(1)
Radiology Department Beijing You’an Hospital, Capital Medical University, Beijing, People’s Republic of China
21.3.1 Pathogens and Pathogenesis
21.3.2 Pathophysiological Basis
21.3.3 Clinical Symptoms and Signs
21.3.5 Imaging Demonstrations
21.3.6 Diagnostic Basis
21.3.7 Differential Diagnosis
21.4.1 Pathogens and Pathogenesis
21.4.2 Pathophysiological Basis
21.4.3 Clinical Symptom and Signs
21.4.5 Imaging Demonstrations
21.4.6 Diagnostic Basis
21.4.7 Differential Diagnosis
Abstract
Abdomen is one of the most commonly involved body parts by AIDS, following the chest. It may involve the whole digestive tract and the liver, biliary tract, pancreas and some urinary and reproductive organs. It may also involve the tissues of mesentery, peritoneum and retroperitoneum. Currently, with the continuously increasing prevalence of AIDS, the manifestations and diagnosis of HIV/AIDS related abdominal diseases have gained increasing attention. In fact, many patients are definitively diagnosed as AIDS because they pay clinic visits due to gastrointestinal symptoms. Most of the abdominal symptoms in AIDS patients are non-specific, including abdominal pain, abdominal distension, diarrhea, fever, weight loss, abdominal mass, jaundice and gastrointestinal bleeding. These non-specific clinical manifestations, in addition to delayed specific laboratory tests, the diagnosis and treatment are usually delayed. HIV/AIDS related abdominal organs diseases will be described in detail in the relevant chapters and sections. In this chapter, we focus our attention on peritoneal and retroperitoneal diseases.
21.1 General Introduction to HIV/AIDS Related Peritoneal and Retroperitoneal Diseases
Abdomen is one of the most commonly involved body parts by AIDS, following the chest. It may involve the whole digestive tract and the liver, biliary tract, pancreas and some urinary and reproductive organs. It may also involve the tissues of mesentery, peritoneum and retroperitoneum. Currently, with the continuously increasing prevalence of AIDS, the manifestations and diagnosis of HIV/AIDS related abdominal diseases have gained increasing attention. In fact, many patients are definitively diagnosed as AIDS because they pay clinic visits due to gastrointestinal symptoms. Most of the abdominal symptoms in AIDS patients are non-specific, including abdominal pain, abdominal distension, diarrhea, fever, weight loss, abdominal mass, jaundice and gastrointestinal bleeding. These non-specific clinical manifestations, in addition to delayed specific laboratory tests, the diagnosis and treatment are usually delayed. HIV/AIDS related abdominal organs diseases will be described in detail in the relevant chapters and sections. In this chapter, we focus our attention on peritoneal and retroperitoneal diseases.
After HIV infection, it firstly involves the lymph nodes all over the body. Stimulated by the virus antigen, the immunocytes in the lymph nodes are activated to proliferate and differentiate to cause cellular and humoral immune responses in the lymph nodes. Clinically, it is manifested as lymphadenectasis, which is caused directly by HIV infection. Most diseases in AIDS patients are the complications after HIV infection progresses into the stage of AIDS. In the stage of AIDS, helper T lymphocytes significantly decrease due to long-term damage by HIV and its immune functions are also destroyed in different degrees. The patients are susceptible to opportunistic infections and malignancies, especially concurrence of multiple opportunistic infections when CD4 T cell count is extremely low. Occurrence of peritoneal and retroperitoneal diseases in AIDS patients are mostly peritoneal and retroperitoneal responses to the abdominal organs lesions. That is to say, abdominal organs lesions commonly involve the peritoneum and retroperitoneum. Therefore, clinically, the imaging demonstrations and immunity of the patients should be in combination to be considered. In the imaging analysis, the abdominal organs lesions should be in combination with peritoneal and retroperitoneal lesions for a comprehensive understanding of their relationship for the diagnosis.
Opportunistic infections are the principal complications of HIV/AIDS, whose incidence is related to the virulence of the pathogenic bacteria or virus and the immunity of the patient. The chances of opportunistic infections significantly increase when CD4 T cell count is lower than 350–400 × 106/L. The common abdominal opportunistic infections in AIDS patients include tuberculosis, CMV infection, herpes virus infection, fungal infection, pneumocystis carinii infection and histoplasmosis. These infections not only involve abdominal organs, biliary system and intestinal mucosa, but also are disseminating to invade and involve the peritoneal cavity and retroperitoneal structures. HIV/AIDS complicated by mycobacterium non-tuberculosis infection are frequently reported and it occurs when the immunity is severely compromised.
Kaposi’s sarcoma and lymphoma are more common in HIV/AIDS related malignancies. KS and malignant lymphoma of abdominal organs are discussed in the corresponding chapters and sections. In this chapter, HIV/AIDS related peritoneal and retroperitoneal lymphoma is the focus. Lymphoma is the second common in HIV/AIDS related malignancies, following KS. The risk of non-Hodgkin’s lymphoma in AIDS patients is greatly higher than the general population and its pathogenesis is still unknown, which may be related to B lymphocytes proliferation caused by HIV or Epstein-Bar virus.
Due to compromised immunity of the AIDS patients, the incidence of various opportunistic infections and other related tumors obviously increases. Abdominal lesions in AIDS patients need various examinations, especially CT scanning, to define their diagnosis and differential diagnosis as well as to assess the therapeutic efficacy. Barium meal radiology is the most convenient method to detect the lesions of the gastrointestinal tract, which can demonstrate the lesions in the gastrointestinal lumen. Although endoscopy can visually display the lesions as well as collect tissues for biopsy, its manipulation is complex that can lead to obscure bleeding of the gastrointestinal mucosa to endanger the patients. CT scanning is advantageous in demonstrating the extragastrointestinal lesions, peritoneal lesions, abdominal lymph nodes lesions and abdominal organs lesions. Especially the enhancement of lesions range and lymph nodes can help to make a preliminary diagnosis before the results of bacteriological or histological examinations. However, MR imaging is rarely applied because CT scanning can well define the lesions and the further MR imaging is thus unnecessary. The cost of MR imaging is also a reason. And the other reason is that AIDS patients are in a generally poor physical constitution and they show poor compliances in breath holding examinations for MR imaging. The importance of the diagnostic imaging is that they can assess the dynamic changes of the lesions and the therapeutic efficacy. The diagnostic imaging of peritoneum and retroperitoneum is a part of abdominal scanning/imaging. For patients with AIDS complicated by abdominal diseases, non-invasive diagnostic examination should be of choice to reduce their pain’ and to reduce the risk of infection in medical staffs.
21.2 HIV/AIDS Related Peritoneal and Retroperitoneal Lymphadenectasis
21.2.1 HIV/AIDS Related Lymphadenectasis
21.2.1.1 Pathogens and Pathogenesis
Lymph node is a peripheral immune organ. The pathogenic microorganisms and toxins from tissues can gain their access into the lymph fluid via lymphatic capillaries. The immunocytes in the lymph nodes receive antigen stimulation to be activated for proliferation and differentiation. The following cellular and humoral immune responses occur in the lymph nodes to cause the clinical manifestation of lymphadenectasis.
Lymphadenectasis in non-AIDS patients can be divided into two types according to their distribution: (1) local lymphadenectasis, which is commonly seen in the cases of lymph nodes inflammation, lymph nodes tuberculosis and lymph node metastasis of malignancies; (2) general lymphadenectasis, which is common in the cases of infectious mononucleosis, lymphoma, various types of leukemia, and systemic lupus erythematosus. Clinically, according to the distribution of the enlarged lymph nodes, its differential diagnosis can be restricted into less possibility. Abdominal organs lesions, including infections and malignancies, can invade the lymph nodes via the lymphatic system. Therefore, occurrence of peritoneal and retroperitoneal lymphadenectasis cannot exclude the possibility of abdominal organs diseases, especially malignancies.
Pathologic changes of AIDS are predominantly found in lymphatic tissues and hematopoietic system. The lymph node is the key target organ. There are three common causes of HIV/AIDS related lymphadenectasis. By frequency, they are lymph nodes lesions caused by HIV itself, opportunistic infections and malignancies. In this section, we focus on the most common one, lymphadenectasis caused by HIV itself.
After HIV gains its access into the human body, Langerhans cells or dendritic cells pass it to CD4 T cells, whose homing causes in acute infection of the lymphatic tissue, with clinical manifestations of general lymphadenectasis, fever, rash and (or) symptoms of the central nervous system. After a varying durations of incubation period (clinically asymptomatic period), the virus replicates itself in a large quantity to successively involve the general lymphatic tissues. Meanwhile, specific immunity occurs and the viruses are confined in follicular dendritic cells of the lymphatic germinal centre. This is known as the chronic infection stage with clinical manifestations of AIDS associated syndrome and chronic lymphadenopathy. During the acute and chronic periods of lymphatic tissues infection, general lymphadenectasis may occur, with abdominal lymphadenectasis as its local manifestation.
In addition to HIV induced general lymphadenectasis, the indirect effects of HIV to induce destruction of CD4 T cells and cellular immunodeficiency are predominant. The results are occurrence of opportunistic infections and neoplasms.
In HIV infected patients, with the further damage to the immunity by the viruses, the CD4 T cell count is gradually decreasing to cause increasingly serious compromised immunity. When CD4 T cell count is below 200/μl in the stage of AIDS, opportunistic infections occurs successively. With the decrease of the CD4 T cell count, the incidence of opportunistic infections is increasing, with complications of various opportunistic infections as well as complex and diverse conditions. The gastrointestinal tract, communicating with the outside world, is a location that is most vulnerable to opportunistic infections. The causes of abdominal infectious lymphadenectasis are mainly tuberculosis infection, followed by intestinal infection. Fungal infections are relatively rare. Once the HIV infection progresses into the stage of AIDS, HIV exerts great destructive effects on the macrophages and CD4 T lymphocytes to cause a decrease or even loss of its suppression against mycobacterium tuberculosis, which further leads to recurrence and dissemination of the tuberculosis foci. Meanwhile, the obviously compromised immunity increases the possibility of reinfection by exogenous tuberculosis bacilli. All of these processes can result in tuberculous lymphadenectasis.
In AIDS patients, the lymphocyte count is decreasing, with deficiency of T cells and reverse ratio of TH/TS. There is also reduced activity of the natural killer cells. All these factors cause the decreases of immune surveillance and defensive function, which in turn impedes the body from effectively eliminating mutant cells to cause malignancies. In HIV/AIDS related tumors, the most common is Kaposi’s sarcoma, followed by lymphoma that is commonly non-Hodgkin’s B cell lymphoma. So far, it has been understood that the decrease of CD4 T cell count is the only reason for significantly increased risk of KS. It has been reported that impaired immunity, chronic antigen stimulation and overproduction of cytokines all contribute to the occurrence of lymphoma. EB virus may be the main reason for occurrence of lymphoma and non-Hodgkin’s lymphoma. Apart from the knowledge about KS and typical Non-Hodgkin’s lymphoma, the pathogenesis of other tumors caused by compromised immunity remains elusive. But it has been known that their pathogenesis is related to the decrease of CD4 T cell count. HIV/AIDS related neoplasms cause general lymphadenectasis, with involvement of abdominal, retroperitoneal and mesenteric lymph nodes.
21.2.1.2 Pathophysiological Basis
During the early and chronic persistent periods, the pathological changes of lymph nodes are mainly reactive hyperplasia (follicular hyperplasia, I period). In this period, follicular hyperplasia is obvious, with irregular shapes like a map. The mantle zone is thinner or absent, with expansion of the germinal centre. Due to the destruction of dendritic cells in the follicular centre, lytic follicle occurs, which is not unique in AIDS. With the development of the lesions, follicles degenerate and the follicular central cells gradually reduce, with proliferation of interstitial cells, to form a characteristic concentric circle like an onion (follicular regression, II period). When it progresses into the period of follicles absence (III period), there is a disorderly lymphatic structure, with obviously decreased amount of follicles, proliferation of histocytes with scattered lymphocytes, plasmacytes and immunoblastic cells, and commonly post-capillary vein hyperplasia. In the period of lymph nodes exhaustion (IV period), total destruction of the lymph nodes structure occurs, with obviously decreased lymphocytes, diffuse or nodular proliferation of histocytes with or without accompanying fibrosis. Follicular regression and absence indicate the decline of the immune function. Therefore, opportunistic infections and/or neoplasms complicate HIV/AIDS in these two periods.
Lymphadenectasis caused by various HIV/AIDS related opportunistic infections and neoplasms will be discussed in the following sections.
21.2.1.3 Clinical Symptoms and Signs
As the fact that AIDS is a new type of infectious disease, with the immune system as the target organ of HIV, various diseases may occur when the immunity is compromised. Therefore, the clinical manifestations are diverse and complex. The clinical manifestations can be categorized into following five groups: (1) general manifestations including long-term fever, night sweat, weight loss of more than 10 %, abdominal pain, diarrhea and bloody stool; (2) persistent general lymphadenectasis, especially retroperitoneal and mesenteric lymphadenectasis with non-specific symptoms and signs; (3) multiple infections, especially opportunistic infections; (4) various neoplasms, especially KS and lymphoma; (5) multiple lesions of the nervous system. Therefore, AIDS patients commonly pay their clinic visits due to various common diseases, including all clinic sections. The physicians should comprehensively access the clinical symptoms and signs to consider the possibility of AIDS in the differential diagnosis.
21.2.1.4 Examinations and Their Selection
There are various causes for the abdominal lymphadenectasis in AIDS patients, with varying manifestations. The selection of appropriate diagnostic imaging facilitates the detection, comprehensive assessment, diagnosis and differential diagnosis. Ultrasound is widely applied for abdominal diseases. For the diagnosis of AIDS, a syndrome that can involve multiple organs with various manifestations, ultrasound is economical, practical and convenient, which is suitable for screening. Its application for reexamination is also convenient, which is applicable for following up observations of the therapeutic efficacy. However, due to the interference of gastrointestinal gas and coverage by the spinal column, ultrasound is less sensitive to early lesions of retroperitoneal lymphadenectasis and can favorably demonstrate the large or fused mass of lymphadenectasis. In addition, it can favorably show the indirect changes of the retroperitoneal blood vessels. Compared to ultrasound, CT scanning and MR imaging play increasingly more important roles in the diagnosis of HIV/AIDS related abdominal diseases. Both can comprehensively evaluate the abdominal lesions in AIDS patients, and even can provide information for accurate diagnosis. Although the imaging findings are not always specific, they play important role in formulating therapeutic plan and assessing therapeutic efficacy, such as accurate staging of the opportunistic infections. The nuclear medical examination, such as PET scanning, is rarely applied for the assessment of AIDS.
21.2.1.5 Imaging Demonstrations
CT Scanning
Abdominal lymphadenectasis is one of the manifestations of general extensive lymphadenectasis in AIDS patients. Superficial lymphadenectasis mainly distributes in the bilateral inguinal region, with manifestations of multiple nodules in a diameter of above 3 cm that may scatter or accumulate into a large mass. Deep lymphadenectasis such as retroperitoneal, mesenteric and pelvic lymphadenectasis is mostly multiple nodular in different sizes surrounding the major blood vessels with clear boundaries and rare fusion. The nodular density is even, with slight to moderate enhancement by enhanced scanning and no obvious necrotic area. Enlarged lymph nodes surrounding the abdominal aorta may cause anterior migration of the abdominal aorta and its enlarged distance from the spinal column and the inferior vena cava. The enlarged lymph nodes surrounding the abdominal trunk can straighten its running course. Enlarged lymph nodes surrounding the superior mesenteric artery and enlarged lymph nodes surrounding the renal vessels can also lead to similar migration.
MR Imaging
The distribution of retroperitoneal lymphadenectasis is the same as CT scanning demonstrations. Its MR imaging shows similar signals to general lymph nodes, with even and low T1WI signal against high signaling adipose background and slightly high and even T2WI signal in moderate and high signaling adipose tissues. By adipose suppression imaging, the enlarged lymph nodes are more clearly defined, in moderately high and even signal. The lymph nodes can accumulate into groups, but rarely fuse, with clear boundaries from each other. The surrounding blood vessels of the lymph nodes are in void low signals and are compressed by multiple enlarged lymph nodes to migrate, with rigid running course. But the vascular wall is smooth and intact with no invasion.
Ultrasound
Abdominal lymphadenectasis is obvious in HIV infected patients, with commonly accumulation of multiple enlarged lymph nodes and their fusion. The ultrasonogram demonstrates characteristic changes, including (1) Enlarged wide diameter of the lymph nodes, longitudinal to transverse ratio below 2, full morphology and huge mass formed by fusion of multiple enlarged lymph nodes. (2) Unclearly defined interface of the cortex and medulla in the enlarged lymph nodes, with low echo, enhanced echo of the envelope with unclear boundary that has peripheral infiltration in crab liked appearance. (3) Lymphadenectasis can be singular or multiple, principally multiple, with greater significance. (4) Changes of the adjacent blood vessels including straight running course of the abdominal trunk due to its surrounding lymphadenectasis, the left and right wings sign when enlarged lymph nodes encompassing the hepatic artery and splenic artery (hawk wing sign), forward migration of the abdominal aorta and its enlarged distance from the inferior vena cava due to its surrounding lymphadenectasis.
Case Study
A male patient aged 35 years was confirmatively diagnosed as having AIDS by the CDC. His CD4 T cell count was 85/ μl.
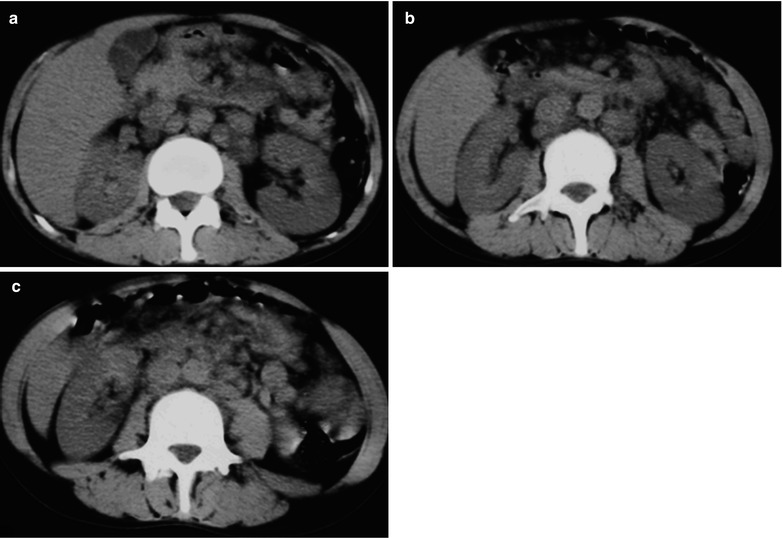
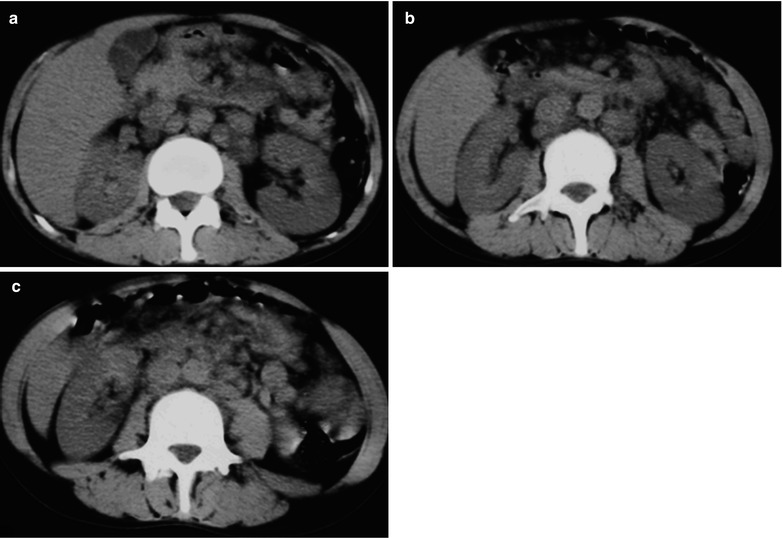
Fig. 21.1
(a–c) HIV/AIDS related retroperitoneal lymphadenectasis. (a–c) Epigastric plain CT scanning demonstrates multiple lymphadenectasis surrounding the abdominal artery, supramesenteric artery and bilateral hepatic portal areas that accumulate into mass but with no fusion
21.2.1.6 Diagnostic Basis
As for HIV infected patients, general or local lymphadenectasis can be detected by physical examinations and diagnostic imaging. Their density and signal are even, with rare fusion. The causes of lymphadenectasis are multiple. According to the imaging demonstrations, the causes can be preliminarily distinguished. But the definitive diagnosis of HIV/AIDS related lymphadenectasis cannot be made. Most conclusions are the diagnosis of consistency.
21.2.1.7 Differential Diagnosis
HIV/AIDS Related Lymphoma
HIV/AIDS related abdominal lymphadenectasis should be differentiated from HIV/AIDS related lymphoma, which has its lesions confined within the retroperitoneum. HIV/AIDS related lymphoma can only involved the retroperitoneal lymph nodes. The distribution of the involved lymph nodes is in a similar range like HIV/AIDS related abdominal lymphadenectasis, with even density and rare necrosis as well as even enhancement by enhanced CT scanning. However, the cases of HIV/AIDS related lymphoma have accumulated multiple enlarged lymph nodes with fusion into a mass to embed the mesenteric blood vessels, abdominal aorta and inferior vena cava in vascular embedding sign. More importantly, HIV/AIDS related lymphoma commonly has manifestations of intestinal lymphoma.
HIV/AIDS Related Lymphoid Tuberculosis
It manifests as multiple enlarged lymph nodes in the retroperitoneum, with uneven density and lower interior density. Enhanced scanning demonstrates smooth ring shaped enhancement, with no central enhancement. HIV/AIDS related lymphadenectasis has even density foci, with rare interior necrosis. In addition, retroperitoneal lymphoid tuberculosis is commonly complicated by or secondary to intestinal tuberculosis, with corresponding clinical manifestations of intestinal tuberculosis, which facilitates the differential diagnosis.
Non-HIV/AIDS Related Lymphadenectasis
Before the clinical confirmative diagnosis of HIV infection, their differential diagnosis is difficult. HIV/AIDS related lymphadenectasis has evident features: (1) a wider range of involvement, rare local foci, common involvement of the abdomen, diffuse enlargement, large flaky fusion, sandwich sign in the mesentery and the major omentum in large pie liked appearance; (2) multiple organs involvement with commonly involved abdominal lymph nodes, liver and spleen, peritoneum and gastrointestinal tract. Compared to the cases of non-HIV/AIDS related lymphadenectasis, the involvement of the liver and spleen in the cases of HIV/AIDS related lymphadenectasis are more common, with diffuse nodular foci, which can be the basis for the gross differentiation of the two diseases.
Non-HIV/AIDS related lymphadenectasis occurs in many diseases, with distinctive features.
Typhoid Fever
In the cases of typhoid fever, there is peritoneal lymphadenectasis, with accompanying symptoms of high fever, ascites, hepatosplenomegaly, decreased peripheral WBC count and platelets, which are similar to malignant histiocytosis. After treatment, the heteromorphic lymphocytes are absent, with negative findings by blood culture and normal retroperitoneal lymph nodes.
Histiocytic Necrotic Lymphadenitis (HNL)
It is rarely seen in clinical practice and therefore can be misdiagnosed. It occurs commonly in middle aged and young adults, with 80 % patients being under the age of 30 years. The pathological examinations demonstrate characteristic necrosis of the lymph nodes, which is also known as extensive and coagulative necrosis of lymph nodes, with no infiltration of neutrophils. In the cortex area, there are extensive cellular necrosis, large quantity residue fragments which is known as necrotic fragments. The clinical symptoms include persistent high fever. Routine B mode ultrasound demonstrates retroperitoneal lymphadenectasis of different sizes, which can be pathologically confirmed. The cause of the disease may be related to virus infection or to virus induced autoimmune responses. It is believed to be lymph nodes with allergic reaction or slight collagen disease. Antibiotic therapy is ineffective.
Retroperitoneal Chronic Non-specific Lymphadenitis
The cause of the disease is complex, with more occurrences in young and middle-aged adults. Its pathogenesis is the chronic infection of the corresponding drainage tissues and organs and absorption of tissues destructive products, which can involve the lymph nodes of the drainage area to cause chronic inflammation. Chronic lymphadenitis has complex manifestations, including various responsive hyperplasias in the lymph nodes such as chronic diffuse lymphocytes proliferation, follicular hyperplasia, sinus histocytes proliferation. Its diagnosis needs to exclude specific lymphadenitis or lymphadenopathy such as lymphoid tuberculosis and systemic lupus erythematosus. Its diagnosis is difficult. Findings by once puncture and biopsy cannot define its diagnosis.
21.2.2 HIV/AIDS Related Mycobacterium Infectious Lymphadenectasis
21.2.2.1 Pathogens and Pathogenesis
Mycobacterium infection is one of the common abdominal opportunistic infections in AIDS patients and the most common pathogen is mycobacterium tuberculosis bacilli. Generally decreased immunity is the pathogenic basis of TB. Factors including fatigue, coldness and dampness, malnutrition, vitamin deficiency, poor living environment and some virus infection contribute to decreased immunity. Tuberculosis induced by HIV infection has distinctive pathological changes and imaging demonstrations.
HIV infection targets to destroy CD4 T cells, leading to a progressive decrease of CD4 T cell count in the blood circulation. The impaired function of CD4 T cells destroys the defense mechanism of the human body to limit the responses from cells to the antigen of mycobacterium tuberculosis bacilli. Therefore, the stable incubated old TB foci are reactivated to cause secondary TB, namely endogenous reactivation. In addition, HIV infected patients are susceptible to exogenous reinfection due to the weak defense mechanism. The reinfected mycobacterium tuberculosis bacilli can rapidly cause the disease, with rapidly exacerbating conditions. The resistance of the mycobacterium bacilli to drugs can lead to outbreak and prevalence of TB.
Abdominal TB infection is often a result of blood-borne transmission, with complications of blood borne transmitted pulmonary TB and general lymph nodes TB. It has been reported that when the CD4 T cell count is below 350–400/μl, the infection rate of TB is obviously increasing, with concurrent increased infection rate of extrapulmonary TB, being up to 50 %. In patients with non-HIV/AIDS related TB, the incidence of extrapulmonary TB is only 10–15 %. Abdominal lymph nodes involvement is the most common manifestation of abdominal TB, found in 2/3 patients, commonly with multiple lymph nodes involvement. Abdominal TB in AIDS patients is more prone to disseminate, with involvement of mesenteric lymph nodes, peritoneum and abdominal organs including the liver, spleen, pancreas and gastrointestinal tract, especially ileum and colon.
In the patients with immune-deficiency, atypical mycobacteria infections rarely occur, but commonly occur in AIDS patients. The pathogen is commonly avium intracellular mycobacterium. Eight cases of AIDS complicated by Geneva mycobacteria infection have been reported and it is believed that its occurrence is at CD4 T cell count being lower than 100/μl. Puncture for biopsy can define the diagnosis.
21.2.2.2 Pathophysiological Basis
Early HIV infection can be complicated by TB, or TB may occur prior to HIV infection. The manifestation of TB is similar to those in immunocompetent patients. Microscopically, typical tuberculosis granuloma can be found, with slight caseous necrosis, less mycobacterium tuberculosis (MTB), more CD4 T cells, epithelioid giant cells and Langerhans cells around the foci to confine the foci. Because the destructive effects of HIV on the immune functions of CD4 T lymphocytes and macrophages, with the decrease of the CD4 T cells, the macrophages have decreased ability to inhibit the growth of mycobacterium tuberculosis to result in expanded caseous necrosis, decreased epithelioid giant cell and Langerhans cell and inhibited formation of tuberculous granuloma. In the advanced stage of HIV infection with complicated tuberculosis, the CD4 T cell count further decreases, with more serious immunodeficiency and even loss of immune responses. In the foci, there are insufficient epithelioid giant cells and Langerhans cells, extremely rare giant cells and lymphocytes, no granuloma formation but purulent coagulative necrosis and large quantity proliferation of mycobacterium tuberculosis bacilli. By biopsy or autopsy, it is found that TB is blood borne disseminating and non-responsive.
21.2.2.3 Clinic Symptoms and Signs
AIDS complicated by abdominal tuberculosis is manifested as active tuberculosis and systemic blood borne spreading. Clinically, patients show general symptoms of TB including fever, cough, expectoration and hemoptysis, night sweats, general soreness and pain, fatigue, anemia, emaciation, malnutrition and other toxic consumptive symptoms. Based on the involved organs by abdominal TB, there are corresponding symptoms and signs, commonly with abdominal pain, abdominal distention, diarrhea, abdominal tenderness and rebound pain in some patients, ascites sign positive and other gastrointestinal symptoms, lymphadenectasis and hepatosplenomegaly.
21.2.2.4 Examinations and Their Selection
AIDS complicated by abdominal mycobacterial bacilli infection can involve the gastrointestinal tract and parenchymal organs. Therefore, different diagnostic imaging examinations are necessary to comprehensively assess the abdominal lesions. Ultrasound examination is economical, practical and convenient, with wide application for assessment of abdominal parenchymal organs, following up examinations and assessment of curative effect. Ultrasound guided biopsy of parenchymal organs can shorten the time for definitive diagnosis. Barium meal radiology is simple and noninvasive that result in favorable compliance from the patients to assess the gastrointestinal involvement. Meanwhile, the comparatively not close contacts between the patients and medical staffs facilitate the occupational protection of the medical staffs. CT scanning and MR imaging are advantageous in assessing the abdominal parenchymal organs as well as abdominal and retroperitoneal lymph nodes. When the intestinal tract is well prepared, the gastrointestinal tract can be well assessed. Therefore, CT scanning and MR imaging, especially CT scanning, play important roles in assessing AIDS complicated by abdominal diseases. The above mentioned diagnostic imaging examinations can simultaneously assess retroperitoneal lymph nodes TB.
Nuclear medical examinations, including PET, have advantages of high sensitivity, but less significance for AIDS complicated by abdominal tuberculosis.
21.2.2.5 Imaging Demonstrations
HIV/AIDS related abdominal TB is commonly multiple organs infection with mesenteric, peritoneal and retroperitoneal lymph nodes TB. Abdominal organs TB are discussed in the corresponding chapter and sections.
CT Scanning Demonstrations
Abdominal lymph node TB is manifested as multiple soft tissue density nodules in the mesenteric, hepatic portal, hepatoduodenal ligament and surrounding abdominal aorta areas. The nodules are accumulated into mass with comparatively clear boundary. In the serious cases, there is sandwich liked changes in the mesentery, namely anterior and dorsal mesenteric lymphadenectasis with central mesenteric vascular vessels. Retroperitoneal enlarged lymph nodes are distributed around the major blood vessels, commonly leading to enlarged distance between the aorta and the spinal column as well as the inferior vena cava. Enhanced scanning demonstrates central necrosis of the nodules with no enhancement, marginal smooth ring shaped enhancement, and even the ring shaped enhancement of the small lymph nodes.
Abdominal organs tuberculosis can cause peritoneal tuberculosis, with manifestations of extensively thickened peritoneum and obviously thickened omentum in pie liked appearance and multiple nodules in the peritoneum to form abdominal effusion. Enhanced scanning demonstrates obvious enhancement of the nodules in the thickened omentum and peritoneum.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree