(1)
Radiology Department Beijing You’an Hospital, Capital Medical University, Beijing, People’s Republic of China
23.1.2 Abscesses
23.1.3 Osteomyelitis
23.1.4 Ischemic Necrosis
23.1.5 Rheumatic Diseases
23.1.6 Neoplasms
23.2.1 Pathogens and Pathogenesis
23.2.2 Pathophysiological Basis
23.2.3 Clinical Symptoms and Signs
23.2.5 Imaging Demonstrations
23.2.6 Diagnostic Basis
23.2.7 Differential Diagnosis
23.3.1 Pathogen and Pathogenesis
23.3.2 Pathophysiological Basis
23.3.3 Clinical Symptoms and Signs
23.3.5 Imaging Demonstrations
23.3.6 Diagnostic Basis
23.3.7 Differential Diagnosis
23.4.1 Pathogen and Pathogenesis
23.4.2 Pathophysiological Basis
23.4.3 Clinical Symptoms and Signs
23.4.5 Imaging Demonstrations
23.4.6 Diagnostic Basis
23.4.7 Differential Diagnosis
23.5.1 Pathogen and Pathogenesis
23.5.2 Pathophysiological Basis
23.5.3 Clinical Symptoms and Signs
23.5.4 Imaging Demonstrations
23.5.5 Diagnostic Basis
23.5.6 Differential Diagnosis
23.7.1 Pathogen and Pathogenesis
23.7.2 Pathophysiological Basis
23.7.3 Clinical Symptoms and Signs
23.7.5 Imaging Demonstrations
23.7.6 Diagnostic Basis
23.7.7 Differential Diagnosis
23.8.1 Pathogen and Pathogenesis
23.8.2 Pathophysiological Basis
23.8.3 Clinical Symptoms and Signs
23.8.5 Imaging Demonstrations
23.8.6 Diagnostic Basis
23.8.7 Differential Diagnosis
23.9.1 Pathogen and Pathogenesis
23.9.2 Pathophysiological Basis
23.9.3 Clinical Symptoms and Signs
23.9.5 Imaging Demonstrations
23.9.6 Diagnostic Basis
23.9.7 Differential Diagnosis
Abstract
In recent years, the widespread use of immunosuppressive therapy and supportive therapy prolong the survival period of AIDS patients. Therefore, chronic immunosuppression occurs, including various inflammatory diseases and arthritis, which is possibly related to HIV infection
23.1 An Overview of HIV/AIDS Related Musculoskeletal Diseases
In recent years, the widespread use of immunosuppressive therapy and supportive therapy prolong the survival period of AIDS patients. Therefore, chronic immunosuppression occurs, including various inflammatory diseases and arthritis, which is possibly related to HIV infection
Soft tissue diseases and skeletal diseases in AIDS patients are rarely reported, which is related to the less common occurrence of skeletal complications than central nervous complications and respiratory complications. However, musculoskeletal diseases are possibly the initial disease of AIDS, which should be paid focused attention. Due to its less common occurrence, less attention is paid on musculoskeletal complications and delayed treatment. Therefore, its progression is accelerated. The diagnostic imaging is important for the early diagnosis of musculoskeletal infectious diseases. In this chapter, we focus on the diagnostic imaging of HIV/AIDS related musculoskeletal diseases.
23.1.1 Muscular and Soft Tissue Infections
Myositis may occur secondary to various bacterial infections. In the cases with no trauma and osteomyelitis, the volume, morphology, CT value and MRI signal can be varying, with normal subcutaneous adipose tissue or with lymphedema and cellulitis. Muscular necrosis occurs at sterile conditions or secondary to/complicated by bacterial infections. MR imaging is more sensitive to CT scanning in demonstrating muscular and facial changes, which facilitate the differentiation from superficial non-necrotic soft tissue inflammation.
23.1.2 Abscesses
Soft tissue abscess is usually liquid accumulation with clear boundary and thick wall. The surrounding soft tissue has inflammatory responses. The diagnostic imaging plays an important role in defining the location and range of soft tissue abscesses, which can also guide the puncture of abscesses for biopsy and drainage. Especially CT scanning and MR imaging, both have definitive demonstrations for the diagnosis. One of the main causes of abscesses in HIV positive patients is their sharing of needles for intravenous drug use. Other causes include blood borne spreading and direct spreading from adjacent osteomyelitis or purulent arthritis. The pathogenic bacteria of abscesses include Staphylococcus aureus, purulent streptococcus, Salmonella, tubercle bacilli and atypical mycobacteria. The range and progression of abscesses are dependent on the immunity status of the patients.
23.1.3 Osteomyelitis
Osteomyelitis is one of the common complications of skeletal infection, which commonly occurs in the progressive period of HIV infection. It has a rapid progression but hideous symptoms. And its pathogenic bacteria are commonly Staphylococcus aureus and Salmonella.
23.1.4 Ischemic Necrosis
Due to the immunological factors after HIV infection, vasculitis and vascular involvement can cause ischemia and necrosis of bones.
23.1.5 Rheumatic Diseases
It is still controversial concerning the correlation between rheumatic arthritis, non-purulent inflammations and HIV infection, mainly because of the etiological controversies of arthritis. Therefore, the diagnosis by radiologists is important for the therapeutic options by orthopaedic surgeons and rheumatologists. In patients with Reiter’s disease, skin and skeletal psoriasis, spinal arthritis with serological negative findings or spinal osteoarthrosis, and inexplicable facet lesions, HIV infection should be suspected.
23.1.6 Neoplasms
Along with the compromised immunity in HIV positive patients, the incidence of neoplasm is increasing. Kaposi’s sarcoma, a more common neoplasm, invades multiple organs but rarely involves the bone and bone marrow.
The prevalence of HIV infection adds new lesions for the diagnostic imaging of musculoskeletal system. The knowledge about HIV/AIDS related musculoskeletal diseases facilitates the diagnosis and differential diagnosis.
23.2 HIV/AIDS Related Osteomyelitis
23.2.1 Pathogens and Pathogenesis
After any part of human body is infected, the pathogen can involve the bone marrow, bone and periosteum along with blood flow and spread to the surrounding soft tissue. In the osteoblasts, the bacteria can directly invade the bone marrow to cause osteomyelitis. Its spreading is mainly via the following three transmission routes: (1) Blood borne infection has an inappropriately treated purulent infective lesion before its onset. The transmission route is that the bacteria gain their access to the bone tissue along with blood flow to cause osteomyelitis. (2) Traumatic infection is caused by the direct invasion of the pathogenic bacteria to the bone tissue, leading to osteomyelitis. (3) Spreading infection is caused by direct spreading of the adjacent purulent lesions to the bone tissues to cause osteomyelitis.
23.2.2 Pathophysiological Basis
When the immunity is compromised, local inflammation shows an acute onset to form large quantity pus fluid and invade the periosteum and bone marrow, resulting in osteomyelitis. Chronic purulent osteomyelitis repeatedly occurs, with newly formed dead space and necrotic bone during each period of attack to complicate the dead cavities and sinuses. Meanwhile, due to the long term local deficiency in blood supply and repeated inflammatory stimulations, local bone hyperplasia and sclerosis occur.
23.2.3 Clinical Symptoms and Signs
The symptoms of acute osteomyelitis are local redness and swelling, fever, pain, hard lump with limited mobility. The symptoms of chronic osteomyelitis include trauma surface erosion, white and foul secretion at the opening of the fistula. In the serious cases, the bone is destructed and cannot heal in a long period of time. Necrotic bones, sinuses or dead spaces are formed, with discharge of necrotic osteocomma from the sinus tract.
23.2.4 Examinations and Their Selection
23.2.4.1 Laboratory Tests
The blood WBC count can be normal, but ESR and C reactive protein increase.
23.2.4.2 X-ray
It has demonstrations of irregular thickening and sclerosis of the bone, with cavities of different sizes and necrotic bones.
23.2.4.3 CT Scanning
In the cases with unclearly defined demonstrations by X-ray, CT scanning can be ordered to define the diseased bone and paravertebral abscesses.
23.2.4.4 Biopsy
For neoplasms, biopsy can be performed for bacterial culture and drug sensitivity test.
23.2.4.5 Lipiodolography
To confirm the relation between dead bone, dead space and sinus tract.
23.2.5 Imaging Demonstrations
1.
Conventional X-ray is not sensitive to early osteomyelitis. Abnormal demonstrations can be found when peritoneum is reactive and bone is destructed to cause obvious osteolysis.
2.
CT scanning demonstrates soft tissue swelling, reactive peritoneum, intramedullary density changes, localized cortical bone erosion and rough bone trabecula.
3.
MR imaging has a sensitivity and specificity of 82–100 % and 53–94 %, respectively, in the diagnosis of osteomyelitis. There are low T1WI signal and high T2WI signal. Enhanced imaging can increase the assessment range of bone and soft tissue infections.
Case Study 1
A female patient aged 29 years was confirmatively diagnosed as having AIDS by the CDC. Her CD4 T cell count was 110/μl.


Fig. 23.1
(a–d) HIV/AIDS related tuberculous osteomyelitis. (a–d) DR demonstrates surrounding soft tissue swelling of the thumb interphalangeal joint, osteoporosis surrounding the joint, blurry joint space, worm bitten liked changes of articular facet and multiple small cystic low density areas
Case Study 2
A male patient aged 45 years was confirmatively diagnosed as having AIDS by the CDC. He had been found to be HIV antibody positive for 5 years, with complaint of joint pain for more than 20 days. He was in a chronic episode, with a history of unhealthy sexual behaviors. His CD4 T cell count was153/μl.
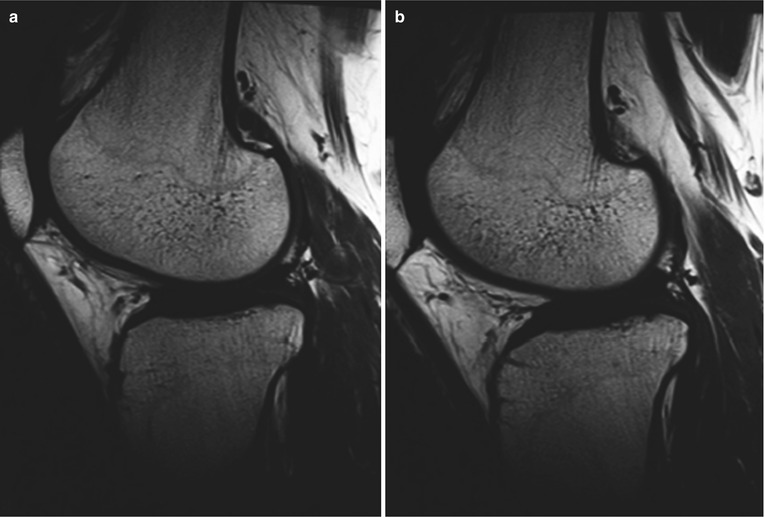
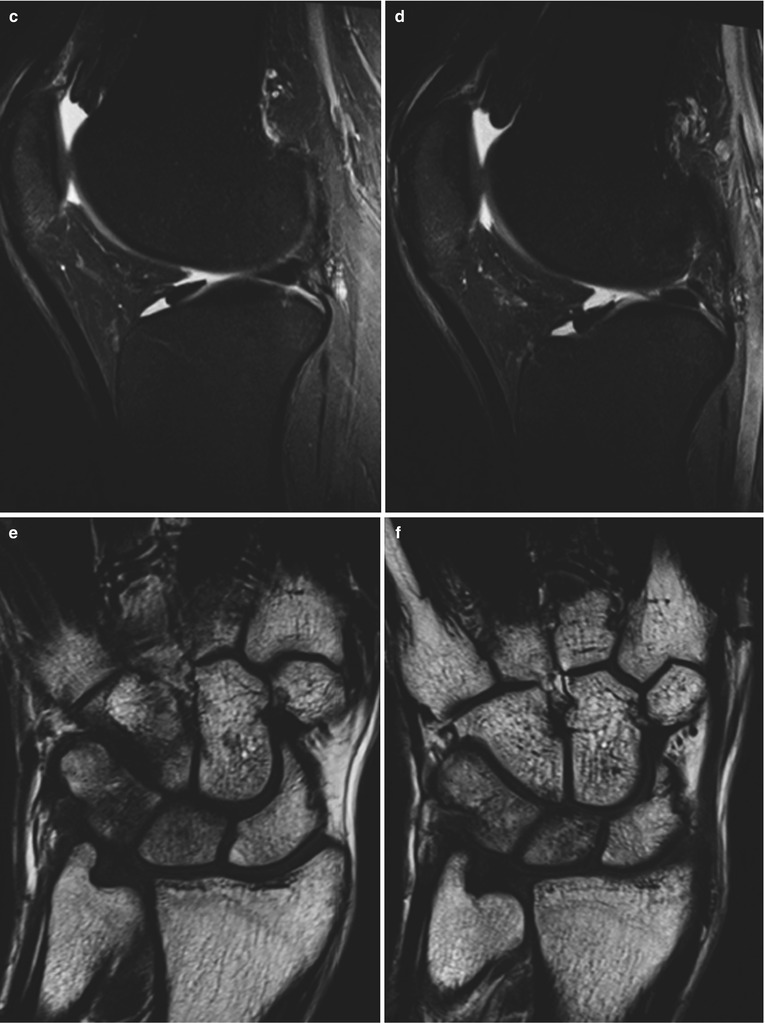
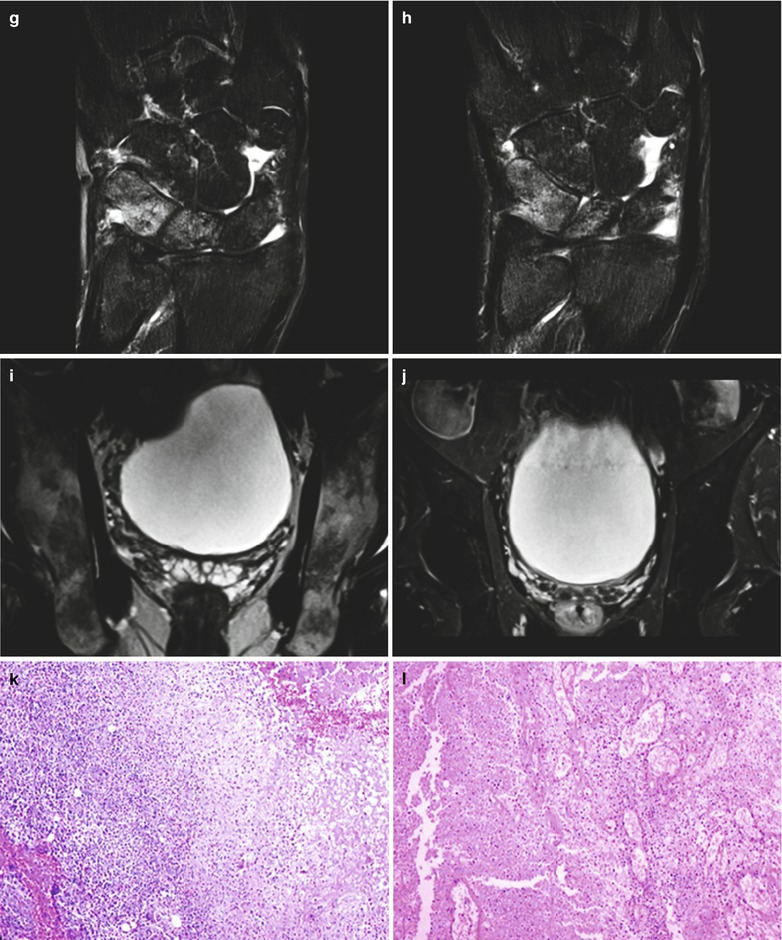
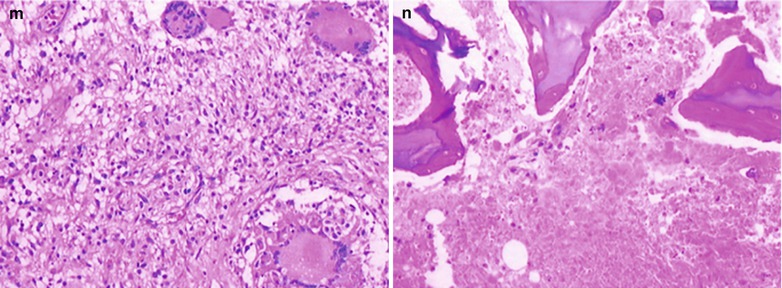
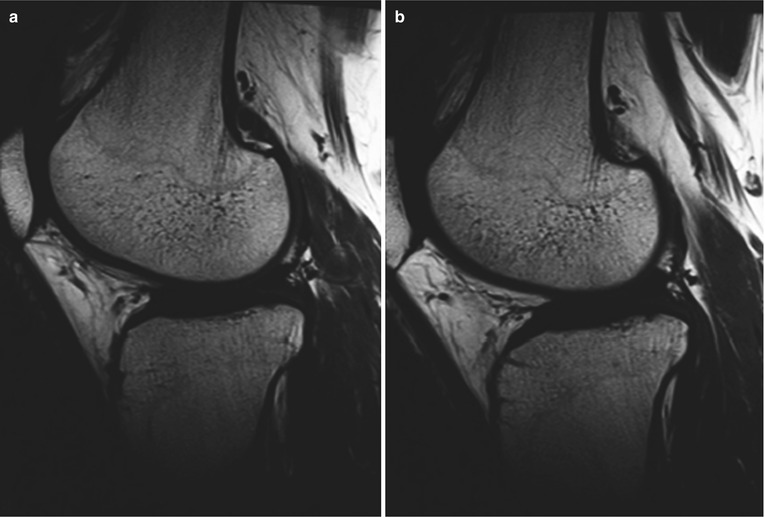
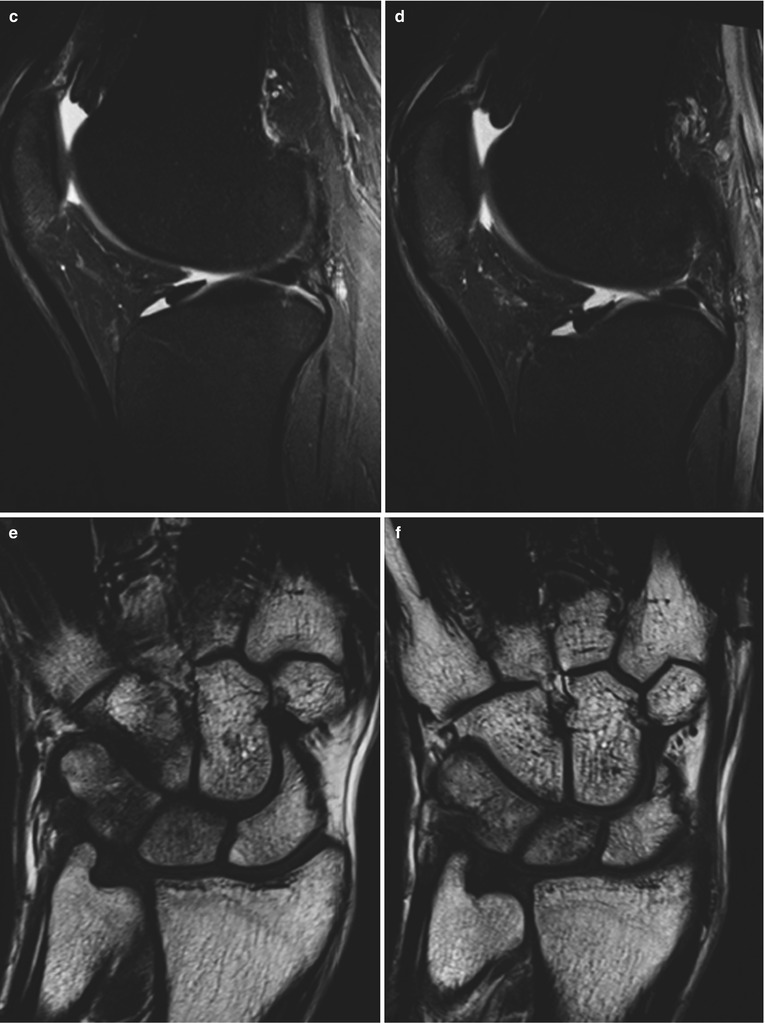
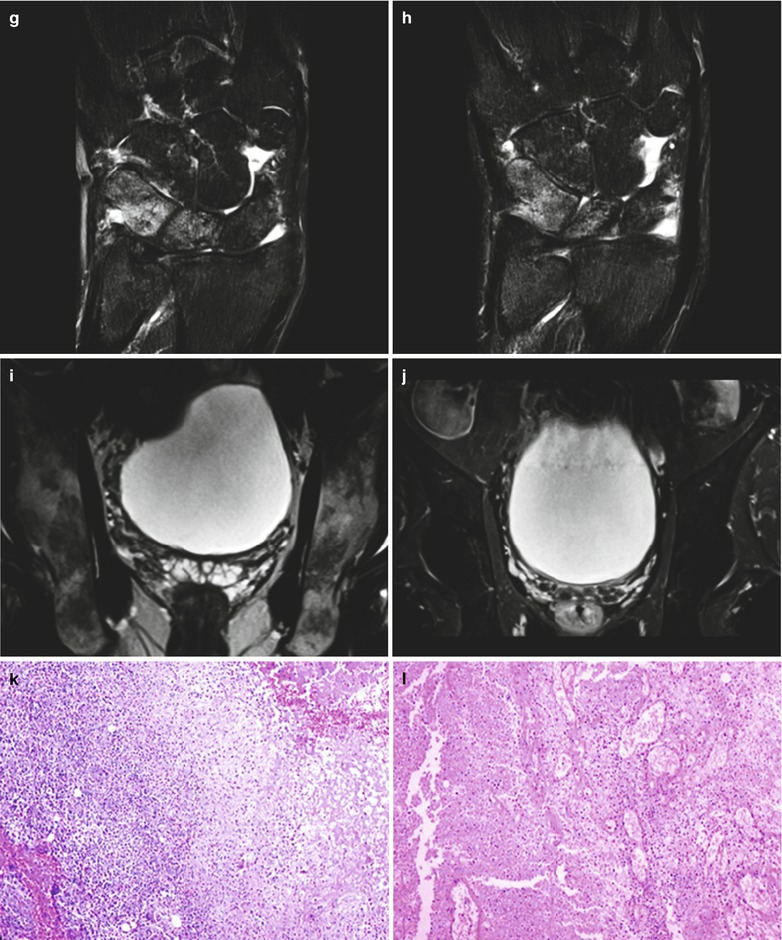
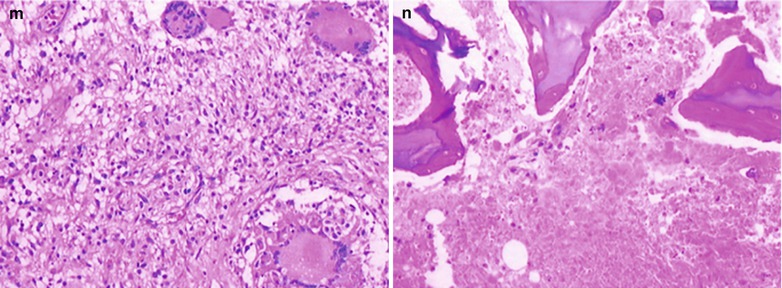
Fig. 23.2
(a–n) HIV/AIDS related gonarthromeningitis, wrist osteomyelitis and pelvic osteomyelitis. (a–d) MRI demonstrates strip liked long T1 and long T2 signal in the articular cavity of both knees. (e–h) It is demonstrated to have decreased T1WI signal in the lunate bone marrow and triangular bone marrow of the right wrist, high T2 signal after adipose suppression, intact cortical bone, strip liked long T1 and long T2 signal in the trapezoid bone, capital bone and scapholunate joint. (i–j) It is demonstrated to have strip liked long T1 and long T2 signals in the radioscaphoid joint space and extensive worm bitten liked bone destruction in the bilateral pelvic bones. (k) Microscopy at a low magnification demonstrates caseous necrosis, epithelioid cells and lymphocytes. (l) Microscopy at a low magnification demonstrates caseous necrosis and inflammatory granulation tissue. (m) Microscopy at a medium magnification demonstrates epithelioid cells and multinucleated giant cells. (n) Microscopy at a medium magnification demonstrates necrotic tissues and necrotic bones
Case Study 3
A male patient aged 38 years was confirmatively diagnosed as having AIDS by the CDC. He had a history of paid blood donation, with complaint of fever, posterior curvature of the back for 3 months and both lower limbs fatigue for 1 month. His CD4 T cell count was 26/μl.
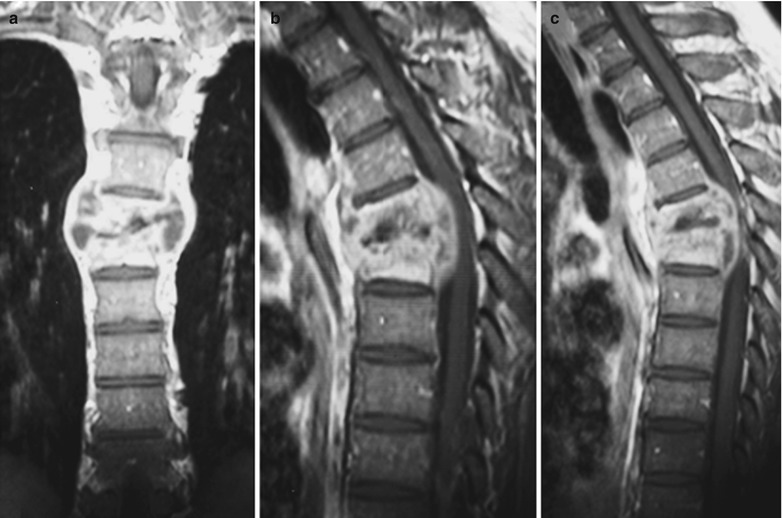
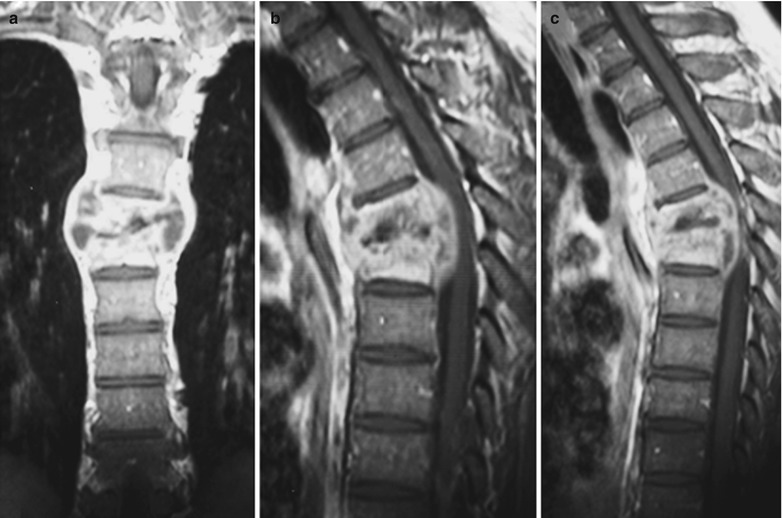
Fig. 23.3
(a–c) HIV/AIDS related extrapulmonary thoracic spinal tuberculosis. (a–b) It is demonstrated to have T7-8 vertebral compressed fracture in a wedge shape with fusion, narrowed joint space with surrounding cold abscesses to protrude into the spinal canal, and obviously compressed spinal cord. (c) Enhanced scanning of the thoracic vertebrae demonstrates patchy abnormal enhancement of the thoracic vertebrae, linear and even abnormal enhancement of the abscess wall
Case Study 4
A male patient aged 35 years was confirmatively diagnosed as having AIDS by the CDC. He had a history of paid blood donation, with complaint of fever, heel pain for 2 months. His CD4 T cell count was 406/μl.
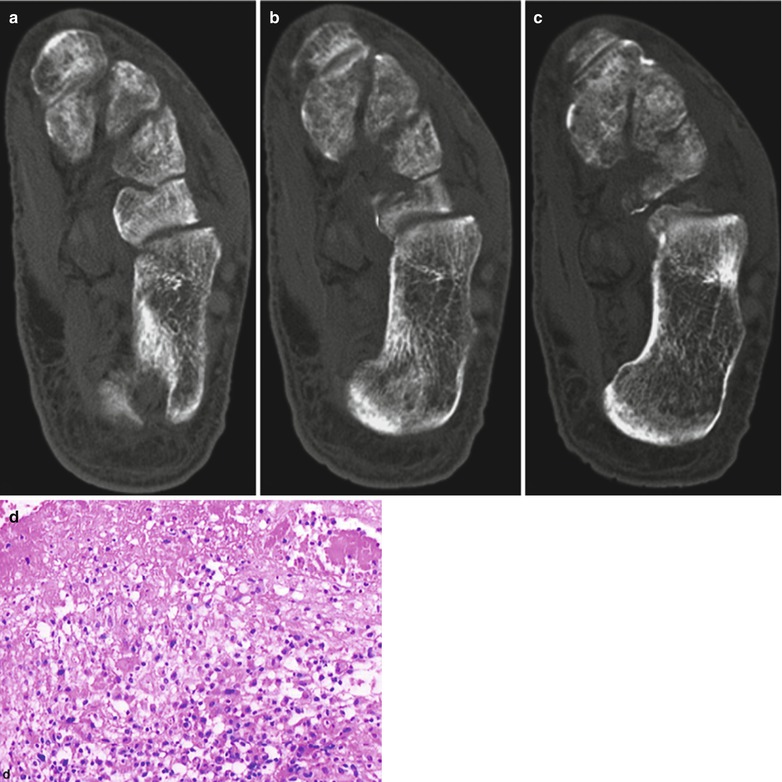
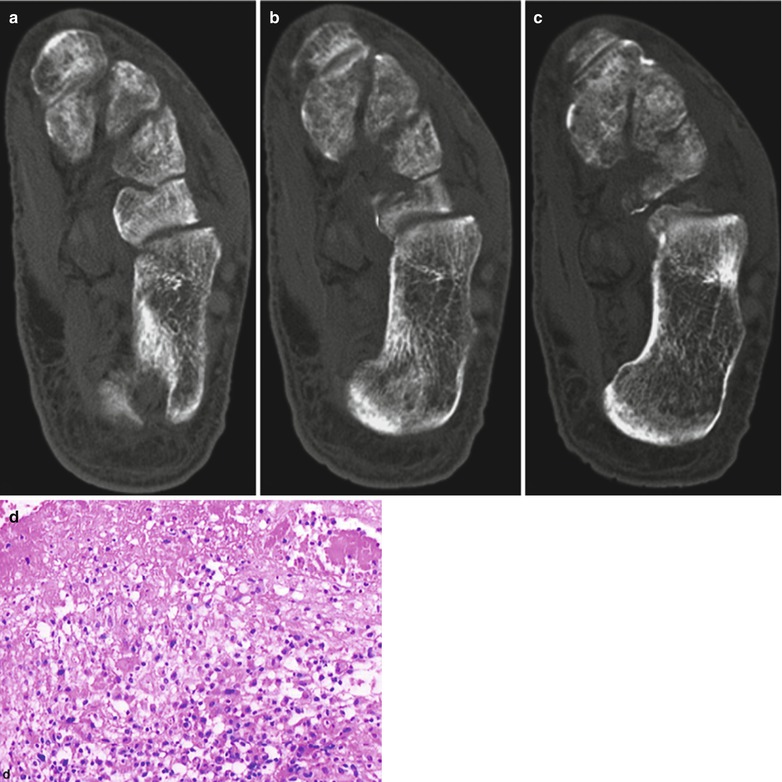
Fig. 23.4
(a–d) HIV/AIDS related extrapulmonarycalcaneal tuberculous osteomyelitis. (a–c) It is demonstrated to have round liked bone defects in the posterior calcaneus with clear boundary and sparse calcaneal trabecula. (d) Microscopy at a medium magnification demonstrates epitheloid cells and caseous necrosis
23.2.6 Diagnostic Basis
1.
The patients mostly have a source lesion of TB or a past history of TB.
2.
The patients have a long term fever, night sweating, accelerated ESR and other symptoms of TB.
3.
Conventional X-ray demonstrates destructed bone, blurry facet and soft tissue swelling.
4.
CT scanning demonstrates more favorably fine bone destruction, facet involvement, peritoneal reaction and surrounding soft tissues of the joints.
5.
MR imaging demonstrates intramedullary edema in long T2 signal, which is more sensitive to the pathological changes of the soft tissues.
23.2.7 Differential Diagnosis
The disease should be mainly differentiated from malignant bone tumor and aseptic bone necrosis. The following findings including swelling degrees of the soft tissue, abscess liked cysts, soft tissue masses, residual bone shell at the margin of soft tissue masses or shell liked calcification, neoplasm in the soft tissue mass or tumor chondral calcification have significance for the differential diagnosis. In the cases with osteomyelitis, the range of soft tissue swelling is more extensive than those in bone malignancy. Increased surrounding bone density of destructed bone areas is an important feature of acute osteomyelitis. Gas and adipose liquid signs as well as formation of sinus canal are rare but reliable signs of osteomyelitis.
23.3 HIV/AIDS Related Suppurative Myositis
23.3.1 Pathogen and Pathogenesis
This disease is actually abscess formed in deep layer of large striated muscle. Intramuscular abscess is rare. Its pathogenesis is believed to be blood borne spreading caused by bacteremia. Otherwise, it is caused by spreading of adjacent bone or soft tissue infection and further spreading along with blood flow.
23.3.2 Pathophysiological Basis
Purulent myositis occurs commonly in immunocompromised patients, especially AIDS patients. The lesions are most commonly found in quadriceps femoris, gluteus, arm and shoulder muscles. According to statistics, about 40 % of the cases have multiple abscesses.
23.3.3 Clinical Symptoms and Signs
The early symptoms include spasm pain, and then upsets caused by progressively serious edema and low grade fever, muscle rigidity, tissue edema and aggravating tenderness. In early period of muscle rigidity, puncture and aspiration may have negative findings, and then yellowish thick purulent fluid can be obtained. By bacterial culture, staphylococcus aureus can always be found, occasionally Pyogenic streptococcus or Escherichia coli.
23.3.4 Examinations and Their Selection
MR imaging has a higher resolution in demonstrating soft issue lesions than CT scanning. MR imaging provides more direct images from multiple perspectives, which is sensitive to the early lesions in the muscles and bones. Therefore, MR imaging is the examination of choice and the optimal examination for suppurative myositis.
For the cases with further progressive lesions, CT scanning can provide supplementary information on bone destruction.
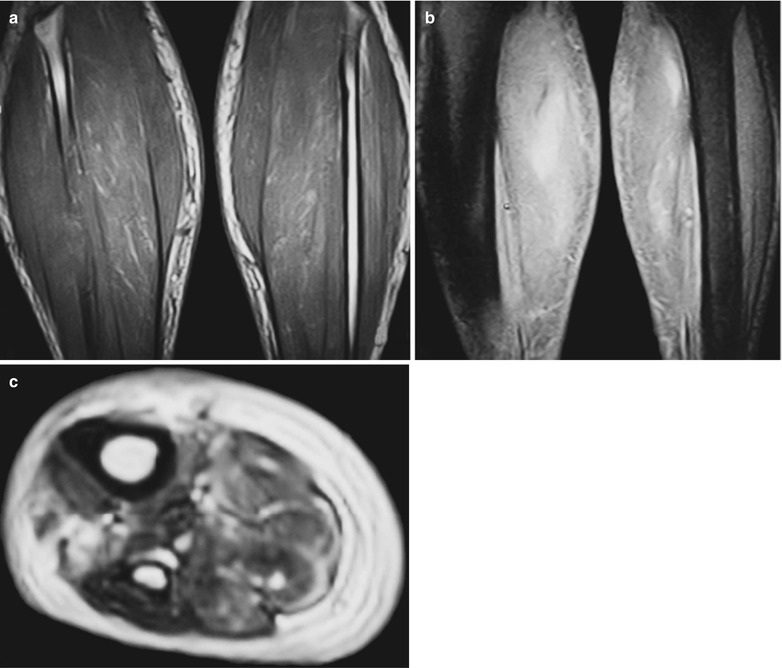
23.3.5 Imaging Demonstrations
23.3.5.1 CT Scanning
CT scanning demonstrates swollen muscles with decreased CT values due to edema, clearly defined intramuscular abscesses. Enhanced scanning demonstrates intramuscular necrosis and no enhancement of the necrotic areas, ring shaped enhancement of muscular abscesses with clear boundary.
23.3.5.2 MR Imaging
MR imaging is more sensitive than CT scanning in demonstrating muscular inflammations. T1WI demonstrates low signal in the muscles. T2WI demonstrate high signal from the intramuscular pus fluid. Enhanced imaging demonstrates low signal and high signal ring shaped enhancement surrounding the necrotic tissue.
Case Study
A female patient aged 34 years was confirmatively diagnosed as having AIDS by the CDC. Her CD4 T cell count was 40/μl.