Location
Tumor
Neck
Cystic hygroma – lymphangioma
Sternocleidomastoid muscle
Capillary hemangioma
Fibromatosis colli
Trunk
Askin (PNET) tumor
Axilla
Cystic hygroma-lymphangioma
Upper limb
Wrist
Ganglion cyst
Wrist, volar aspect
Fibrolipohamartoma of median nerve
Hand, volar aspect
Fibrolipohamartoma of median nerve
Finger, dorsal aspect
Digital fibroma
Lower limb
Thigh
Fibrohamartoma of infancy
Knee
Synovial hemangioma
Knee, tibiofibular joint
Ganglion cyst
Ankle
Ganglion cyst
Foot, extensor aspect
Ganglion cyst
Upper and lower limbs
Myositis ossificans
Hand and feet
Calcifying aponeurotic fibroma
Joints, periarticular
Synovial hemangioma
Cutis, subcutis
Dermatofibrosarcoma protuberans

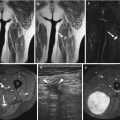
Fig. 25.1
Fibromatosis colli in 6-week-old boy. (a) Ultrasound shows a heteroechoic thickening of the central part of the sternocleidomastoid muscle. (b–d) Axial and sagittal T2-weighted MR images show a hypointense focal thickening (long arrows) of the right sternocleidomastoid muscle. The left sternocleidomastoid muscle (short arrow) is normal

Fig. 25.2
Granuloma annulare in a 3-year-old girl. (a, b) Axial T1-weighted images show a subcutaneous soft tissue lesion (arrows) enhancing after contrast administration. (c) Coronal fat-saturated (FS) T2-weighted MR image shows multiple ill-defined hyperintense lesions (arrows)

Fig. 25.3
Fibrosarcoma in a 1-year-old girl. (a–b) Coronal T1- and T2-weighted MR images show a large soft tissue mass in the right axilla. (c) Axial CE FS T1-weighted image depicts intense homogeneous enhancement of the lesion

Fig. 25.4
Synovial sarcoma in a 16-year-old-girl. Axial (a) FS T2-weighted and (b) CE FS T1-weighted MR images show a heterogeneous, partially enhancing mass in the soft tissues anterior of the shoulder

Fig. 25.5
Infantile rhabdomyosarcoma in a 1-day-old girl. (a, b) Axial and sagittal FS T2-weighted images show multiple soft tissue lesions (arrows) with cystic and solid components anterior to the nose and in the submandibular space. (c) Sagittal CE FS T1-weighted image shows enhancement of the solid components of the mass

Fig. 25.6
Infantile hemangioma in a 4-year-old boy. (a, b) Sagittal and coronal FS T2-weighted images show a soft tissue mass with flow voids (arrows) due to the presence of vessels with high flow. (c) Sagittal CE T1-weighted image shows intense homogeneous enhancement of the mass

Fig. 25.7
Infantile hemangioma in a 4-year-old boy. (a) Coronal FS T2-weighted image shows a soft tissue mass on the right side of the neck. (b) Axial CE T1-weighted image shows marked homogeneous enhancement of the mass
Location In children younger than 6 years of age, 60 % of benign and malignant lesions occur in the head and neck region, the lower extremity, or the trunk. In children of 6–15 years old, benign tumors often occur in the hand or wrist, the head and neck region, and the lower extremities [1, 2], whereas malignant soft tissue tumors are more common in the extremities or the trunk. Many of the primary sites of childhood rhabdomyosarcoma, such as the orbit, bladder, prostate, and paratesticular region, are rarely primary sites of the non-rhabdomyosarcoma tumors in children and of other soft tissue sarcomas in adults [1, 2].
25.2 The Role of Imaging
Benign masses with characteristic clinical presentation may be recognized by experienced clinicians and may not require imaging. Most cutaneous or subcutaneous masses are small and often excised without imaging.
Children frequently have nonspecific symptoms and complaints are often initially neglected or diagnosis may be delayed. As children often have injuries related to play, pain and soft tissue masses may be attributed to trauma. Therapeutic options and long-term survival of soft tissue tumors is strongly related to the disease stage at the time of diagnosis. This stresses the importance of performing timely and dedicated imaging studies.
Current methods of diagnosis such as dynamic contrast-enhanced MR imaging, PET scan, molecular biology, immunology, and cytogenetics give additional insight into the biology of tumors and may help us in tailoring therapeutic strategies according to these biologic and imaging characteristics.
Tables present the most common locations for tumors (Table 25.1), multiplicity (Table 25.2), different shapes associated with specific soft tissue tumors (Table 25.3), and specific MR features, including the presence of signal voids (Table 25.4) and fluid-fluid levels (Table 25.5) [4–25].
Table 25.2
Multiplicity
Venous malformation |
Lipoma (5–8 %) |
Neurofibroma |
Dermatofibrosarcoma protuberans |
Desmoid |
Table 25.3
Shape
Fusiform (ovoid) | Neurofibroma |
Lipoma | |
Dumbbell | Neurofibroma |
Moniliform | Neurofibroma |
Round | Cyst |
Schwannoma | |
Serpiginous | Hemangioma |
Lymphangioma |
Table 25.4
Intratumoral signal void
Flow | Hemangioma (capillary) |
Arteriovenous malformation | |
Calcification | Hemangioma (phlebolith) |
Lipoma (well differentiated and dedifferentiated) | |
Myositis ossificans (marginal) | |
Myofibromatosis |
Table 25.5
Fluid-fluid levels
Hemangioma |
Cystic lymphangioma |
Synoviosarcoma |
Hematoma |
25.3 Imaging Modalities
25.3.1 Ultrasound
The value of ultrasound is limited. In a study by Brouns et al. [27] about the delay in diagnosis of soft tissue sarcoma, wrong diagnosis on ultrasound was the most frequent reason for this delay.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree