Chapter 35 Imaging in Thyroid Cancer
Introduction
Although thyroid cancer represents less than 1% of all malignancies worldwide, it is currently one of the most rapidly increasing malignancies in the Western world.1 Thyroid nodules can be palpated in 4% to 7% of patients and can be detected on imaging in approximately 50% of the general population.1–3 Five percent of these nodules represent cancer.1,2 With newly available imaging modalities, more and more asymptomatic and nonpalpable nodules are detected, making it imperative that primary care doctors and radiologists understand how to interpret these diagnostic studies, understand indications for further referral, and manage the long-term survivors of thyroid cancer. Most of the patients who have thyroid cancer have well-differentiated cancers, with an excellent long-term prognosis. Some patients have well-differentiated cancers with a poor prognosis, and some have other less common types of thyroid cancers. The challenge for the clinician is to identify the patients who have cancers, to treat them according to the extent and aggressiveness of their disease, and to limit morbidity and mortality.
Epidemiology and Risk Factors
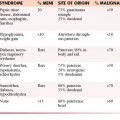
Over the last few decades, the incidence of thyroid cancer has increased dramatically. It is unclear whether this increased incidence is real or whether it may be attributable to increased detection by newer diagnostic imaging techniques.4,5 Autopsy studies have shown that up to 30% of adults have incidental cancers smaller than 1 cm at the time of death.6 The average age of diagnosis of thyroid cancer is 47 years, and the average age of death is 74 years.5 The most common type is the papillary thyroid cancer (PTC); it accounts for approximately 70% of all thyroid cancers. Follicular thyroid carcinoma (FTC) represents approximately 15% of cancers and, in combination with PTC, composes the category of well-differentiated thyroid carcinomas. Grouped into the less common cancers are medullary (4-6%), anaplastic (3-4%), and others (≤5%). This group may include lymphoma, sarcoma, squamous cell carcinoma, and metastases.5
The most significant environmental risk factor for developing thyroid cancer is prior exposure to ionizing radiation, which can be due to either medical treatment or nuclear fallout (e.g., atomic bomb/testing survivors, nuclear energy accidents). The effects of ionizing radiation are most pronounced in children, especially those younger than 10 years old at the time of exposure. The latency period of developing cancer from this exposure is approximately 10 years for patients having external beam radiation exposure to less than 5 years for victims of the Chernobyl nuclear accident in the Ukraine.7 The increased risk persists for 30 to 40 years.8,9 Patients presenting with benign thyroid disease may also be at higher risk of harboring a malignant nodule; for example, cold nodule found on radionuclide scanning in patients with Graves’ disease may be malignant 15% to 38% of the time and complex cysts in thyroid disease may harbor a malignancy approximately 17% of the time.7 Given that, overall, two thirds of thyroid cancer cases occur in women, there would seem to be a link between reproductive hormones and the development of thyroid cancer. Estrogen has been linked as a stimulus for genomic instability, which may explain how it exerts its mutagenic effects on the thyroid.10 There are no definite data on the role of dietary iodine and its role in the development of thyroid cancer.11 Certain genetic syndromes increase the risk for thyroid cancer, or are associated with thyroid cancer, especially medullary thyroid cancer, which has been linked to several specific genetic abnormalities. In some cases, PTC follows a familial pattern. Several rare genetic disorders, including Cowden’s disease, multiple endocrine neoplasia (MEN), and Gardner’s syndrome, are also associated with a higher incidence of thyroid cancer.5
Anatomy
The thyroid is a shield-shaped gland that consists of right and left lobes connected by the isthmus in midline, although occasionally, the isthmus can be absent. The thyroid isthmus is anterior to the trachea, usually overlying the first through the third tracheal rings. The thyroid gland typically terminates above the level of the clavicle; however, substernal extension into the superior mediastinum can occur. An accessory lobe, the pyramidal lobe, may be present in 50% to 70% of people and usually arises from the isthmus and extends superiorly.12 The visceral fascia, part of the middle layer of the deep cervical fascia, attaches the thyroid gland to the larynx and trachea. As a result, the gland or abnormalities related to it will move with the larynx during swallowing. The arterial supply to the gland is derived from two separate paired vessels. The inferior thyroid vessels come directly off of the thyrocervical trunk and supply the inferior part of the gland as well as both the superior and the inferior parathyroids. The superior thyroid artery arises as the first branch of the external carotid artery and supplies the superior portion of the gland. Rarely, a small artery or pair of arteries may come directly from the aorta or brachiocephalic trunk, named the thyroid ima artery. There are three main paired veins that drain the thyroid. There is some variability in location and presence, but they generally drain into the internal jugular veins and innominate vein. The lymphatics of the thyroid consist of intraglandular and extraglandular components. Extraglandular lymphatics generally follow venous flow; the inferior portions of the lateral lobes drain along the tracheoesophageal groove into the central neck. The superior parts of the lobes drain toward the superior thyroid veins, and the isthmus may drain toward the delphian (prelaryngeal) lymph node or central neck nodes. More unusual, but clearly documented, are lymphatic pathways to the retropharyngeal region, accounting for metastases to the skull base. Based on clinical and anatomic review, the central lymphatics are generally considered the primary drainage pathways for thyroid cancers, with the lateral neck nodes being considered secondary levels of lymphatic spread. These facts are important from an imaging and a treatment perspective.13 The parathyroid glands are also closely related to the thyroid anatomically. They tend to lie on the undersurface of the thyroid and receive their blood supply from the inferior thyroid artery.
Pathology
Tumor Types
Papillary Thyroid Carcinoma
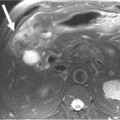
The most common type is the PTC, which accounts for approximately 70% of all thyroid cancers. This cancer has a favorable prognosis with most of the patients who are treated; either cured of their disease or live for many years after the initial diagnosis. Less than 50% of recurrences occur within the first 5 years, and sometimes recurrences can present several years after the initial diagnosis.12 The cancer often retains the ability to concentrate iodine, secrete thyroglobulin, and respond to thyrotropin-stimulating hormone (TSH) stimulation. There are several variants of PTC. The follicular variant of PTC has a pattern of neoplastic follicles that are small with little colloid. They contain relatively fewer nuclear inclusions and psammoma bodies. The prognosis and biologic behavior are similar to that of PTC. The tall cell variant has neoplastic cells in which the height is twice the width. It is associated with more aggressive biologic characteristics and tends to metastasize earlier in its course. It is common for PTC to demonstrate multifocal disease within the thyroid gland at the time of histologic examination. The incidence has been reported to be as high as 80% in the literature.5 Extrathyroidal extension of the tumor is seen and has prognostic significance.14 The overlying strap muscles in the neck are the most commonly invaded structures. Cases of tracheal, laryngeal, esophageal, and other soft tissue extensions in the neck are sometimes seen.
Follicular Thyroid Carcinoma
FTC is the second most common type of thyroid cancer. It represents approximately 15% of thyroid cancers. Many authors have suggested that the prognosis is slightly poorer than that for PTC. Both benign and malignant follicular lesions demonstrate follicular cells arranged in microfollicles, rosettes, or spindles, and thus, they cannot be differentiated on fine-needle aspiration. Capsular invasion is the only current method of distinguishing between the two entities, and hence, quite often, the diagnosis is made after surgery, unless extracapsular extension is seen on imaging before surgery. In patients who have minimal capsular invasion, the prognosis is excellent, and few patients develop distant metastases or die of disease.5,15 Unfortunately, patients with capsular invasion have worse prognosis. Young patients and women may have a slightly better prognosis than men. Clinically, FTCs tend to present with a solitary thyroid mass. The incidence of multicentric disease within the thyroid is much lower than with PTC.
Hurthle Cell Carcinoma
Hurthle cell carcinoma is a variant of FTC, accounting for 3% to 5% of all thyroid cancers.16 It is composed of large acidophilic or oncocytic cells that do not take up radioiodine as well as classic FTC. Like FTC, the diagnosis can be made only after examination of the entire tumor capsule. The cancers generally have a slightly worse prognosis than other FTCs. They are associated with a higher rate of lymph node and distant metastasis than other FTCs.17
Medullary Thyroid Carcinoma
Medullary thyroid carcinoma (MTC) arises from the parafollicular or C cells, which are a part of the amine precursor uptake and decarboxylation (APUD) cell system. These cells produce calcitonin and are unrelated to the iodine-concentrating and thyroid hormone production of the gland. MTC is more closely related to other tumors of the neuroendocrine system such as the carcinoid tumors and pheochromocytomas. MTC is rare, accounting for 3% to 5% of thyroid cancers.5 The familial form, which is less common than the sporadic form of MTC, is inherited as an autosomal dominant trait. It can be inherited as a part of three distinct entities. The most common, MEN IIA, is associated with pheochromocytoma and hyperparathyroidism. The second most common, MEN IIB, is associated with pheochromocytoma, mucosal neuromas, and marfanoid body habitus. The least common, familial medullary thyroid cancer (FMTC), consists of MTC only. The presence of MTC has been strongly linked to the RET oncogene, located on chromosome 10. The discovery of this gene mutation has been studied extensively and has had a significant effect on diagnosis, management, and understanding of these tumors.5 Clinically, patients tend to present with a solitary thyroid nodule. Some patients present with an enlarging neck mass or, rarely, with signs of local invasion, including hoarseness or dysphagia. Some patients can present with paraneoplastic syndromes, such as Cushing’s or carcinoid syndrome.
Anaplastic Thyroid Carcinoma
Anaplastic thyroid cancer is an aggressive disease, usually proving fatal within several weeks to months of diagnosis. It represents approximately 3% to 5% of thyroid cancers.5 This cancer tends to affect elderly patients, and the peak incidence is in the seventh decade.18 Some investigators believe that anaplastic carcinoma may represent a dedifferentiation of well-differentiated cancers.19 Clinically, patients present with a rapidly growing neck mass, often in the context of a slow-growing mass or goiter for several decades. Patients often present with signs of local invasion such as dysphagia, dyspnea, hoarseness, sore throat, and neck pain.
Lymphoma of the Thyroid Gland
Lymphoma of the thyroid has been reported to make up 2% to 5% of thyroid cancers.20 It tends to be non-Hodgkin’s B-cell type, although other types do occur. Patients with Hashimoto’s disease (chronic lymphocytic thyroiditis) have a 70-fold increased incidence of thyroid lymphoma compared with the general population.20 It is suspected that chronic autoimmune stimulation is responsible for the development of this cancer.20 Many lymphomas can be diagnosed cytologically, based on their monoclonality. Differentiating them from anaplastic carcinoma is often challenging, however, and it is not uncommon to require core or open biopsy to make an accurate diagnosis. In the clinical setting, lymphoma also mirrors anaplastic carcinoma in many ways. It tends to present with a rapidly expanding mass in the neck, often fixed to surrounding structures. Patients often have neck pain, hoarseness, dysphagia, and even facial edema. The tumor is often fixed to surrounding structures, including the trachea and larynx, the esophagus, and the skin.
Other Cancers of the Thyroid
Although rare, several other cancers can involve the thyroid, either primarily or through metastasis. Squamous cell carcinoma is a rare primary cancer of the thyroid. Once diagnosed, a thorough workup must be performed to rule out a head and neck primary that has merely metastasized to the thyroid. Metastatic cancer to the thyroid is also rare, although well documented. It is suspected that the significant vascularity of the gland accounts for these metastases. Cancers of the kidney, lung, breast, and melanoma are the most commonly documented.5 In patients who have a known history of other primary cancers who have a new thyroid mass, the possibility of metastatic disease must be entertained.
Gross and Microscopic Features
On gross pathology, PTC is poorly encapsulated, firm, and often has calcifications (psammoma bodies) within their substance. The presence of these calcifications is of diagnostic significance, because they are rarely present in other cancers. Larger tumors may contain focal areas of hemorrhage and necrosis. PTC demonstrates papillary fronds along with follicular components. The nuclei have a characteristic appearance, with a feature described as “Orphan Annie eyes” used to refer to the relatively empty appearance of the nucleoplasm.5
FTC has a thick capsule with focal necrosis and cystic changes.21 The cells are small and monotonous and organized into follicles with sparse amount of colloid. Psammoma bodies are rare compared with PTC.
MTCs are well-encapsulated tumors. Histologically, the tumor demonstrates amyloid depositions in 60% to 80% of cases.22 The tumor often displays nuclear pleomorphism, necrosis, and multiple mitosis. Calcitonin staining is also helpful, and the level of staining may reflect the level of cellular differentiation. Serum calcitonin levels are useful as a diagnostic and measure of response to therapy. MTC have been reported to secrete multiple polypeptide hormones, adrenocorticotropic hormone, somatostatin, vasoactive intestinal peptide, chromogranin A, neuron-specific enolase, and substance P.5 Carcinoembryonic antigen is also secreted by many MTCs and has been used as a tumor marker and a receptor for nuclear imaging with octreotide imaging.
Clinical Presentation
Most of the patients with thyroid cancer commonly self-diagnose a lump in their neck found during palpation. Other patients may present with a thyroid nodule detected incidentally on imaging ordered for other medical reasons. Other symptoms that may be seen in thyroid cancer include dysphagia, change in voice, coughing, choking, dyspnea, and pain. There may be a history of exposure to ionizing radiation and a family history of thyroid or parathyroid disease. Physical examination should assess for features of the nodule and for the presence of cervical lymphadenopathy. Suspicious features for cancer include nodules that are hard, fixed, irregular, 4 cm or larger, or with associated lymphadenopathy. A general rule to follow is that any lesion with two or more associated high-risk characteristics may have a malignancy rate greater than 80%.23
Patterns of Tumor Spread
Regional metastasis to the neck and mediastinal lymph nodes is the common pattern of spread for PTC, with incidence rates from 40% to more than 75%.24 The role of regional metastasis on overall prognosis of PTC is still being debated.12,25 Unlike regional metastasis, distant metastasis does seem to adversely affect prognosis. Approximately 10% of patients demonstrate metastasis to distant sites, most commonly to the lungs, brain, and bones.26
Patients with anaplastic tumors may demonstrate cervical metastasis. Distant metastasis tends to be to the lungs, although other sites, including bone, brain, and mediastinum, have been demonstrated.27
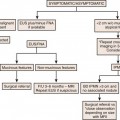
Staging Evaluation
Table 35-1presents the tumor-node-metastasis (TNM) system diagnosis.28
Table 35-1 Tumor-Node-Metastasis System Diagnosis
| Primary Tumor (T) |
| TXPrimary tumor cannot be assessed |
| T0No evidence of primary tumor |
| T1Tumor ≤ 2 cm in greatest dimension limited to the thyroid |
| T2Tumor ≥ 2 cm but not > 4 cm in greatest dimension limited to the thyroid |
| T3Tumor > 4 cm in greatest dimension limited to the thyroid or any tumor with minimal extrathyroid extension (e.g., extension to sternothyroid muscle or perithyroid soft tissue) |
| T4a Tumor of any size extending beyond the thyroid capsule to invade subcutaneous soft tissues, larynx, trachea, esophagus, or recurrent laryngeal nerve |
| T4b Tumor invades prevertebral fascia or encases carotid artery or mediastinal vessels |
| All anaplastic carcinomas are considered T4 tumors: |
| T4a: Intrathyroid anaplastic carcinoma–surgically resectable |
| T4b: Extrathyroid anaplastic carcinoma–surgically unresectable |
| Note: All categories may be subdivided: (a) solitary tumor or (b) multifocal tumor (the largest determines the classification). |
| Regional Lymph Nodes (N) |
| Regional lymph nodes are the central compartment and lateral cervical and upper mediastinal lymph nodes |
| NXRegional lymph nodes cannot be assessed |
| N0No regional lymph node metastasis |
| N1Regional lymph node metastasis |