High-resolution computed tomography (HRCT) is widely used in the evaluation of a variety of diffuse lung diseases. The goal of this introductory chapter is to discuss the basics of HRCT, including indications, technique, and normal lung anatomy, as displayed using this modality.
INDICATIONS FOR HRCT
HRCT has several indications and uses in patients with, or suspected of having, diffuse lung disease (Table 1.1).
Detection of Diffuse Lung Disease
HRCT can be more sensitive and specific in the diagnosis of diffuse lung disease than other diagnostic tests (Fig. 1.1A, B), including plain radiographs and pulmonary function tests. For instance, HRCT may detect abnormalities in asymptomatic patients with connective tissue disease or other conditions, or with various exposures, before pulmonary function tests become abnormal. Detecting abnormalities at an early stage may allow for appropriate treatment, preventing progression of lung disease.
Table 1.1 Indications for HRCT
Detection of diffuse lung disease
• Detect abnormalities before other tests (e.g., chest x-ray) become abnormal
• Exclude certain diseases as a cause of symptoms
Characterization of diffuse lung disease
• Identification of specific abnormalities
• Formulation of a differential diagnosis
• Determine if reversible or irreversible abnormalities are likely present
• Help determine prognosis
Differential diagnosis and guidance for further testing
• HRCT findings (with clinical information) may be sufficiently diagnostic
• HRCT findings may suggest the appropriate study
• tree-in-bud: sputum analysis
• perilymphatic nodules or possible infection: transbronchial biopsy
• nonspecific diffuse lung disease: video-assisted thoracoscopic surgical lung biopsy
Sequential evaluation of abnormalities over time
• Response to treatment
• Assess patients with new symptoms
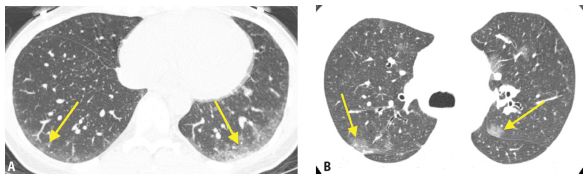
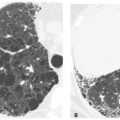
Figure 1.1
Detection of early lung disease. HRCT may be more sensitive than other tests in detecting diffuse lung disease. A. Mild subpleural ground glass opacity (arrows) is seen in a patient with nonspecific interstitial pneumonia associated with scleroderma. This patient has a normal chest x-ray and pulmonary function tests. B. In a patient with acquired immune deficiency syndrome and a normal chest x-ray, patchy ground glass opacity (arrows) is visible on HRCT. Bronchoscopy confirmed Pneumocystis jiroveci infection.
HRCT may also be used to exclude certain lung diseases as a cause of symptoms or abnormal pulmonary function test findings. For example, in patients with pulmonary hypertension, HRCT may be used to exclude emphysema and fibrotic lung disease as causative etiologies. As another example, in patients with acquired immune deficiency syndrome and a suspicion of Pneumocystis jiroveci infection, HRCT has a high negative predictive value, and further testing, such as bronchoscopy, is not generally required if the study is normal.
Characterization of Diffuse Lung Disease
The primary role of HRCT is in the identification of specific abnormalities that allow a characterization of diffuse lung disease and formulation of a differential diagnosis. The type and specific location of lung abnormalities may be determined using HRCT, and it may be suggested whether the disease present is primarily inflammatory or fibrotic or whether it is an airways disease (Fig. 1.2), interstitial disease, or alveolar (airspace) disease (Fig. 1.3).
HRCT findings may have important implications for treatment and prognosis. When findings of fibrosis are present on HRCT, patients are less likely to respond to various medications and, in general, have a poorer prognosis. Patients with HRCT findings suggestive of inflammation are generally treated more aggressively in the hope that the lung findings are reversible. HRCT is helpful in making this distinction.
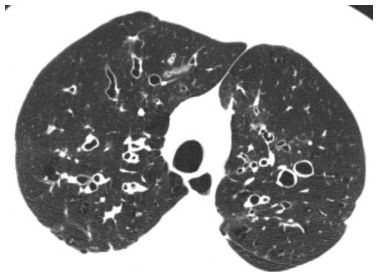
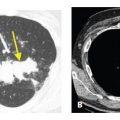
Figure 1.2
HRCT characterization of lung disease. HRCT allows the diagnosis of airways disease in this patient with chronic symptoms. It provides an accurate assessment of both acute and chronic abnormalities in patients with airways disease. Bronchiectasis, airway wall thickening, and luminal impaction are present in this patient with cystic fibrosis.
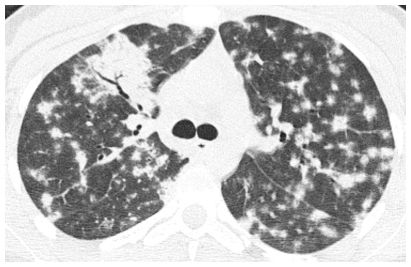
Figure 1.3
HRCT characterization of lung disease. HRCT provides an accurate diagnosis of diffuse alveolar or airspace disease in a patient with patchy consolidation and an air bronchogram. In this example, patchy nodular areas of peribronchovascular and subpleural consolidation are present in a patient with organizing pneumonia.
Differential Diagnosis and Guidance for Further Diagnostic Testing
HRCT is more specific than chest radiography, physical examination, and pulmonary function tests in the diagnosis and characterization of lung abnormalities in patients with diffuse lung disease (Fig. 1.4A, B), and some HRCT findings may be highly suggestive of a specific disease. Nonetheless, most HRCT abnormalities are nonspecific and require a differential diagnosis.
The diagnosis of diffuse lung disease is generally based on a multidisciplinary approach, incorporating clinical information, HRCT findings, and sometimes pathology. Infrequently, one of these is sufficient to make a definitive diagnosis, and a combination of at least two is usually required to maintain a high degree of diagnostic accuracy and confidence. When HRCT is interpreted in conjunction with clinical information, the accuracy and specificity of diagnosis improve significantly (Table 1.2). Examples of clinical information useful in the diagnosis of diffuse lung abnormalities include patient age, duration of symptoms, a history of cigarette smoking, exposures (e.g., inhalational and environmental), immune status, drug treatment, and known systemic disorders such as connective tissue disease.
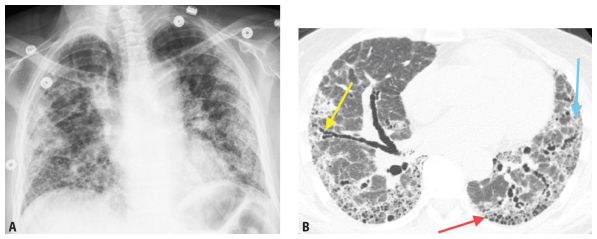
Figure 1.4
Specificity of HRCT. A. Frontal chest radiograph in a patient with idiopathic pulmonary fibrosis (IPF) shows diffuse nonspecific opacities. B. HRCT provides superior evaluation of lung abnormalities. Subpleural honeycombing (red arrow), traction bronchiectasis (yellow arrow), and irregular reticulation (blue arrow) are present. In the absence of known diseases or exposures, HRCT is considered diagnostic of IPF.
Table 1.2 Clinical information that may be useful in the interpretation of HRCT abnormalities
Age
Acute or chronic symptoms
Cigarette smoking
Exposures (drugs, dusts, and organic antigens) Immune status
Connective tissue disease
In many cases, a combination of HRCT findings and clinical information may predict a single diagnosis with a high degree of accuracy (Fig. 1.5A, B). In such cases, further diagnostic testing may not be needed. For instance, when centrilobular nodules of ground glass opacity are present on HRCT in a patient with an exposure to birds, the diagnosis is very likely hypersensitivity pneumonitis. In such cases, biopsy is not usually required for diagnosis. Another example is an HRCT showing honeycombing in a subpleural and basilar distribution. This pattern is compatible with usual interstitial pneumonia (UIP) and a biopsy is not generally required for confirmation. In the absence of known diseases or exposures, the patient will be diagnosed as having idiopathic pulmonary fibrosis (IPF).
On the other hand, when the HRCT pattern is nonspecific, the suggested differential diagnosis may help to guide additional tests. For example, when tree-in-bud opacities are present on HRCT, a diagnosis is often obtained using sputum analysis, as this finding usually reflects an infectious cellular bronchiolitis with impaction of small airways. In patients with perilymphatic nodules visible on HRCT, there is a high likelihood of obtaining a histologic diagnosis on transbronchial biopsy, as this abnormality is often due to sarcoidosis or lymphangitic tumor spread (Fig. 1.6). Transbronchial biopsy is useful in the diagnosis of these two diseases, because they involve the airways or predominate in the peribronchovascular interstitium. It is also helpful in diagnosing some infections, when sputum analysis is not sufficient. Histologic samples obtained at transbronchial biopsy, however, have significant potential limitations, primarily because they represent small samples of lung, and the samples obtained may not be representative of the overall process that is present. HRCT, on the other hand, provides a global evaluation of the lung abnormalities present (Fig. 1.7).
Lung biopsy is obtained in cases in which the combination of clinical information and HRCT is not considered sufficient for diagnosis. Video-assisted thoracoscopic surgical (VATS) biopsies are most helpful as they obtain relatively large samples from multiple locations within the lung. In patients with nonspecific fibrosis on HRCT, a VATS biopsy is usually required for diagnosis. HRCT may help guide the surgeon to the most appropriate regions for biopsy. It is important to recognize, however, that even if a VATS biopsy is obtained, it is often important to consider it in association with the HRCT abnormalities.
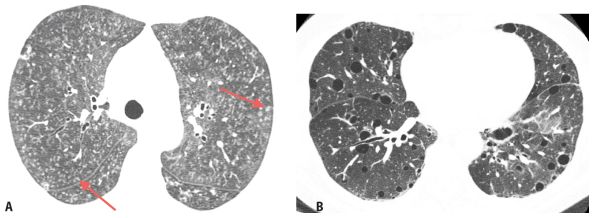
Figure 1.5
Correlation of HRCT findings with clinical information. A. HRCT shows diffuse indistinct centrilobular nodules (arrows). There are several possible diagnoses based upon the HRCT pattern. This patient has chronic symptoms and a history of recurrent exposure to birds. This combination of HRCT findings and clinical information is highly suggestive of hypersensitivity pneumonitis. B. HRCT in a patient with Sjögren’s syndrome shows scattered lung cysts. While this finding is nonspecific, in a patient with a history of connective tissue disease, it is highly suggestive of lymphoid interstitial pneumonia.
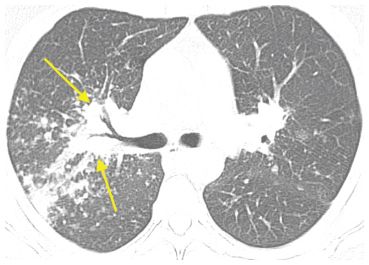
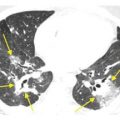
Figure 1.6
HRCT in sarcoidosis. HRCT shows clusters of nodules in the interstitium around the central bronchovascular bundles (arrows) suggestive of sarcoidosis. Given the proximity of these findings to the airways, bronchoscopy with transbronchial biopsy is the test of choice for confirmation of this diagnosis.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree