(1)
Radiology Department Beijing You’an Hospital, Capital Medical University, Beijing, People’s Republic of China
18.1.1 Pericardial Disease
18.1.2 Pulmonary Hypertension
18.1.3 Myocarditis
18.1.4 Dilated Cardiomyopathy
18.1.5 Cardiac Neoplasm
18.2.1 Pathogens and Pathogenesis
18.2.2 Pathophysiological Basis
18.2.3 Clinical Symptoms and Signs
18.2.5 Imaging Demonstrations
18.2.6 Criteria for the Diagnosis
18.2.7 Differential Diagnosis
18.3.1 HIV/AIDS Related Myocarditis
18.3.3 Discussion
18.6.2 Pulmonary Hypertension
18.6.3 Vasculitis
Abstract
Cardiovascular diseases occur in patients with AIDS of its advanced stage. The cardiovascular complications include dilated cardiomyopathy, pericardial effusion, endocarditis, cardiac dysfunction, pulmonary hypertension and arrhythmia. Left ventricular dysfunction is more common in the advanced stage. Since the year of 1981, there has been increasingly clinical and autopsy reports about AIDS complicated by cardiopathy, with the most frequently reported cases of pericarditis or pericardial effusion and occasionally accompanying cardiac tamponade. In adults and children AIDS patients, about 20–40 % is found to have pericarditis. According to the autopsy reports, the incidence of pericardiac lesions is 3–37 %, while its incidence by echocardiography is 30–38 %. HIV/AIDS related cardiopathy is a kind of non-inflammatory heart disease that is related to dysmetabolism. Myocardium is the basic dynamic tissue for the contraction and relaxation of the heart, and it is particularly sensitive to infections, hypoxia, drugs and toxins. Among AIDS patients, dilated and hypertrophic myocardial diseases are more common. By myocardium tissue culture, HIV can be found, although some scholars believed that HIV attacks hemoglobin instead of myocardial tissue. In 5 % cases of myocarditis in AIDS patients by autopsy, only 20 % is pathologically confirmed as having dilated myocardiopathy. By electrocardiography, 30–45 % cases of AIDS complicated by cardiopathy show abnormalities.
18.1 An Overview of HIV/AIDS Related Cardiac Diseases
Cardiovascular diseases occur in patients with AIDS of its advanced stage. The cardiovascular complications include dilated cardiomyopathy, pericardial effusion, endocarditis, cardiac dysfunction, pulmonary hypertension and arrhythmia. Left ventricular dysfunction is more common in the advanced stage. Since the year of 1981, there has been increasingly clinical and autopsy reports about AIDS complicated by cardiopathy, with the most frequently reported cases of pericarditis or pericardial effusion and occasionally accompanying cardiac tamponade. In adults and children AIDS patients, about 20–40 % is found to have pericarditis. According to the autopsy reports, the incidence of pericardiac lesions is 3–37 %, while its incidence by echocardiography is 30–38 %. HIV/AIDS related cardiopathy is a kind of non-inflammatory heart disease that is related to dysmetabolism. Myocardium is the basic dynamic tissue for the contraction and relaxation of the heart, and it is particularly sensitive to infections, hypoxia, drugs and toxins. Among AIDS patients, dilated and hypertrophic myocardial diseases are more common. By myocardium tissue culture, HIV can be found, although some scholars believed that HIV attacks hemoglobin instead of myocardial tissue. In 5 % cases of myocarditis in AIDS patients by autopsy, only 20 % is pathologically confirmed as having dilated myocardiopathy. By electrocardiography, 30–45 % cases of AIDS complicated by cardiopathy show abnormalities.
Endocardial diseases may occur in AIDS patients. The more commonly endocardial diseases in AIDS patients include non-bacterial endocarditis and infectious endocarditis. Infectious endocarditis can be caused by pathogens of bacteria, fungi, mycobacterium and protozoa, with symptoms of fever, anorexia, upset, chest pain and weight loss.
HIV/AIDS related cardiac diseases include:
18.1.1 Pericardial Disease
The pericardium is the most commonly involved part of heart in HIV/AIDS patients. In the early stage of HIV infection, pericardial lesions may occur, but being asymptomatic during his/her life time. HIV/AIDS related pericarditis caused by tuberculous mycobacteria infection is the most common. Staphylococcus and streptococcus are also the common causes of pneumonia and pericarditis. Others pathogens including Nocardia and Listeria can also cause pericarditis. HIV/AIDS related pericarditis has a poor prognosis, with the CD4 T cell count being lower than 100/μl.
18.1.2 Pulmonary Hypertension
AIDS and left ventricular dysfunction, valvular heart disease or cardiac shunt can cause pulmonary hypertension and pulmonary heart disease. Patients with AIDS complicated by pulmonary hypertension mostly sustain serious pulmonary infection, such as Pneumocystis carinii pneumonia and cytomegaloviral pneumonia. Progressive pulmonary pressure in AIDS patients is caused by hyperplasia of pulmonary endothelial cells resulted from stimulation of growth factors to pulmonary endothelial cells. It has been recognized that growth factors can be derived from infected T cells or directly derived from HIV. Therefore, occurrence of dyspnea in AIDS patients shows evidence of right ventricular dysfunction instead of left ventricular dysfunction. In such cases, possible occurrence of pulmonary hypertension should be considered.
18.1.3 Myocarditis
HIV/AIDS related myocarditis plays an important role in progressive left ventricular dysfunction. About 80 % cases of myocarditis is idiopathic and about 20 % is opportunistic. The pathogen usually includes the complex of tubercle bacillus and mycobacterium avium, fungi including cryptococcus, aspergillus, Candida albicans, Histoplasma capsulatum and Coccidiodes, and protozoa including Cytomegalovirus, simplex herpes virus and HIV.
18.1.4 Dilated Cardiomyopathy
HIV/AIDS related dilated cardiomyopathy may be caused by diffuse weakened mobility of myocardium due to myocarditis. The diffuse weakened mobility of myocardium causes compensatory hypertrophy and dilation of the ventricles, and finally progresses into dilated cardiomyopathy.
18.1.5 Cardiac Neoplasm
18.1.5.1 Kaposi’s Sarcoma
Kaposi’s sarcoma is common in AIDS patients, and usually involves myocardium and epicardium. Generally, cardiac KS is found during autopsy, being asymptomatic during the patient’s lifetime. According to data from the autopsy, foci of KS are found in about 28–40 % AIDS patients, involving all parts of heart including heart apex, interventricular septum, pericardium, aortic adventitia and pulmonary artery trunk. The foci of KS can be patchy or nodular.
18.1.5.2 Malignant Lymphomas
Cardiac malignant lymphoma is more common than KS in AIDS patients. For cases with lymphoma with involvement of pericardium, pericardial effusion can be caused. For cases with lymphoma with involvement of myocardium, arrhythmia and conduction block can occur to cause congestive heart failure. Occasionally, lymphoma invades into cardiac chambers to cause blockage of the blood flow. Patients with cardiac lymphoma cannot be pathologically diagnosed during his/her lifetime.
18.1.6 Valvular Heart Disease and Pulmonary Vascular Disease
In AIDS patients, some vascular diseases may occur. HIV/AIDS related cardiopathy is common and dilated cardiomyopathy can also occur as one of the cardiac complications of AIDS. The common cardiovascular diseases that complicate AIDS are myocarditis, cardiomyopathy, pericarditis and pericardial effusion, abnormal heart valves, vascular diseases and neoplasms. In cases of pulmonary infections, the pulmonary vascular intima responds to lesions, mostly caused by HIV under effects of inflammatory mediators and cytokines. The endothelial cells can release vasoactive substances or trigger proliferative response to growth factors to cause the increase of pulmonary vascular resistance. Calabrese et al. reported four cases of AIDS patients, with occurrence of necrotic vasculitis [5]. The lesions were reported to be nodular arteritis and acute inflammation of small and medium-sized blood vessels, resulting in lesions of the skin, muscles and nerve fibers. There were two cases with such lesions occurring in the nervous system, with their clinical and morphological manifestations being in line with those of neurologic granulomatous vasculitis. The pathogenesis of vasculitis is still unknown, and it may be related to the effects of virus (HIV, CNV, HBV and EBV) or immune complexes to cause vascular lesions, opportunistic infections, pulmonary diseases, drugs and nutritional status. Autopsy of AIDS patients found inflammatory and fiber calcified arterial lesions. The inflammatory arterial lesions are vasculitis and peripheral inflammation, while fiber calcified arterial lesions often involve medium sized artery to cause arterial intimal fibrosis, elastic fiber breakage, arterial medial fibrosis and calcification, possibly with accompanying varying degrees of stenosis. In addition, aneurysm can be found in some AIDS patients, with vascular wall fibrosis and calcification as well as endothelial cell proliferation, with accompanying arterial stenosis of different degrees. Changes in the microcirculation have been studied, but the abnormalities and their significance still need clarifying.
18.2 HIV/AIDS Related Pericarditis and Pericardial Effusion
Pericarditis and pericardial effusion are the common complications of AIDS. Pericardial effusion is often ignored in the early stage. For cases of AIDS patients with sinus tachycardia and dyspnea, the possibility of pericardial effusion should be considered. Echocardiography is recommended for the diagnosis and should be performed as early as possible. AIDS complicated by pericardial effusion mostly occurs in those with tuberculous serous cavity effusions, possibly progresses into pericardial tamponade in the advanced stage. Since the first case of AIDS reported in 1981, there were clinical and autopsy reports about the cardiac abnormalities in AIDS patients, among which the most common cardiovascular disease is pericarditis or pericardial effusion, with the symptom of cardiac tamponade. It is estimated that 5–10 % HIV infected patients in America have pericardial effusion, but mostly being asymptomatic and obtaining their definitive diagnosis by echocardiography or autopsy. According to autopsy reports, the incidence of pericardial disease is 3–37 %; and the incidence of pericardial effusion is 30–38 % by echocardiography.
18.2.1 Pathogens and Pathogenesis
In cases of acute pericarditis, infections can be caused by bacteria, parasites, protozoa, viruses and fungi. The pathogens of bacterial infections are commonly streptococcus, staphylococcus and Gram-negative bacilli. The pathogens of virus infections in immunocompromised patients are commonly Echovirus, influenza virus, and Coxsackie B virus. AIDS can be complicated by pericardial effusion due to infections of tuberculous mycobacterium avium, actinomyces, fungi or virus, lymphoma and Kaposi’s sarcoma.
The common subtypes of chronic pericarditis are chronic constrictive pericarditis and chronic exudative pericarditis.
Chronic constrictive pericarditis is usually non-specific, but almost all subtypes of acute pericarditis can be its cause. The common cause is tuberculosis or other infection, rheumatoid arthritis, trauma and heart surgery.
Chronic exudative pericarditis is usually non-specific, but can be caused by mycobacterium tuberculosis, fungi or neoplasm. Among inpatients, the most common cause of large quantity pericardial effusion is the metastatic tumors or direct spreading of tumors, such as cancer (especially lung cancer or breast cancer), sarcoma (especially melanoma), leukemia, lymphoma and thoracic tumors.
18.2.2 Pathophysiological Basis
Acute pericarditis can be serous, fibrinous, hemorrhagic or suppurative. It may involve surface of the sub-picardial myocardium. The quantity and quality of the cellular responses are determined by pathogens.
Chronic pericarditis can be serous, chylous or blood exudative. Alternatively, chronic pericarditis can be fibrinous, adhesive or calcified. And it can be constrictive and asymptomatic. In cases of chronic exudative pericarditis, the pericardial effusion fluid is about 50–1,000 ml (normally less than 25 ml). In the cases of less but rapid pericardial effusion, more but slow pericardial effusion, decreased accommodation of the pericardium due to fibrosis, calcification and neoplasm, the ventricular filling during its diastole can be restricted. Under such conditions, the terminal pressure of the left ventricular diastole is determined by the quantity of pericardial effusion and the thickness of the thickened pericardium. The diastolic pressures of ventricles, atria and venous bed are close, usually being 13–32 mmHg. Occurrence of venous congestion of systemic circulation causes too much body fluid effusion from the capillaries, resulting in postural edema and later ascites. The sign of surrounding tissue congestion is more obvious than that of pulmonary congestion, but pulmonary edema with obvious clinical symptoms is not common. However, pericardial effusion gradually progresses and the quantity of effusion being up to more than 1,000 ml may fail to cause pericardial tamponade due to its elasticity for adaptation.
Pathologically, pericarditis can be divided into two stages of the fibrinous stage and the serofibrinous stage. In the early stage of pericarditis, parietal and visceral pericardium has congestion, swelling and effusions of fibrin, leukocyte and some endothelial cells. The thick exudates can be restricted to a certain part of pericardium or diffuse across the entire surface of the heart. The surface of the pericardium can be coarse. In the cases of increased exudates, the effusion fluid can be serofibrinous effusions, with its quantity varying from 100 to 2,000–3,000 ml. The sub-epicardial myocardium often has inflammatory changes. After being cured, the exudates can be reabsorbed within 2–3 weeks or shorter time period. But in some cases, the exudates may remain for several days or even years, such as in the cases of tuberculous pericarditis. When pericardium recedes, varying degrees of adhesion may remain. Sometimes, both layers of pericardium can be obviously thickened and adhesive to completely fill the pericardial cavity. Therefore, thick and hard scars form to compress the heart and the major vascular roots. The cardiac diastole is therefore affected to develop into chronic constrictive pericarditis.
18.2.3 Clinical Symptoms and Signs
Acute pericarditis is manifested with symptoms of chest pain, difficulty breathing, fever, pericardial friction sound, pericardial tamponade, chest or retrosternal dull or sharp pain that radiates to the neck, trapezius (especially the left side) or the shoulder. The severity of the pain varies, commonly aggravating at conditions of chest motion, coughing and breathing and alleviating at the postures of standing up from sitting and leaning forward. Fever, chills and fatigue are very common. And the most important sign is three-phase or two-phase (systolic and diastolic) pericardial friction sound. For cases of large quantity pericardial effusion, the heart sound is low, with enlarged range of dullness sound. In such cases, the lungs can be compressed to cause dyspnea. About 8–30 % patients with pericarditis have symptoms of heart tamponade, with accompanying increased central venous pressure. Cardiac tamponade is fatal. Chronic pericarditis has symptoms of fever but with no chest pain.
18.2.4 Examinations and Their Selection
18.2.4.1 Echocardiography
Echocardiography is the examination of choice for HIV/AIDS related pericarditis and pericardial effusion. The demonstrations include liquid dark area within pericardial cavity. It is a diagnostic method with accuracy, safety and simple manipulations.
18.2.4.2 Electrocardiography
For the cases with pericardial effusion, QRS waves group is in low voltage.
18.2.4.3 Pericardiocentesis
Pericardiocentesis facilitates to clarify the quality of pericardial effusion. Its combination with smear and culture can detect the pathogens of the infection. For cases of neoplastic pericardial effusion, tumor cells can be detected.
18.2.4.4 Diagnostic Imaging
CT scanning and MR imaging are the effective assistant examinations, with accurate localization.
18.2.5 Imaging Demonstrations
For the cases of pericardial effusion, the imaging demonstrations include enlarged heart shadow in shape of a flask, the increased ratio of heart to chest, and the absence of outer line of the heart. Generally, when pericardial effusion reaches up to 300–500 ml or above, the heart shadow commonly expands to both sides, with different morphology of the heart shadow due to different posture. Superior vena cava obviously expands and the cardiophrenic angle becomes blunt. When pericardial effusion exceeds 1,000 ml, the heart shadow obviously expands in a shape of triangle or flask. In addition, normal limits of heart arches are absent, with weakened or no heart beat by X-ray.
Case Study 1
A male patient with AIDS aged 15 years. He was confirmatively diagnosed by CDC. He complained of fever for 1 month, with history of blood donation and symptoms of fever, cough and chest distress. His CD4 T cell count was 69/ μl.
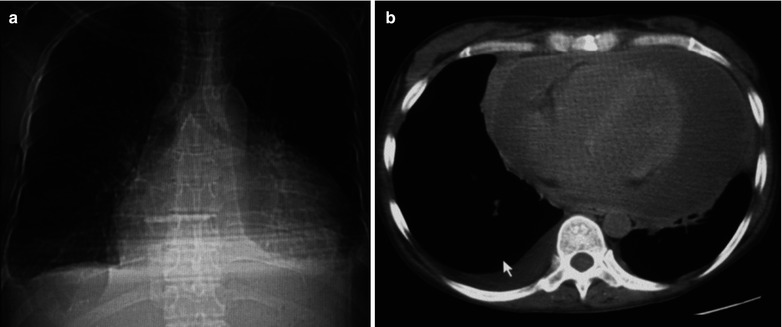
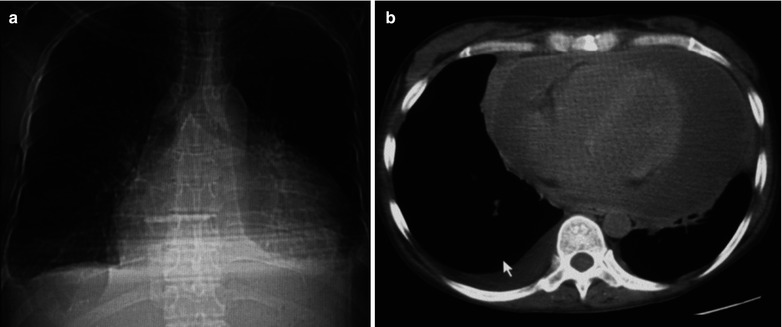
Fig. 18.1
(a, b) HIV/AIDS related pericardial effusion. (a) DR demonstrates enlarged heart shadow in shape of a flask, increased ratio of the heart to the chest, closed bilateral costophrenic angles with adhesion. (b) CT scanning demonstrates stripe liked fluid density shadow in the pericardial cavity and fluid density shadow in posterior chest wall of the right chest cavity
Case Study 2
A female patient aged 33 years was confirmatively diagnosed as having AIDS by CDC. She had a history of blood transfusion in 1996, with chief complaints of fever, cough and chest distress in 2007. Her CD4 T cell count was 46/μl.
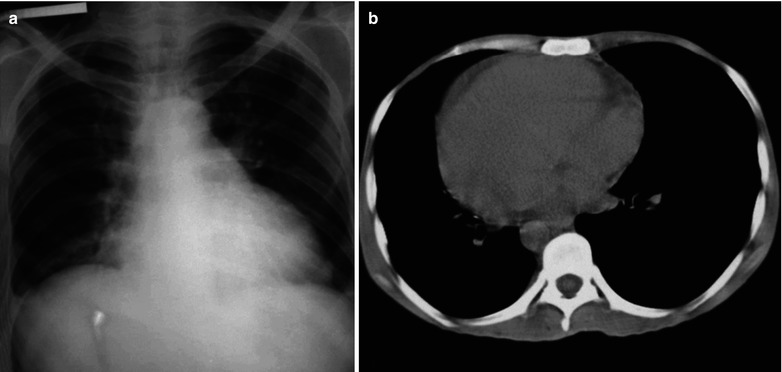
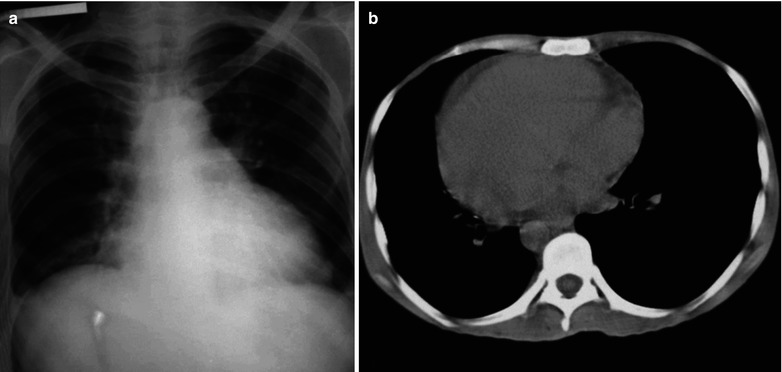
Fig. 18.2
(a, b) HIV/AIDS related tuberculous pericarditis. (a) DR demonstrates enlarged heart shadow in shape of a flask and increased ratio of the heart to the chest. (b) CT scanning demonstrates stripe liked fluid density shadow in the pericardial cavity
Case Study 3
A female patient aged 38 years was confirmatively diagnosed as having AIDS by CDC. She had a history of blood transfusion in 1995, and complained of fever, cough, expectoration and chest distress in 2007. Her CD4 T cell count was 46/μl.
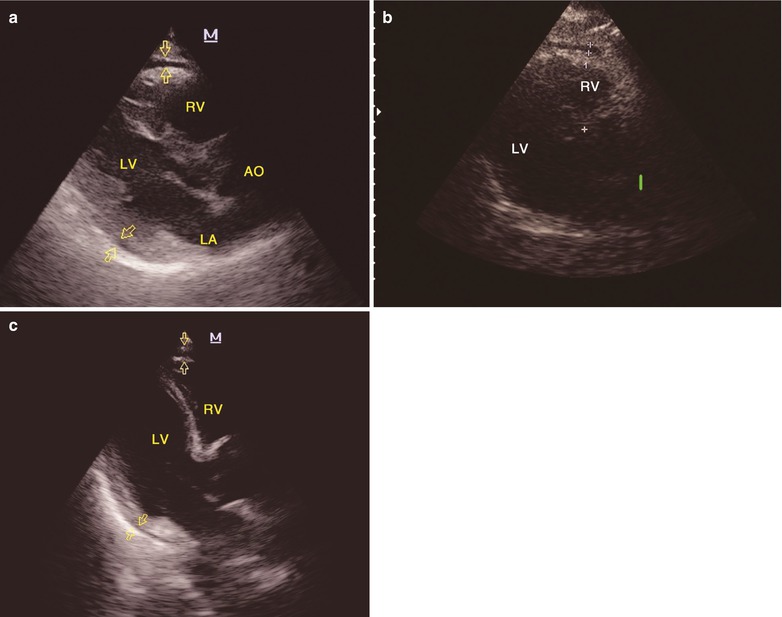
Fig. 18.3




(a–c) HIV/AIDS related pericardial effusion. (a–c) Color Doppler ultrasound demonstrates long axis cross section of the left ventricle: fluid dark area of 7 mm in width in the pericardial cavity and the posterior wall of the left ventricle, fluid dark area of 5 mm in width in the anterior wall of the right ventricle, with favorable echoes. AO aorta opening, LA left atria, LV left ventricle, RV right ventricle
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree