(1)
Radiology Department Beijing You’an Hospital, Capital Medical University, Beijing, People’s Republic of China
25.1.3 Zoster
25.1.4 Molluscum Contagiosum
25.1.5 Oral Candidiasis
25.1.6 Seborrheic Dermatitis
25.1.7 Genital Candidiasis
25.1.8 Scabies
25.1.9 Kaposi’s Sarcoma
25.5.1 Pathogen and Pathogenesis
25.5.2 Pathophysiological Basis
25.5.3 Clinical Symptoms and Signs
Abstract
In AIDS patients, skin diseases are common including infectious and exogenous infectious skin diseases. The infectious skin diseases are commonly fungal and viral infection of the skin, and bacterial infection of the skin rarely occurs.
25.1 An Overview of HIV/AIDS Related Skin Diseases
In AIDS patients, skin diseases are common including infectious and exogenous infectious skin diseases. The infectious skin diseases are commonly fungal and viral infection of the skin, and bacterial infection of the skin rarely occurs.
The common skin diseases include seborrheic dermatitis, psoriasis, skin and nail fungal infection, herpes virus infection, insect skin infection and bacterial infection.
25.1.1 Bacillary Angioma or Bacillary Peliosis
Bacillary epithelioid angiomatosis (BA) is also known as bacillary angiomatosis (BP) or epithelioid angiomatosis. It was first reported by Stoler in 1983 to be a multiple cutaneous vascular proliferative disease in AIDS patients that is different from Kaposi sarcoma [15]. The findings of small bacilli in the skin lesions were also reported. The disease was then believed to be a newly found infectious disease in AIDS patients which causes cutaneous and organ minor vascular proliferation. Bacillary angioma can cause vascular proliferation in multiple organs, including lymph nodes, skin, gastrointestinal tract and lungs. The manifestations of skin lesions are various, including reddish vascular lesions that are smooth and tend to rupture; spot lesions of cellulitis, KS liked lesions, dry squamous lesions with lupus base and subcutaneous nodules. Bacillary vascular diseases may be chronic and last for 1 year. There is commonly collar desquamation around the lesions, which is the key point for the differential diagnosis from Kaposi’s sarcoma. In addition, it also should be differentiated from vascular sarcoma, pyogenic granuloma and other pathogenic sepsis.
25.1.2 Herpes Simplex Virus Caused Primary or Recurrent Oral and Genital Diseases
The lesions are commonly found in the oral cavity, perioral area, vulva, mucosa and perianal skin; occasionally in the groin and buttocks, being small blisters or erosions, and even shallow ulceration.
25.1.3 Zoster
Varicella-zoster virus causes skin and mucosa infections that are distributed along the skin area. In HIV positive patients, the manifestations are pain, necrosis and hemorrhage. The patients have painful skin blisters, which is different from HIV negative patients with zoster. Zoster in HIV negative population recurs.
25.1.4 Molluscum Contagiosum
It is a benign skin infection caused by pox virus, which transmits via direct contacts. It usually occurs in the head and neck as well as pudendum. They are semicircular papules in the colors of flesh, white and yellow. It should be differentiated from disseminated cryptococcosis infection or other fungal infections with similar clinical manifestations.
25.1.5 Oral Candidiasis
It is a fungal disease in the oral mucosa or tongue which is caused by Candida, which commonly indicates the occurrence of HIV infection. Thrush is the most common manifestation. Other manifestations include erythema, hyperplasia or plaques. HIV patients usually have three symptoms: pseudomembrane, erythema and angular cheilitis.
25.1.6 Seborrheic Dermatitis
About 25–83 % of HIV positive patients have seborrheic dermatitis which has always a local occurrence near the midline of the body. Sometimes, it occurs in ears, chest, upper back, axilla and groin.
25.1.7 Genital Candidiasis
Genital yeast infection is caused by a variety of pathogens belonging to the Candida species. It is common in females and is more common and serious in HIV positive females. Refractory vaginal Candida infection may be the primary clinical manifestation in HIV positive women, which can also have manifestations of genital inflammation, white thick secretion on the vaginal folds and ulcers on the viginal wall.
25.1.8 Scabies
It is one of the reasons of pruritus in HIV positive patients. And it is common underdeveloped areas.
Studies have demonstrated that the incidence of neoplasms closely related to virus infections. Therefore, the neoplasms are known as opportunistic neoplasms.
25.1.9 Kaposi’s Sarcoma
It is a neoplasm originated from blood vessels in the skin, mucosal surface or organs, which is the most common neoplasm in HIV positive patients. Currently, it is believed to be induced by HHV-8. Epidemic or HIV/AIDS related KS is a neoplasm with short duration that can be disseminated. It prevalence is commonly regional in homosexual HIV positive patients. The condition progresses slowly or rapidly, with poor prognosis. Epidemic KS commonly spreads to the skin, lymphatic system, lungs, gastrointestinal tract, liver or heart. The clinical manifestations are characterized by asymptomatic skin defects with pigment sedimentation or skin defects in the head, neck and the oral cavity. Extensive oral involvement has manifestations of fallen tooth, pain and ulcer. In the advanced stage, edema and pain occur in the lower limbs ends, penis, scrotum or face. CD4 T cell count may increase by about 200–500/μl.
25.2 HIV/AIDS Related Fungal Infections
25.2.1 HIV/AIDS Related Mucocutaneous Candidiasis
25.2.1.1 Pathogen and Pathogenesis
Candida is a yeast liked fungus of gemmation, which has a wide distribution in the nature world. It can also be parasitize in normal human skin and the oral, gastrointestinal, anal and vaginal mucosa, with no occurrence of diseases. It is a typical conditional pathogen. Candida albicans is a common pathogen. Only when the immunity of the human body is compromised, Candida albicans can cause diseases. The pathogenesis of Candida includes three aspects: (1) The compromised cellular immunity of the human body. Its manifestations include candida antigen skin test negative. When stimulated in vitro by Candida antigen, the lymphocyte transformation rate is low and reduced/absent macrophage migration inhibitory factor synthesis. The amount of phagocytes is reduced, with loss of the chemotaxis and declining ability to swallow and kill the pathogens. (2) The pathogen. The spore wall of Candida albicans is mainly composed of glycogen and mannan which could strengthen the adhesion of Candida albicans to cause infection. (3) Iatrogenic factor. Iatrogenic factor includes the administrations of broad spectrum antibiotics, adrenal cortical hormone, and immunosuppressants, which provide chances for the invasion of the pathogens.
25.2.1.2 Pathological Basis
The histopathological changes include inflammatory (such as the skin, lungs), purulent (such as kidney, lung and brain) or granulomatous (such as skin). Special organs and tissues can also have special manifestations. For instances, ulceration occurs in the esophagus and small intestine; proliferative changes occur in the cardiac valves; micro-abscesses occur in the cases of acute disseminated diseases with spores and hyphae in the abscesses and external infiltration of the neutrophils and histocytes. Surrounding the spore, there occasionally are eosinophilic materials, like astral body. Sometimes, the hyphae invade into the vascular wall. The histopathological findings of hyphae have diagnostic value.
25.2.1.3 Clinical Symptoms and Signs
Candida erythema commonly occurs in the skin folds, such as the gluteal fold, groin, under the breast, axillary, umbilical fossa, as well as the labia. The manifestations include erythema erosion and dipping whitish membranous scales, with clear boundary, surrounding red macula, blisters or pustules, and sense of itches. It is common in patients with diabetes, overweight and hidrosis. Due to the immunodeficiency of AIDS patients, systemic skin candidiasis may occur, with manifestations of widespread erythema and scales lesions with clear boundary, scattered surrounding papules or vesicles. It is often accompanied by thrush or gastroenteritis.
25.2.1.4 Examinations and Their Selection
Direct Microscopy
It is the most commonly used examination.
Staining
Microscopy after staining has a higher detection rate, comparing to the direct microscopy.
Isolation and Culture
The patients with smears negative findings should receive Candida culture.
Case Study 1
A female patient aged 43 years was confirmatively diagnosed as having AIDS by the CDC. Her CD4 T cell count was 78/μl.
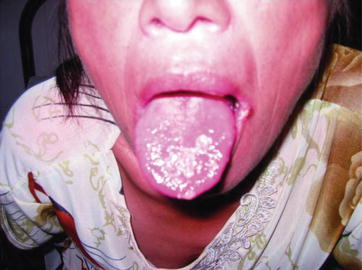
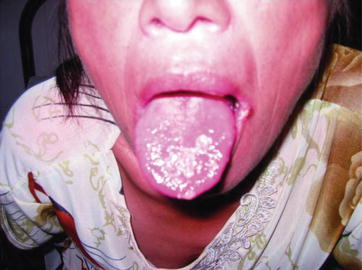
Fig. 25.1
HIV/AIDS related oral mucosa candidiasis. The gross observation demonstrates diffuse scattering whitish mucous plaques on the surface of the tongue
Case Study 2
A female patient aged 55 years was confirmatively diagnosed as having AIDS by the CDC. Her CD4 T cell count was 98/μl.
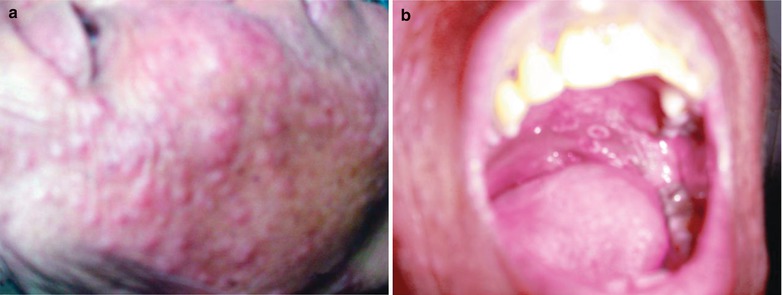
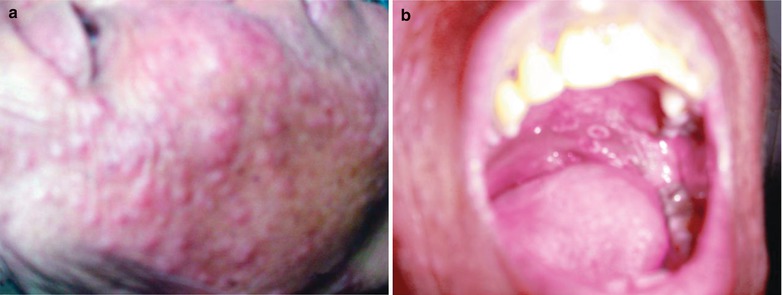
Fig. 25.2
(a, b) HIV/AIDS related skin and oral mucosa candidiasis. (a) The gross observation demonstrates diffuse scattering grayish white papules on the face. (b) The gross observation demonstrates white plaques and ulcers in the oral upper palate.
25.2.2 HIV/AIDS Related Cryptococcal Infection
25.2.2.1 Pathogen and Pathogenesis
Compromised immunity is an important factor inducing cryptococcal infection. Cryptococcal infection is rarely infected via skin contacts to Cryptococcus contaminated objects. Systemic cryptococcal disease with local manifestations is more common, which may be caused by spreading from meningeal, pulmonary or other lesions.
25.2.2.2 Pathophysiological Basis
The basic pathological changes have two kinds: early diffuse infiltrative exudative changes, and later granuloma formation. In the early lesions, there are large quantity Cryptococcus neoformans gathering, encapsulated thallus by colloid capsule that avoids direct contacts between the thallus and the surrounding tissues. Therefore, the inflammatory responses of the tissue are not obvious. Granuloma formation occurs sever months after the infection, with proliferated giant cells, macrophages and fibroblasts, infiltration of lymphocytes and plasma cells, and occasional occurrence of necrosis and small cavities.
25.2.2.3 Clinical Symptoms and Signs
Skin Cryptococcus infection has manifestations of acne liked skin rash, papules, hard nodules, and granuloma. The lesions have central necrosis, ulceration and fistula. The mucosal lesions are commonly found in the oral cavity and nasopharynx, with manifestations of nodules, ulceration and granuloma, with coverage of the surfaces with adhesive exudative thin membrane.
25.2.2.4 Examinations and Their Selection
Pathogenic Examinations
India ink staining is a rapid, simple and reliable method. Its repeated application has a high detection rate.
Serological Tests
The examination of the antibody has low positive rate, with low specificity. It is applied as a facilitative examination for the diagnosis.
Case Study 1
A female patient aged 34 years was confirmatively diagnosed as having AIDS by the CDC. Her CD4 T cell count was 118/μl.
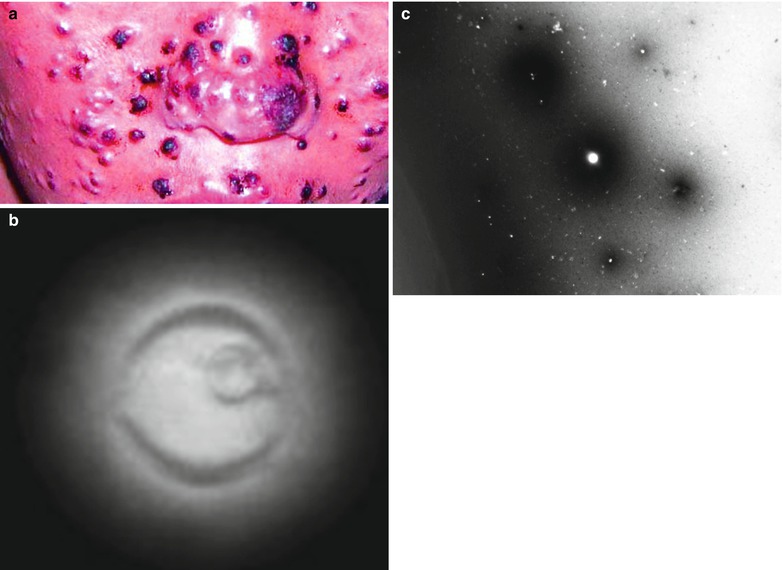
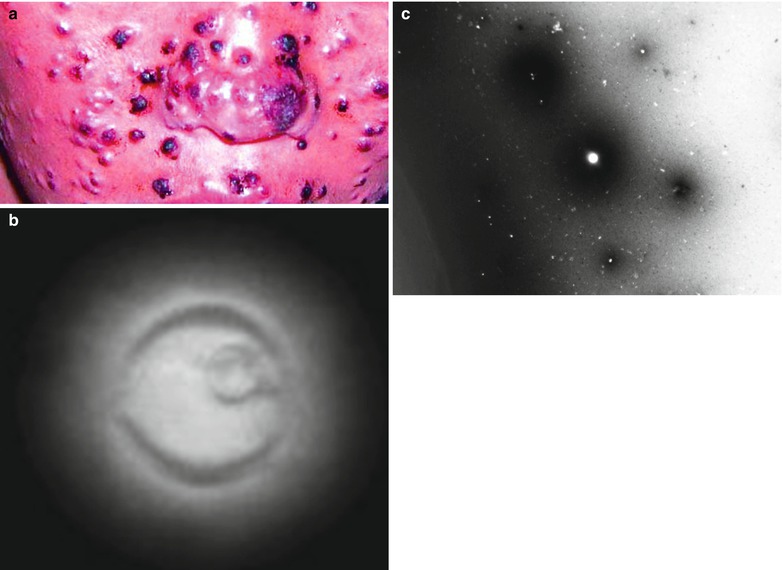
Fig. 25.3
(a–c) HIV/AIDS related skin cryptococcal infection. (a) The gross observation demonstrates diffuse scattering purplish black papules on the face. (b, c) Ink staining and light microscopy demonstrate cryptococcal cystozooid
Case Study 2
A female patient aged 46 years was confirmatively diagnosed as having AIDS by the CDC. Her CD4 T cell count was 58/μl.
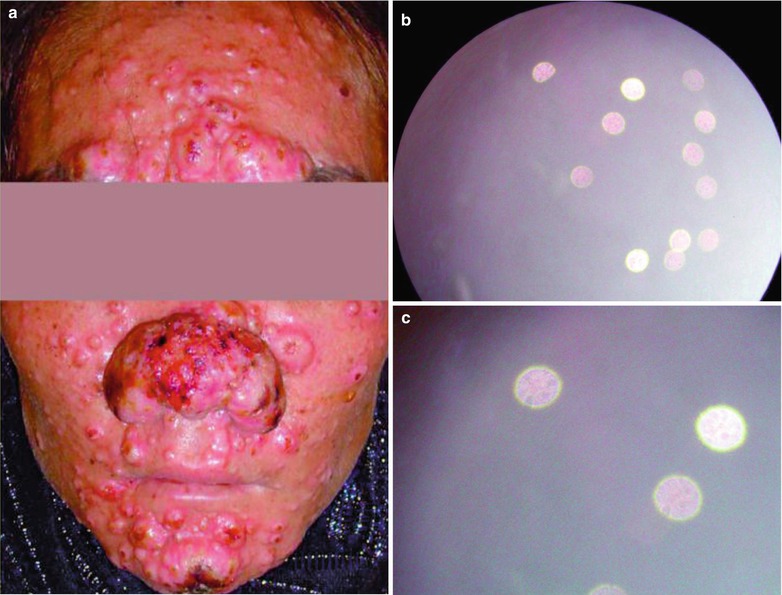
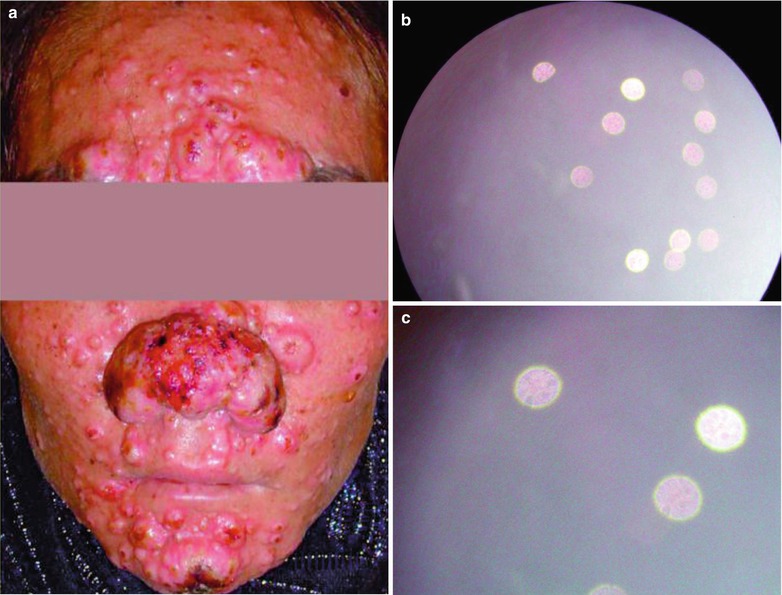
Fig. 25.4
(a–c) HIV/AIDS related skin cryptococcal infection. (a) The gross observation demonstrates diffuse scattering purplish red papules on the face. (b, c) Ink staining and light microscopy demonstrate cryptococcal cystozooid
25.2.3 HIV/AIDS Related Histoplasmosis Infection
25.2.3.1 Pathogen and Pathogenesis
Histoplasma is a biphasic fungus. It is in the yeast phase in the tissues and grows in the cells. By HE staining, round or oval globules can be found, with surrounding transparent halo like a capsule and a diameter of merely 2–4 um. PAS bacteria are slightly larger, with surround red stained cell wall to take the place of the capsule liked halo (actually the fungus has no capsule). It is highly contagious and can cause laboratory infection. The disease is caused by capsular histoplasmosis, which invades the human body via the skin. Its access into the human body causes primary or disseminated infections in people with compromised immunity.
25.2.3.2 Pathophysiological Basis
The pathological basis is the non-specific inflammatory infiltration of primary histoplasmosis. Occasionally, the macrophages and necrotic area can be found. In the macrophages, there are large quantity pathogenic fungi; and histocytes with swallowed spores can also be found in the regional lymph nodes. In the early period, there is central proliferation, with more or less fungi in the macrophages. After that, tissue necrosis occurs, with surrounding granuloma changes and final fibrosis to heal.
25.2.3.3 Clinical Symptoms and Signs
Skin histoplasmosis has hard plaques, nodules and subcutaneous nodules of erythema liked changes.
25.2.3.4 Examinations and Their Selection
Pathogenic Examinations
The finding of Histoplasma capsulatum in specimens has decisive significance for the diagnosis of the disease. Culture is still the only basis for the definitive diagnosis.
Serological Tests
In the early period, the latex agglutination test is positive. Immunodiffusion facilitates to differentiate the active lesions from non-active lesions. It is commonly positive in 2–5 weeks after the onset of symptoms.
Fluorescent Antibody Assay
It can facilitate the diagnosis. Complement fixation test can also be used for the screening test.
25.2.4 HIV/AIDS Related Superficial Fungal Infections
Case Study 1
A male patient aged 46 years was confirmatively diagnosed as having AIDS by the CDC. His CD4 T cell count was 153/ μl.


Fig. 25.5
HIV/AIDS related superficial fungal infection. The gross observation demonstrates vertex sparse hairs, and white scalp decrustation
Case Study 2
A female patient aged 36 years was confirmatively diagnosed as having AIDS by the CDC. Her CD4 T cell count was 73/μl and she sustained skin aspergillus infection.
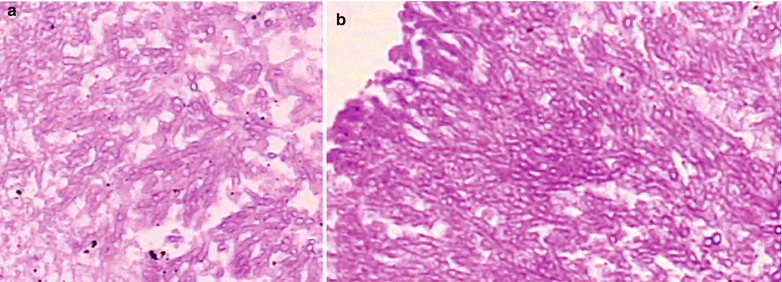
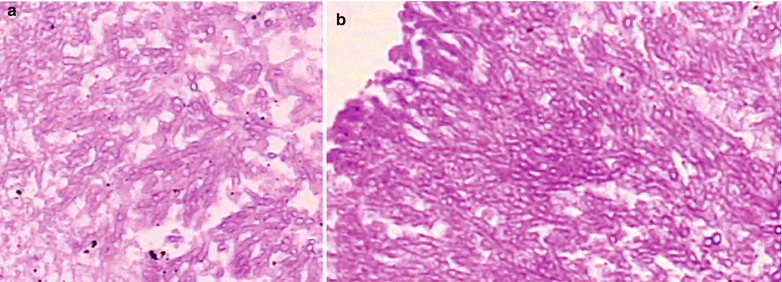
Fig. 25.6
(a, b) HIV/AIDS related fungal infection. Pathological biopsy demonstrates diffuse Aspergillus hyphae under a microscope
Case Study 3
A male patient aged 46 years was confirmatively diagnosed as having AIDS by the CDC. His CD4 T cell count was 13/ μl.
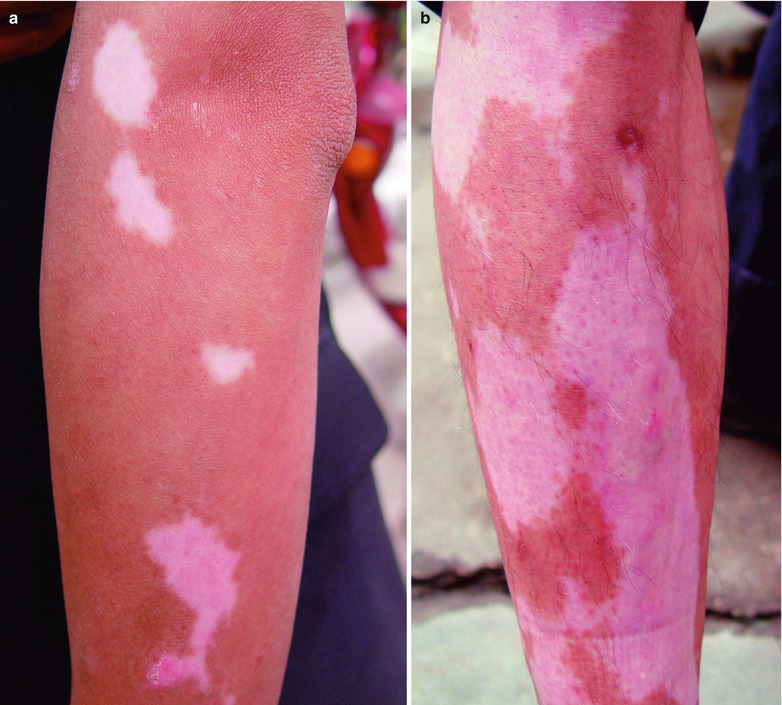
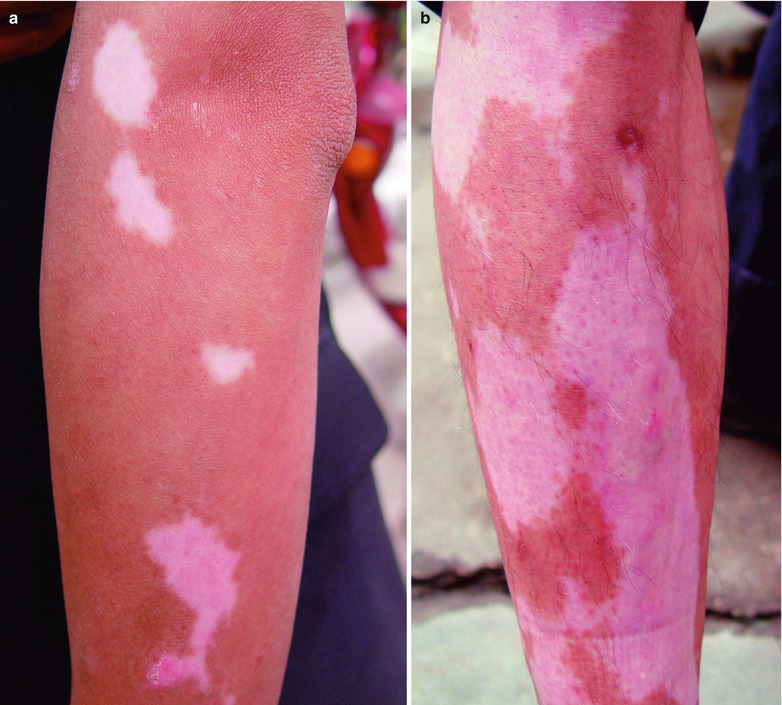
Fig. 25.7
HIV/AIDS related superficial fungal infection. (a, b) The gross observation demonstrates pink and white plaques on the skin surface
25.3 HIV/AIDS Related Parasitic Infections
25.3.1 HIV/AIDS Related Cutaneous Leishmaniasis
25.3.1.1 Pathogen and Pathogenesis
Since the mid 1980s, leishmaniasis in HIV patients has been increasing dramatically. Leishmaniasis is a zoonotic disease caused by Leishmania and it transmits between arthropods and mammals, with occurrence in more than 80 countries. It has been estimated that the total number of infected patients is up to more than 15 million and the newly emerging cases are more than 0.4 million per year. For the HIV positive patients, leishmania may be a opportunistic pathogenic parasite.
25.3.1.2 Pathophysiological Basis
The amastigote of leishmania can parasitize in macrophages and other phagocytic cells, such as monocytes and neutrophil. It causes chronic diffuse cells (including macrophages, lymphocytes and plasma cells) infiltration and the formation of micro granuloma with intact structure in patients with immunodeficiency.
25.3.1.3 Clinical Symptoms and Signs
Cutaneous leishmaniasis has two types: confined and diffuse. The manifestations include singular papula and nodule, with no occurrence of ulceration.
25.3.1.4 Examinations and Their Selection
Pathogenic Diagnosis
The finding of amastigote in cytological or histological examinations can define the diagnosis.
Immunological Diagnosis
The immunological assays include leishmania antibodies examination and cytoimmunological assay, both with high sensitivity.
25.3.2 HIV/AIDS Related Toxoplasma Infection of Skin
25.3.2.1 Pathogen and Pathogenesis
Skin toxoplasmosis is caused by toxoplasma gondii.
25.3.2.2 Pathophysiological Basis
It is pathologically manifested as (1) inflammatory cell infiltration, and sometimes formation of granulomas to involve the blood vessels and skin appendages; (2) vascular changes of capillary dilation, endothelial cells proliferation, venules necrosis and perivasculitis; (3) squamous epithelial cells proliferation, with the demonstration of epitheliomatous symptom in some serious cases.
25.3.2.3 Clinical Symptoms and Signs
The manifestations include skin rashes, commonly in the face, trunk and limbs; and secondary scarlet fever liked desquamation. There are also high fever and general upset.
25.3.2.4 Examinations and Their Selection
Pathogenic Examinations
The finding of the pathogen by histopathological examinations is a reliable basis for the diagnosis.
Immunological Assays
It is the main basis to define the diagnosis.
25.4 HIV/AIDS Related Viral Infections
25.4.1 HIV/AIDS Related Skin Herpes Simplex Virus Infection
25.4.1.1 Pathogen and Pathogenesis
This disease caused by herpes simplex virus of DNA virus. Herpes simplex virus (HSV) can be divided into two types: HSV-1 and HSV-2. HSV-1 often causes the lips and corneal herpes while HSV-2 causes genital herpes which mainly spreads by direct contacts to the lesions (sexual contacts) to result in skin lesions. They can be primary and recurrent herpes.
25.4.1.2 Pathophysiological Basis
Approximately 22 % cases of AIDS are complicated by herpes simplex. According to the diagnostic criteria by the CDC, chronic mucous herpes simplex or disseminated herpes simplex indicate the HIV infection has progressed in to AIDS.
25.4.1.3 Clinical Symptoms and Signs
Clinically, the lesions are erosions and ulcers with irregular margins, which is formed by rupture of intensive small blisters. Herpes simplex has atypical manifestations, with palm blisters or bullous lesions.
25.4.1.4 Examinations and Their Selection
Pathological Examinations
The finding of macrophages or intranuclear inclusions by biopsy has diagnostic significance.
Serological Tests
The finding has diagnostic significance, but it has false negative findings.
Case Study 1
A female patient aged 36 years was confirmatively diagnosed as having AIDS by the CDC. Her CD4 T cell count was 18/μl.
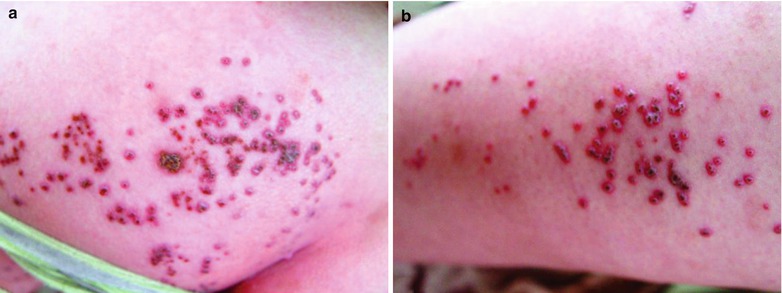
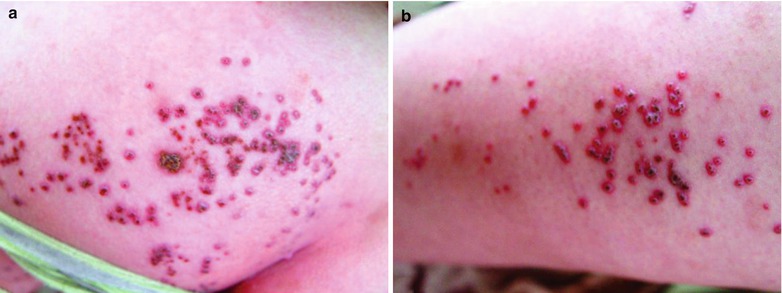
Fig. 25.8




(a¸ b) HIV/AIDS related skin herpes simplex virus infection. The gross observation demonstrates herpes simplex ulceration and scab on the buttocks and thighs, and newly emerging herpes
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree