and require no intervention. Inadvertent puncture of an extrahepatic duct or the gallbladder or multiple punctures of the liver capsule may predispose to this complication, but the same precautions that apply to reducing the risk of hemorrhage also apply here. Only rarely does bile peritonitis occur, and if it does placement of a peritoneal drainage catheter may be all that is necessary.
Pleural complications such as pneumothorax, hemothorax, and biliary–pleural fistula are uncommon. The parietal pleura often extends substantially lower than the fluoroscopically observed costophrenic sulcus, and any puncture performed along the mid-axillary line at, or cephalad to, the tenth intercostal space invariably transgresses the pleural space. Pleural complications may be avoided by choosing a puncture site closer to the anterior axillary line. However, this may make it more difficult to puncture a biliary duct.
In general, the best protection against acute complications is successful placement of a secure drainage catheter. Adequate decompression of the biliary tree decreases the risk of continued cholangitis and bile leak. Major hemorrhage and pleural complications are much less likely if an indwelling catheter tamponades the transhepatic tract. Failure to establish adequate drainage in an obstructed biliary tree, and similarly, early dislodgment of the catheter before a mature fibrous tract is formed, frequently lead to complications. Loss of the drainage catheter from an obstructed system in the immediate postprocedure period should be considered an emergency and a new catheter placed as soon as possible.
The risk of acute complications may be decreased by meticulous attention to proper technique, but delayed complications are not only much more difficult to avoid but also more likely the longer the catheter is in place. Catheter malfunction, usually due to blockage or migration, is the most common delayed complication. For the most part, if problems are recognized early they can be treated on an outpatient basis and have no significant or long-term sequelae. Early detection of these problems depends principally upon how well the patient or the patient’s caretakers understand how a biliary drain works, how to properly care for the catheter, how to recognize the signs of catheter malfunction, and what to do when a problem is identified.
A blocked catheter, which is most often noticed because of bile leakage around the catheter, needs to be exchanged. Catheters that have migrated do not drain optimally and need to be adjusted or, in most cases, exchanged. Obviously, if the catheter becomes completely dislodged it needs to be replaced. After ten to fourteen days of catheter drainage, the mature fibrous tract that forms around the catheter makes replacement relatively easy. In case of catheter dislodgment replacement should be performed as soon as possible, at least within 24 hours.
Delayed cholangitis may also result from catheter malfunction. Usually catheter exchange and antibiotic therapy will be sufficient treatment. If there are persistent or recurrent bouts of cholangitis then the possibility of independently obstructed segments, newly obstructed segments, or liver abscess should be considered and the appropriate imaging done to determine the diagnosis and direct further intervention.
Infrequently, delayed hemorrhage can occur weeks to months after the initial procedure. The etiologies of delayed bleeding include mycotic arteritis as a result of tract infection and pressure erosion of an adjacent blood vessel by the drainage catheter. Usually bleeding occurs during a routine catheter change as the old catheter is removed. The placement of a new catheter will usually tamponade the bleeding vessel and stop hemorrhage, but occasionally transcatheter embolization may be required for treatment.
Overall, the incidence of major complications in the adult population is 5 to 10% and the mortality rate is 2%. However, these statistics are derived from studies in which the majority of patients had malignant obstructions. There is a significantly lower complication rate among patients with benign disease, presumably because of the shorter duration of drainage required and because the overall health of patients with benign obstructions is better than those with malignant obstructions. In patients with benign etiologies of biliary strictures the expected rate of major complications is around 2% and the mortality rate is near zero. The complication rates in the pediatric population are generally lower in our experience; however, there are few studies available to provide objective confirmation.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree