FIGURE 10.1: Transvaginal sonographic appearance of a normal uterine cervix; the internal os, the external os, and the endocervical canal are easily visualized. (From Gomez R, Galasso M, Romero R, et al. Ultrasonographic examination of the uterine cervix is better than cervical digital examination as a predictor of the likelihood of premature delivery in patients with preterm labor and intact membranes. Am J Obstet Gynecol. 1994;171(4):956–964, copyright © 1994 with permission from Elsevier.)
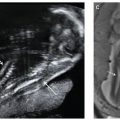
Excessive pressure with the probe may elongate the cervix. To avoid this pitfall, the probe is slowly withdrawn until the image blurs and pressure is subsequently reapplied to restore the image. This can be avoided by confirming equal cervical width and density of the anterior and posterior lips of the endocervical canal (Fig. 10.2).60,61
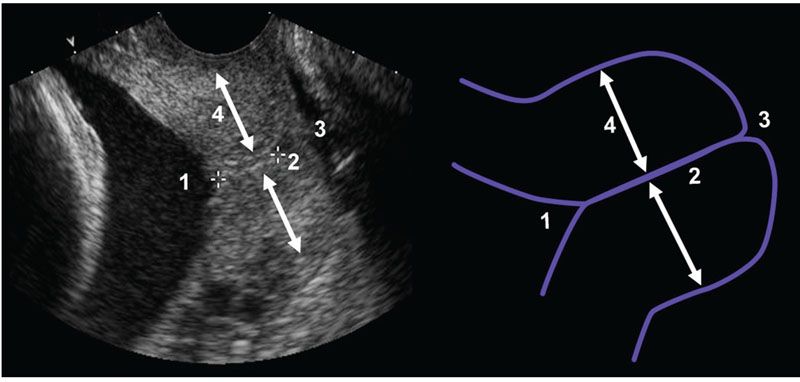
FIGURE 10.2: Transvaginal sonographic appearance of a cervix with a schematic to display common pitfalls and landmarks: (1), internal os; (2), visualization of entire endocervical canal; (3), external os; (4), the distance between the anterior lip of the cervix to the cervical canal and the posterior lip of the cervix and the cervical canal are equal. (Reproduced with permission from Burger M, Weber-Rossler T, Willmann M. Measurement of the pregnant cervix by transvaginal sonography: an interobserver study and new standards to improve the interobserver variability. Ultrasound Obstet Gynecol. 1997;9(3):188–193.)
Cervical length is measured on three separate images. The optimal length of examination ranges from 5 to 10 minutes. If the duration of the examination is too short and the patient has dynamic cervical change during the examination, the cervical length may not represent the true length of the cervix. This may account for some observations in which patients seem to gain cervical length over time. The contours of the anterior and posterior lips of the ectocervix are usually clearly defined. For clinical purposes, the shortest cervical length is reported provided that the image is adequate.
When the cervical canal is curved, the cervical length can be determined by tracing along the canal or by adding the sum of two straight sections. To et al.62 concluded from a prospective study conducted in 301 women at 23 weeks of gestation that the question of whether to measure the cervix as a straight line or along the cervical canal might not have any clinical significance because a short cervix (<16 mm) is always straight.
Although cervical examination may appear simple to the experienced sonographer, certain patients may present significant challenges. The presence of a large cervical polyp can affect the identification of the correct cervical plane.63 In addition, a cervix with an unusual orientation may be difficult to find. Therefore, several potential pitfalls should be avoided. These include: (1) excessive probe pressure (falsely long measurement; Fig. 10.3A); (2) short examination time (miss true cervical shortening); (3) recognition of a poorly developed lower uterine segment (avoid falsely long measurement); (4) unequal size and density of the anterior and posterior lips (Fig. 10.3B); and (5) recognition of amniotic fluid “sludge” (Fig. 10.4) (the clinical significance of amniotic fluid “sludge” is reviewed later in this chapter).
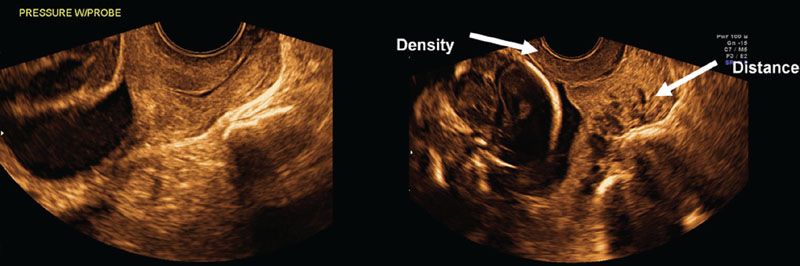
FIGURE 10.3: This transvaginal sonographic image of the cervix demonstrates two pitfalls that can occur when assessing cervical length. A: Excessive probe pressure (can cause the cervical length to appear falsely long). B: Suboptimal image, which displays unequal size and density of the anterior and posterior lips of the cervix. (Reproduced with permission from Hassan SS, Chaiworapongsa T, Vaisbuch E, et al. Sonographic examination of the uterine cervix. In: Fleischer AC, Toy CT, Lee W, et al, eds. Sonography in Obstetrics and Gynecology: Principles and Practice. 7th ed. New York, NY: McGraw-Hill Medical; 2011:816–847.)
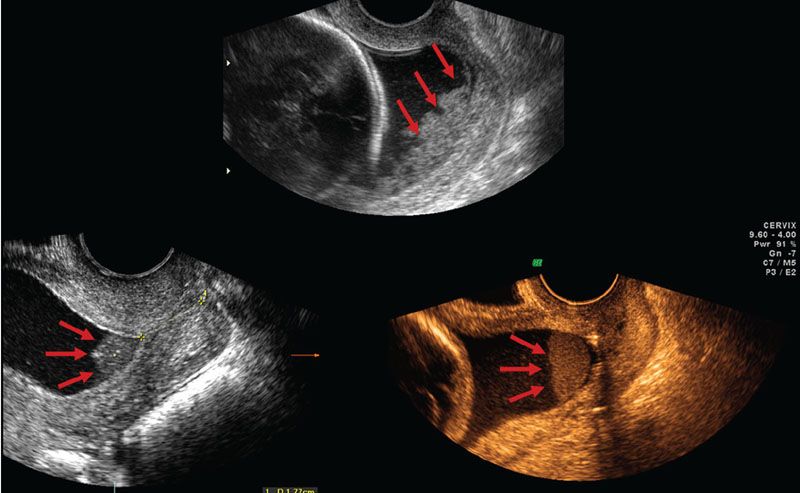
FIGURE 10.4: Transvaginal sonographic images of three patients with short cervices. The arrows illustrate the presence of dense aggregates of particulate matter in close proximity to the internal cervical os, termed amniotic fluid “sludge.” (Reproduced with permission from Hassan SS, Chaiworapongsa T, Vaisbuch E, et al. Sonographic examination of the uterine cervix. In: Fleischer AC, Toy CT, Lee W, et al, eds. Sonography in Obstetrics and Gynecology: Principles and Practice. 7th ed. New York, NY: McGraw-Hill Medical; 2011:816–847.)
Specific recommendations for standardization of each cervical exam within the ultrasound unit can improve the quality of the image acquired (see Fig. 10.2).61 These include obtaining the following criteria on each image of the cervix:
■ Flat internal os or isosceles triangle,
■ Entire length of the cervical canal,
■ Symmetric image of external os, and
■ Equal size and density of the anterior and posterior lips of the cervix.
First Trimester Cervical Sonography for Risk Assessment
The identification of a short cervix, and therefore a patient at risk of preterm birth, early in pregnancy would allow for more timely identification and treatment (if such an intervention is proven) of women destined to have a midtrimester loss prior to the typical midgestation cervical length examination. The accurate measurement of cervical length in the first trimester can be technically difficult as the lower uterine segment may not be distended and can appear to be part of the cervix. Several authors have evaluated the use of first trimester cervical length to predict preterm birth.64–70
Several independent studies concluded that cervical length obtained by first trimester ultrasound does not reliably predict preterm birth.64–67 However, some have described a modified technique to identify the true cervical length and exclude the lower uterine isthmus.68,71 Endocervical length at 11 to 13 weeks was shorter in women who delivered before 34 weeks compared with those who delivered after 34 weeks. The use of sonographic cervical length at 11 to 13 weeks’ gestational age in combination with maternal characteristics such as ethnicity and obstetrical history to predict preterm birth; approximately, 55% of preterm deliveries before 34 weeks could be predicted with a false-positive rate of 10%.68–70
Midtrimester Cervical Sonography for Preterm Birth Risk Assessment
The optimal gestational age to examine the cervix for preterm birth risk assessment is in the midtrimester of pregnancy. The predictive value of cervical length is greater at 19 to 24 weeks when compared with earlier in gestation (i.e., 14 to 24 weeks).17,18,64–70 Furthermore, effective interventions have been demonstrated in trials that have evaluated the uterine cervix at 19 to 25 weeks’ gestation.22–24
PREDICTING PRETERM BIRTH
Cervical length is generally stable in the first 30 weeks of an uncomplicated pregnancy in nulliparous and in multiparous women, and a progressive (although not substantial) shortening of the cervix occurs in the third trimester of pregnancy.15,25,27,72–75 Because transvaginal ultrasound is the most reliable method to assess cervical length, cervical sonography has been used to assess the risk for preterm birth in three groups: (1) asymptomatic low-risk patients; (2) asymptomatic patients with risk factors identifying them as high risk for preterm birth and/or midtrimester loss; and (3) patients presenting with symptoms of preterm labor. This section will highlight some of the studies that have contributed to establishing the value of cervical sonography in the risk assessment for spontaneous preterm birth. Emerging strategies for risk assessment will also be discussed.
Cervical Length for the Prediction of Preterm Delivery
Low-Risk, Asymptomatic Patients
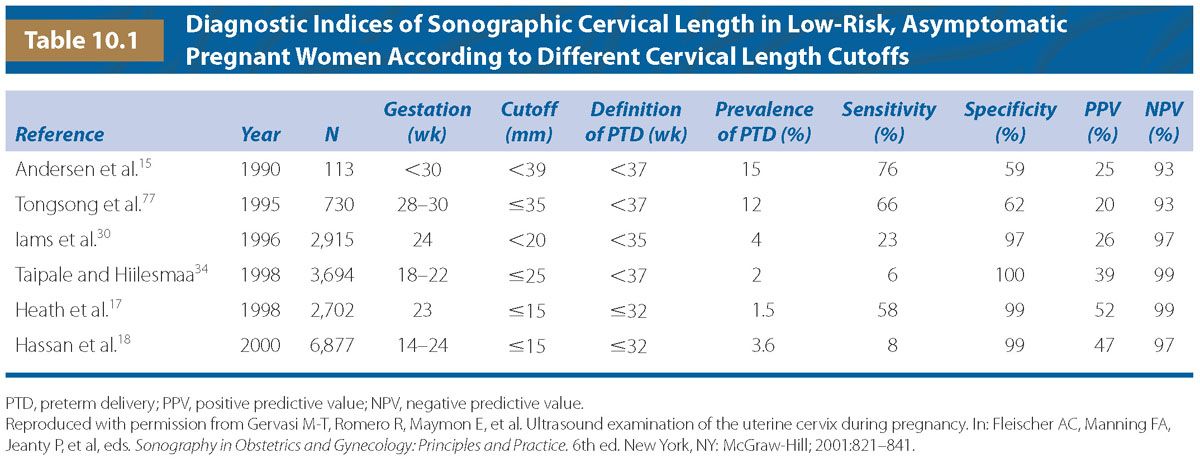
Andersen et al.15 conducted one of the first studies to evaluate the relationship between a sonographic short cervix and the risk of spontaneous preterm birth in a cohort of 113 women who were evaluated by transabdominal and transvaginal sonography, along with manual assessment of the cervix on one occasion before 30 weeks’ gestation. The patient population, with an overall prematurity rate of 15%, was not separated into low-risk and high-risk categories. The authors reported that a cervical length of <39 mm is associated with a 25% risk of preterm delivery, while a long cervix (defined as a cervical length ≥39 mm) decreases the risk of preterm birth (6.7%).15 Furthermore, the risk of spontaneous preterm birth was inversely related to the cervical length. These findings have been confirmed by other investigators, both in low-risk15,17,18,25,27–32,35,37,39,41,75–79 and in high-risk asymptomatic patients.33,36,38,40,60,80–82 Table 10.1 describes the details of some of the studies with adequate information to allow calculation of diagnostic indices and predictive values.
In a prospective cohort study, patients were examined at 24 and 28 weeks of gestation by transvaginal sonography to evaluate the cervix and calculate the risk of delivery prior to 35 weeks.30 There was an exponential increase in the relative risk of delivering <35 weeks as cervical length shortened (Fig. 10.5). This study confirmed the results of Andersen et al.,15 indicating that a short cervix increases the risk for preterm delivery, while the risk is reduced as the cervical length increases.30
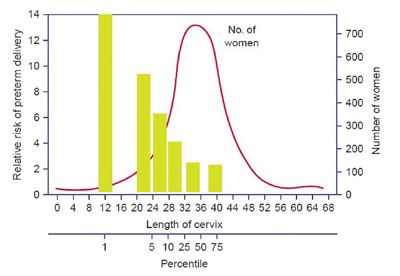
FIGURE 10.5: Distribution of subjects among percentiles for cervical length measured by transvaginal ultrasonography at 24 weeks of gestation (solid line) and relative risk of spontaneous preterm delivery before 35 weeks of gestation according to percentiles for cervical length (bars). (Reproduced with permission from Iams JD, Goldenberg RL, Meis PJ, et al. The length of the cervix and the risk of spontaneous premature delivery. N Engl J Med. 1996;334(9):567–572, copyright © 1996, Massachusetts Medical Society.)
In a population of 2,567 women,17 patients with a history of preterm birth, Afro-Caribbean origin, low maternal age (<20 years), and with low body mass index had a shorter cervix than those without such risk factors. When logistic regression analysis was used to examine the contribution of all these parameters to the prediction of preterm birth (≤32 weeks), a transvaginal sonographic short cervix was the best predictor of outcome.17 Our group evaluated 6,877 women with cervical sonography performed between 14 and 24 weeks. Based on the clinical practice of the ultrasound unit at the time of this study, examinations were initially performed transabdominally and, in cases of cervical length <30 mm or suboptimal visualization, cervical length was evaluated by transvaginal ultrasound.18 (Currently, our unit evaluates the uterine cervix by transvaginal ultrasound); a cervical length of 15 mm or less was associated with preterm delivery at <32 weeks in almost 50% of cases. A history of preterm delivery and African American ethnicity were also associated with the occurrence of spontaneous preterm birth, although the odds ratio was considerably lower than that of a short cervix.18
Thus, several studies have confirmed and extended the observations of Andersen et al.15 in asymptomatic patients at low risk for preterm delivery.15,17,18,25,27,29–32,34–37,39,41,72,77–79,83–85 While the studies evaluating the predictive ability of a short cervix for preterm birth are difficult to compare directly because of differences in study design (i.e., gestational age at cervical length measurement and assessed outcomes), these data have consistently shown that the shorter the cervical length measurement, the higher the risk for preterm birth. Of note, at least one-third of patients who deliver preterm (<32 weeks) will not have a short cervix in the midtrimester; hence, cervical length measurement with ultrasound is not a screening tool but rather a method for risk assessment. The high positive predictive value of a short cervix (nearly 50% for spontaneous preterm birth <32 weeks for cervical length ≤15 mm) has justified trials of intervention (progesterone, cerclage, and pessary to prevent preterm birth).22–24,46–49
High-Risk Singleton Gestations
Several authors have evaluated the utility of cervical length in assessing the risk of preterm birth in women with a history of preterm birth, excisional cervical procedure, known uterine anomaly, or second trimester dilation and evacuation surgery.33,38,72,80,82,86–93
Guzman et al.33 enrolled 469 high-risk patients between 15 and 24 weeks of gestation. High risk was defined as the presence of a history of spontaneous preterm birth before 37 weeks of gestation, prior midtrimester loss, more than two terminations of pregnancy, cone biopsy, uterine malformation, previous cerclage, and exposure to diethylstilbestrol (DES) exposure. Transvaginal cervical sonography and transfundal pressure were performed, and the shortest cervical length, funnel width, funnel length, and cervical index were recorded serially. Cervical length was the best parameter in the prediction of preterm birth in women with prior midtrimester losses.
Owen conducted an observational study that included 183 patients with a history of spontaneous preterm birth before 32 weeks of gestation.38 Patients were enrolled between 16 and 19 weeks of gestation and followed every 2 weeks until 24 weeks of gestation. Forty-eight (26%) women delivered before 35 weeks of gestation. A short cervix (<25 mm) at the first scan was associated with a relative risk of 3.3 (95% CI, 2.1 to 5.0) for spontaneous preterm birth (<35 weeks). The sensitivity, specificity, and positive predictive values were 19%, 98%, and 75%, respectively. After controlling for cervical length, neither funneling nor dynamic shortening were independent predictors of spontaneous preterm birth.
A systematic review of 14 studies evaluating the use of sonographic cervical length to predict preterm birth in patients at high risk for preterm birth demonstrated that patients with a history of spontaneous preterm delivery and a cervical length of <25 mm at <20 weeks had a positive likelihood ratio (LR) of 11.30 (95% CI, 3.59 to 35.57) and at 20 to 24 weeks an LR of 2.86 (95% CI, 2.12 to 3.87), respectively, for delivery at <35 weeks.91
A sonographic short cervix is also predictive of preterm birth in other high-risk populations such as patients with uterine anomalies81 or those with multiple, prior-induced abortions.82
The hypothesis that cervical competence or sufficiency represents a spectrum was studied by Parikh and Mehta,94 who used digital examination of the cervix to assess sufficiency. The authors, however, concluded that degrees of cervical competence did not exist. In contrast, Iams et al.,28 using sonographic examination of the cervix, demonstrated that cervical sufficiency/insufficiency is a continuum. The authors reported a strong relationship between cervical length and previous obstetrical history. This relationship was nearly linear, and patients with a typical history of an “insufficient” cervix did not constitute a separate group from those who delivered preterm.28 Similar results have been reported by Guzman et al.95 Collectively, these studies suggest that there is a relationship between a history of preterm delivery and the cervical length in a subsequent pregnancy. Considering that patients with a short cervix are at increased risk for a midtrimester pregnancy loss (clinically referred to as “cervical insufficiency” by some physicians) or spontaneous preterm delivery with intact or rupture of membranes,15–18,25–30,33,34,36–41,77–80,95 a short cervix can be considered to be the expression of a spectrum of cervical diseases or abnormal function. It is noteworthy that some women with a short cervix have an adverse pregnancy outcome, while others have an uncomplicated term delivery.15,17,25–28,30,33,39,95–98 Indeed, approximately 50% of women with a cervix of 15 mm or less deliver after 32 weeks.17,18 This indicates that cervical length may be only one of the factors determining the degree of cervical strength, and that a short cervix should not be equated with “cervical insufficiency.”
The rate of change in cervical length is associated with spontaneous preterm birth <36 weeks among women with a sonographic short cervix <25 mm.99 Two thousand six hundred ninety-five (2,695) women with a singleton gestation from the general population had a transvaginal cervical length ultrasound performed at 24 weeks (range, 21 to 28 weeks) and a repeat evaluation at 28 weeks (range, 25 to 33 weeks). The change in cervical length (the difference between cervical length at 24 and 28 weeks) was the primary variable of interest. Loss of cervical length between 24 and 28 weeks was represented as a negative value for change in cervical length, while gain in cervical length resulted in a positive value. Calculation of the rate of change was done by dividing the difference in cervical length by the number of days between measurements. The relationships between change in cervical length, average daily change in cervical length, and spontaneous preterm birth <36 weeks were evaluated using logistic regression. The results demonstrate that among women with a sonographic short cervix (<25 mm), change in cervical length between the two visits was significantly associated with a probability of spontaneous preterm birth <36 weeks (odds ratio 0.97; 95% confidence interval, 0.96 to 0.98). In other words, an increase in cervical length between the two visits resulted in decreased risk of spontaneous preterm birth, and conversely, a decrease in cervical length between the two visits resulted in increased risk of spontaneous preterm birth.
Celik et al. proposed the use of an individualized risk assessment for the prediction of preterm birth. The authors conducted a large, prospective observational study of over 58,000 patients.45 Transvaginal sonographic cervical length screening was performed between 20 and 24 6/7 weeks. All patients received routine antenatal care and were given the option to participate in one of two randomized clinical trials of intervention (cerclage or progesterone) if they had a sonographic cervical length of 15 mm or less. Patients who had received the active intervention of either trial were excluded from the risk assessment study. Obstetrical history was subdivided into five groups: (1) primigravida or only pregnancy losses prior to 16 weeks; previous preterm delivery (defined by earliest preterm birth) at (2) 16 to 23 weeks; (3) 24 to 33 weeks; (4) 34 to 36 weeks; or (5) term (>36 weeks). Adjusted odds ratios were calculated for spontaneous delivery at <28 weeks (extreme), 28 to 30 weeks (early), 31 to 33 weeks (moderate), and 34 to 36 weeks (mild) using logistic regression analysis. The authors concluded that cervical length was the best predictor of spontaneous preterm birth. The risk estimation was improved by the addition of obstetric history, but not any maternal characteristics or other interactions. This important study includes tables that provide LRs to allow for the risk assessment of spontaneous preterm birth. The detection rates of extreme, early, moderate, and mild spontaneous preterm birth, by combining the obstetric history and cervical length, were 80.6%, 58.5%, 53.0%, and 28.6%, respectively, with a 10% screen-positive rate.45 This model provides for a higher detection rate than obstetric history or cervical length alone, and allows for population-based screening, which in a setting of potential effective interventions, may have great value.
Repeat Sonographic Evaluation of Cervix
Carvalho et al.65 evaluated the utility of serial cervical length measurements obtained at 11 to 14, and at 22 to 24 weeks of gestation in an unselected group of pregnant women. The authors found that cervical length at 11 to 14 weeks was not significantly different between women who delivered preterm and term, but that the cervical length assessments obtained in the second trimester were predictive of preterm delivery; the shortening between the first and the second exam was more pronounced in the group that delivered preterm. Ozdemir et al.100 subsequently confirmed the observation of a more rapid cervical change between the first and the second trimesters in women destined to deliver preterm.
Several other groups have evaluated repeated measurements in the second trimester and the rate of change in cervical length associated with the risk of preterm birth in high- and low-risk patients.33,99,101–105 Cervical Length was measured serially in high-risk women between 15 and 24 weeks’ gestation. The rate of change in women who did not develop cervical insufficiency was nonsignificant, while those women destined to develop a cervix <2 cm in length, defined as “insufficient,” had a significant rate of cervical length change of −0.52 cm per week.33 Serial evaluation of cervical length in women who were found to have a short cervix between 1 and 25 mm on an initial scan between 16 and 28 weeks,102 demonstrated that the women whose cervix underwent further shortening on the second measurement delivered at an earlier gestational age (36 + 4 vs. 38 + 2 weeks, P = .031). These data collectively indicate that cervical shortening is a part of the activation of the parturition process. This shortening occurs as a continuum, and subsequent cervical length measurements in women at risk may help to differentiate those with a short cervix who will deliver at term, and those who will have a preterm delivery. Moroz and Simhan99 evaluated the difference in cervical length between 24 and 28 weeks in a cohort of women from the general obstetric population. Within the group of women with an initial cervical length <25 mm, additional shortening was associated with an increased risk of preterm birth. The authors also suggest a lower risk of preterm birth in women with an initially identified short cervix if the cervix remained stable or increased in length. As the interval for repeat exam reported in the literature varies from 1 to 8 weeks,102 the optimal timing of a repeat measurement and how clinical management should be adjusted is yet to be determined.
In practice, most algorithms for the management of patients at risk for preterm birth include serial ultrasound evaluation of the uterine cervix; however, there is no consensus on the time interval between measurements, patient population requiring serial ultrasound evaluation, and whether serial evaluations improve pregnancy outcomes.
Cervical Length in Multiple Gestations
Twin Pregnancies
Twin gestations occur in 1% of all pregnancies and are at increased risk of preterm birth. Several studies have examined the value of transvaginal sonography for the prediction of preterm delivery in twin pregnancies, and reported an increased risk for preterm birth in patients with a sonographic short cervix.106–121
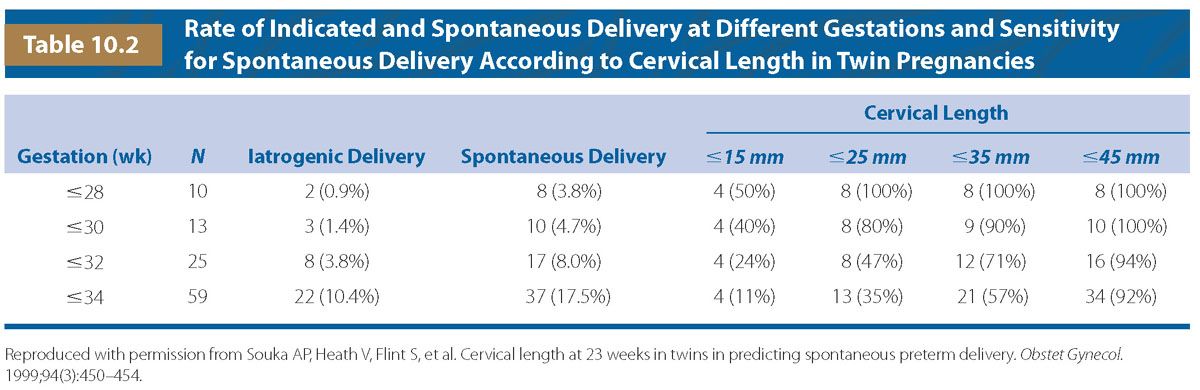
The sensitivity of a short cervix defined as a length of 25 mm or less at 23 weeks’ gestation in the prediction of spontaneous preterm delivery at 28, 30, 32, and 34 weeks is 100%, 80%, 47%, and 35%, respectively (Table 10.2).111 The rate of spontaneous delivery at or before 32 weeks increases exponentially with decreasing cervical length measured at 23 weeks. The risk of preterm delivery for patients with a cervical length of 25 mm or less in twin pregnancies is similar to the risk in singleton pregnancies with a cervical length of 15 mm or less (52%).17,18 Thus, the cervical length required in twin gestations to provide assurance against the occurrence of preterm delivery is greater than that of singleton gestations. Furthermore, ninety-seven percent of twin gestations with a cervical length of 35 mm or more deliver after 34 weeks of gestation.110
The median cervical length for twins at 23 weeks’ gestation is similar to singletons (36 mm).114 However, a greater proportion of twin pregnancies have a cervical length of 25 mm or less (12.9%114) when compared with singletons (8.4%122). The same holds true for patients with a cervical length of 15 mm or less (4.5% in twins114 vs. 1.5% in singletons122).
Fox et al. reported the utility of a repeat cervical exam 2 to 6 weeks after obtaining a baseline exam at 18 to 24 weeks. Among twin pregnancies in which the cervical length decreased by 20% or more, there was an increased risk of preterm birth, even in the setting of a normal cervical length (36.8% rate of preterm birth at <34 weeks vs. 12.9% with stable exam, P = .018).123
Conde-Agudelo et al. performed a systematic review and meta-analysis of the predictive test accuracy for cervical length in asymptomatic twin pregnancies. Among asymptomatic women, a cervical length ≤20 mm at 20 to 24 weeks’ gestation had a pooled positive LR of 10.1 and a negative LR of 0.64 to predict preterm birth <32 weeks. A cervical length ≤25 mm at 20 to 24 weeks’ gestation had a pooled positive LR of 9.6 to predict preterm birth <28 weeks of gestation.124
Sonographic cervical length is predictive of preterm birth in twin gestations in acute preterm labor and can predict those who will deliver within 7 days from those who will not.118 In a study of 87 twin pregnancies presenting in preterm labor, 80% (4 of 5) of patients with a cervical length of 1 to 5 mm delivered within 7 days, in contrast to 0% (0 of 21) of patients with a cervical length of >25 mm.118 A cutoff of 25 mm (≤25) has been proposed for the risk assessment of preterm birth in twin pregnancies.118,120
The utility of preoperative sonographic cervical length in predicting preterm birth in 137 cases of twin-to-twin transfusion syndrome (TTTS) undergoing laser coagulation of placental anastomoses before 26 weeks’ gestation has been examined.119 The risk of delivery prior to 34 weeks was 74% in patients with a cervical length <30 mm. In addition, logistic regression analysis identified cervical length <30 mm (OR 3.53 [1.55 to 8.03]) and being multiparous (OR 2.27 [1.09 to 4.74]) as independent risk factors for preterm birth at <34 weeks.119
Triplet Pregnancies
Cervical length is also predictive of preterm delivery in triplet gestations.125–127 The sensitivity, specificity, positive predictive value, and negative predictive value of a short cervical length measured between 21 and 24 weeks and between 25 and 28 weeks are 86%, 79%, 40%, 97%, and 100%, 57%, 18%, 100%, respectively. A short cervix identifies triplet pregnancies at risk for preterm birth and, for an equal cervical length measurement in a singleton pregnancy; the risk of preterm delivery in a triplet pregnancy is higher.125–127 The identification of patients at risk of preterm birth with triplet gestations may be improved with the combination of cervical length assessment and fetal fibronectin (fFN) testing. In a retrospective study, Fox et al.,128 evaluated the combination of fFN and cervical length as predictors of preterm birth in triplet pregnancies. A historical cohort of 39 consecutive women with triplet pregnancies managed in one maternal–fetal medicine practice from 2005 to 2011 were included into the analysis for this study. A positive fFN was significantly associated with spontaneous preterm birth <28, <30, <32, and <34 weeks, while a sonographic short cervix was significantly associated with spontaneous preterm birth <32 weeks gestation. Combined screening of fFN and cervical length assessment in asymptomatic triple pregnancy and positive results in both tests were associated with the highest likelihood of spontaneous preterm birth at all gestational ages. For example, a positive fFN with a short cervix had a sensitivity of 62.5%, specificity of 90%, positive predictive value of 62.5%, and negative predictive value of 90% for the prediction of spontaneous preterm birth <32 weeks’ gestation. The authors suggest that the combination of fFN and cervical length assessment in the screening of asymptomatic triplet pregnancies for the prediction of spontaneous preterm birth is useful.
Cervical Examination in Patients Presenting with Preterm Labor
Forty-seven percent (47%) of women presenting in preterm labor who are treated with a placebo deliver at term.129 Differentiating those patients who are in true preterm labor is often a challenge.
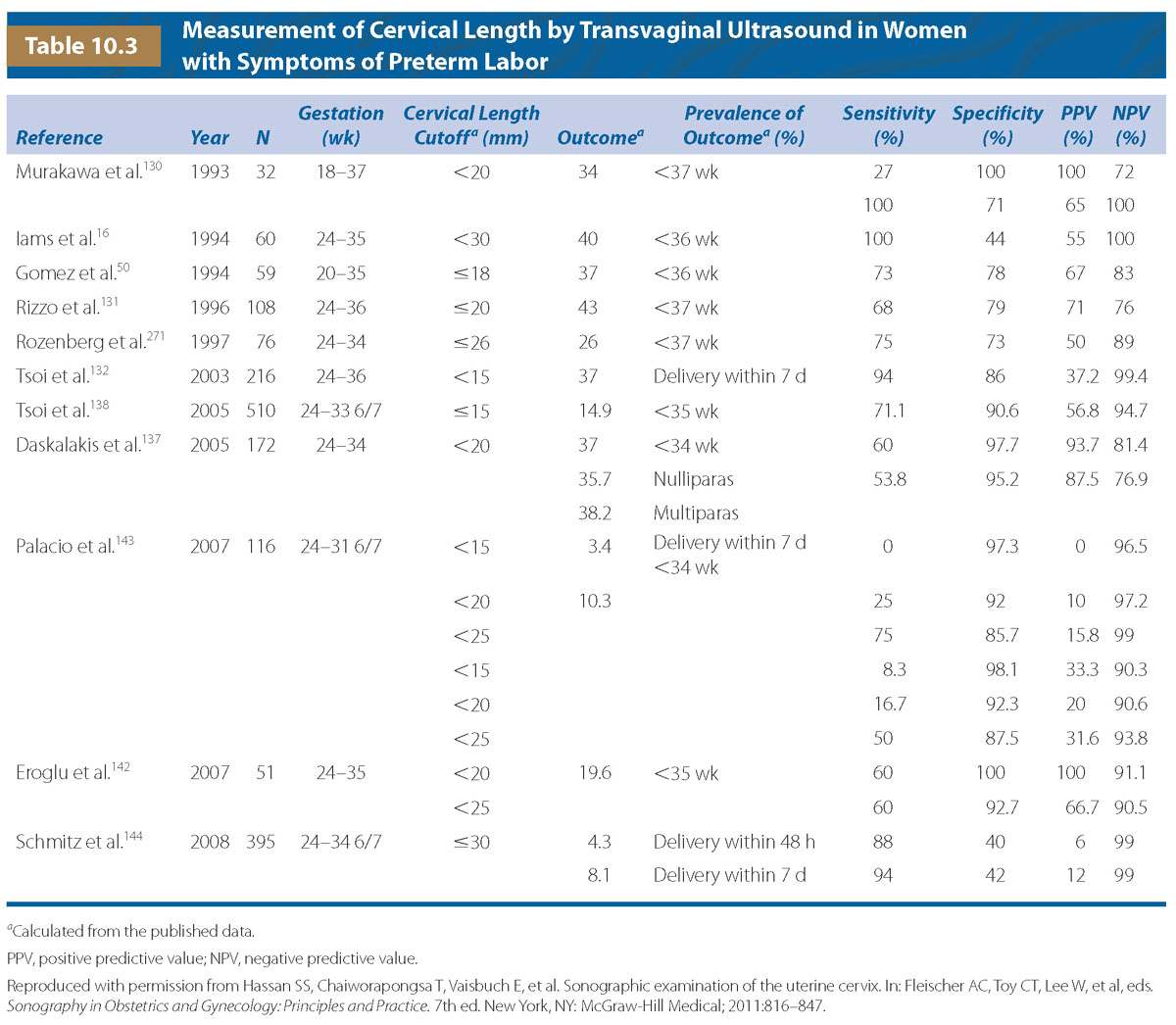
Sonographic examination of the cervix in patients presenting with preterm labor can assist in the risk assessment for preterm delivery. In a study of 60 singleton and twin pregnancies presenting with preterm labor, all patients with a cervix >30 mm delivered at term.16 The high negative predictive value for preterm birth associated with a long cervix provides important clinical information in symptomatic patients.16,50,130–144
The observation that a sonographic short cervix is a powerful predictor of preterm birth in patients presenting with symptoms of preterm labor has been confirmed and extended in several other studies. Gomez et al.145 reported the use of sonographic cervical length and fFN test to predict spontaneous preterm delivery within 48 hours, 7 days, and 14 days of admission as well as delivery at <32 weeks and <35 weeks of gestation. A cervical length of <15 mm was the most powerful predictor of preterm birth within 48 hours (OR 9.7, P < .05). Both cervical length and fFN were predictive of preterm birth within 7 and 14 days. When fFN test results were added to a cervical length cutoff of <30 mm, there was significant improvement in the prediction of preterm delivery.145
A systematic review of seven studies evaluating the use of transvaginal ultrasound and cervical dilation in patients in preterm labor was conducted by Leitich et al.146 The authors subdivided patients into three groups: (1) patients with preterm labor, and (2) low-risk asymptomatic patients with early (20 to 24 weeks) or (3) late (27 to 32 weeks) sonographic cervical length. The optimal cutoff values for cervical length in patients in preterm labor ranged between 18 and 30 mm, with sensitivity between 68% and 100%, and specificity was between 44% and 79%.146 Several studies have demonstrated that the use of sonographic cervical length in labor and delivery can improve the management of patients in preterm labor by decreasing the number of unnecessary interventions. In addition, by applying specific management schemes that utilize a cervical length cutoff, hospital stay and health care costs have been reduced.135,138,139,142,143,145,147–150 The utility of hospitalization in patients with a short cervix151 or repeat sonographic evaluation of the cervix after the completion of tocolysis has been questioned.152
A randomized controlled trial141 was conducted in 41 women with threatened preterm labor. Patients underwent a sonographic evaluation of the cervix or received the planned treatment (tocolytics and steroids). Treatment was withheld among patients in the ultrasound group with cervical length >15 mm. A higher proportion of patients in the control group received steroid treatment despite remaining undelivered for more than a week when compared with those in the ultrasound group (90% [18 of 20] vs. 14% [3 of 21], RR 0.16; 95% CI, 0.05 to 0.39). In addition, there was a significant difference in the duration of hospital stay between the two groups (median [range]; 0 hours [0 to 24] in the ultrasound group vs. 24 hours [0 to 67], P < .0001).141 Larger studies are needed to assess the impact of the use of this management scheme on neonatal outcome.
Table 10.3 summarizes the results of some of the studies published to date that evaluated the use of sonographic cervical length in patients presenting with preterm labor. Although the studies have utilized different cervical length cutoffs, gestational age, and populations, there is agreement that the shorter the cervix, the higher the risk for preterm delivery.
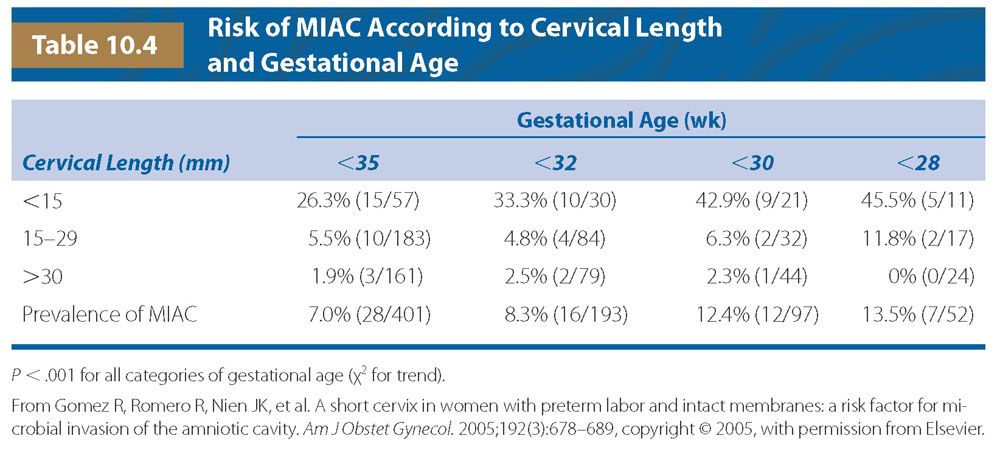
Patients with preterm labor and a short cervix are also at an increased risk for intrauterine infection/inflammation. Gomez et al.153 conducted a study in 401 patients presenting with preterm labor and cervical dilation of <3 cm (as assessed by digital examination). All patients underwent amniocentesis. The prevalence of microbial invasion of the amniotic cavity (MIAC) was 7% (28 of 401). Patients with a short cervix (<15 mm) had a higher rate of MIAC and preterm delivery at <35 weeks compared with those with a long cervix. (MIAC: short cervix, 26.3% [15 of 57] vs. long cervix 3.8% [13 of 344], P < .05; and for preterm delivery <35 weeks: short cervix, 66.7% [38 of 57] vs. long cervix, 13.5% [44 of 327], P < .01.) Furthermore, the rate of infection was higher in patients presenting at 30 weeks or less with a cervical length <15 mm when compared with those 15 mm or greater (43% [9 of 21] vs. 3.9% [3 of 76], P < .05). The authors provided an estimated risk of MIAC in patients in preterm labor according to gestational age and cervical length (Table 10.4).
In summary, cervical sonography is a powerful method to assess the risk of preterm delivery in patients presenting with preterm labor. Clinicians and patients can be reassured with the finding of a long cervix and avoid unnecessary intervention. Patients in preterm labor who are diagnosed with a short cervix are at increased risk for intrauterine infection/inflammation as well as a higher rate of preterm delivery, and thus may benefit from targeted interventions (i.e., antibiotic and/or steroid administration and transfer to a center with a neonatal intensive care unit). Further investigation into the most efficacious algorithm of management for these patients is still needed.
Cervical Length and Fetal Fibronectin for the Prediction of Preterm Birth
Fetal fibronectin in cervicovaginal fluid has been used in conjunction with sonographic cervical length measurement to identify patients at risk for preterm delivery.
A systematic review demonstrated improved accuracy of the combination of fFN with ultrasound assessment of cervical length as screening tools for preterm labor and preterm birth prediction compared with the traditional clinical method of digital cervical examination.154 The authors demonstrated that classic clinical criteria correctly identified 30.2% of women presenting with symptoms of preterm labor and delivered preterm at <37 weeks of gestation. The combination of fFN and ultrasound assessment of cervical length had a modest positive predictive value for preterm birth <37 weeks of 49.4%; however, this was higher than that of clinical diagnostic criteria alone. The diagnostic accuracy of the combination of fFN with sonographic cervical length assessment was significantly higher when predicting preterm birth risk within short periods of time (<7 days) and at earlier gestational ages (<28 weeks). For example, the sensitivity for delivery <7days with the combination method was 71.4%, with negative predictive value of 98.9%. Thus, the combined screening approach of sonographic cervical length assessment with fFN sampling may be useful for predicting short-term risks and may be used to guide acute management of patients presenting with symptoms of preterm labor.
Emerging Imaging Modalities to Evaluate the Cervix
Although cervical length is the most powerful predictor of preterm birth, there is a need to determine if the degree of cervical softening can be evaluated. Emerging imaging modalities seek to evaluate these changes in the cervix in a more objective fashion than the subjective digital assessment of cervical “softness or firmness.”
Elastography
Ultrasound-derived elastography evaluates tissue strain or stiffness of tissue by assessing the displacement of moving tissues when pressure is applied.155,156 Specialized software produces a color code to express softness and stiffness (Fig. 10.6). Strain can also be expressed numerically as a percentage of tissue displaced when pressure is applied within a region of interest.157
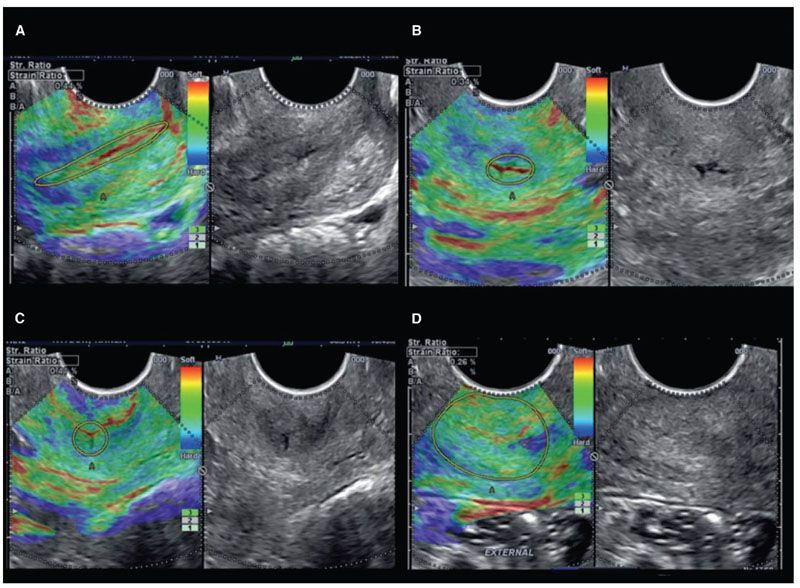
FIGURE 10.6: Cervical strain calculation performed in: A. endocervical canal in a sagittal plane; B. endocervical canal in a cross-sectional plane at the level of the internal os; C. endocervical canal in a cross-sectional plane at the level of the external cervical os; and D. complete cervix in a cross-sectional plane at the level of the external cervical os. (Reproduced with permission from Hernandez-Andrade E, Hassan SS, Ahn H, et al. Evaluation of cervical stiffness during pregnancy using semiquantitative ultrasound elastography. Ultrasound Obstet Gynecol. 2013;41(2):152–161.)
Molina et al.158 reported a reproducibility study that assessed agreement in ultrasound-elastography assessment of the cervix at a gestational age range of 12 and 40 weeks. The reported intraclass correlation coefficients between 0.16 and 0.8 for different regions of interest within the cervix but concluded that with the exception of the external, superior portion of the cervix, the measurements were reproducible. Of note, the authors suggested that although the part of the cervix nearest to the probe appeared to be the most soft, the measurement may merely be a reflection of the pressure applied by the transducer.
Elastography has been used to evaluate cervical stiffness in a cohort of 262 women with 1,557 strain estimations between 8 and 40 weeks’ gestational age.159 Using regions-of-interest at preselected anatomic locations within the cervix, the endocervical canal strain was on average 33% greater (softer) than that obtained for the entire cervix. Cervical tissue strain was greater for multiparous women than for nulliparous women, and was greater among women with a cervical length between 25 and 30 mm compared with those having cervical lengths >30 mm. Overall, a continuous reduction in cervical stiffness with decreasing cervical length and advancing gestational age was seen; which is in keeping with the known physiologic remodeling changes in the cervix during pregnancy.
Ultrasound-derived cervical elastography may have utility in the identification of women with cervical ripening who do not have a short cervix but are destined to deliver preterm, or in a complementary way to cervical length assessment. However, the use of elastography in clinical practice is not routine. Future research is needed to confirm that the changes in strain correlate with changes in cervical remodeling and to evaluate the best use of this technology in the risk assessment for preterm birth.
Acoustic Attenuation
Cervical tissue hydration increases as a function of cervical ripening and advancing gestational age.1–4,160 The loss of energy as an ultrasonic wave propagates through tissue, acoustic attenuation, has been noted to be related to tissue stiffness, collagen concentration, and water concentration.161 Forty women underwent transvaginal ultrasound using a system that allowed access to radiofrequency image data. Radiofrequency data were analyzed using an attenuation coefficient derived from a tissue phantom. Regression analysis revealed that attenuation of the cervix was predictive of the exam-to-delivery interval (β = .43, P = .011) but not predictive of gestational age at the time of the exam (β = −.23, P = .15) or cervical length (β = .077, P = .65). Interestingly, two women in the study had a short cervical length in the midtrimester but moderate or high attenuation values (un-ripe cervix). Both of these women delivered at >34 weeks and remained pregnant for at least 11 weeks after the cervical length measurement. However, a limitation of this technique is the high variation in attenuation values between subjects and operator chosen regions-of-interest for evaluation. Furthermore, cervical tissue is nonhomogeneous, which may limit the application of an attenuation algorithm, which relies on tissue homogeneity.162
CAUSES OF A SONOGRAPHIC SHORT CERVIX
A short cervix often occurs when there is cervical ripening; however, not all short cervices are ripe, hence the observation that some women with a short cervix deliver at term. We have proposed that a short cervix is syndromic in nature and can be caused by multiple etiologies,14,163–165 such as (1) the loss of connective tissue after a cervical operation such as conization166
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree