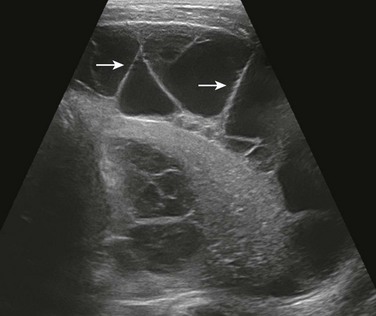
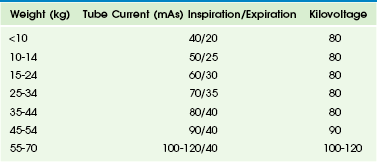
Chapter 49 Conventional radiography is the creation of a projection image with the use of x-rays to view parts of the human body. This primary, cost-effective imaging method currently is the modality used most frequently and widely in clinical practice for evaluation of the respiratory system in pediatric patients. Conventional radiography is associated with a very low level of ionizing radiation exposure (in the range of 0.01 to 0.02 mSv for chest posteroanterior [PA] radiography).1,2 Soft tissue neck study and chest radiography, the two conventional radiographic imaging techniques used most frequently to assess the pediatric respiratory system, are discussed in the following sections. Inspiratory stridor resulting from an upper airway obstruction is the most frequent indication of a soft tissue neck study in pediatric patients.3 The common causes of inspiratory stridor include croup, epiglottitis, a foreign body, and an upper airway mass in infants and children. To obtain optimal diagnostic quality, the neck of the patient should be extended and images should be obtained at full inspiration. The standard soft tissue neck radiographic views consist of both an anteroposterior (AP) view and a lateral view. An additional expiratory lateral view of the neck subsequently may be obtained for assessment of subglottic stenosis, which can be beneficial in differentiating a fixed large airway disorder (e.g., subglottic stenosis) from a dynamic large airway disorder (e.g., tracheomalacia). Chest radiography is the imaging study obtained most frequently to evaluate the respiratory system in pediatric patients. Immobilization is usually required in uncooperative infants and young children (<5 years) to achieve consistent image quality by decreasing motion artifacts and position deviations.4 Chest radiography is obtained during quiet inspiration in uncooperative infants and young children and during full inspiration in cooperative older pediatric patients. The standard chest radiographic views consist of the AP view in infants and young children (<5 years) and both the AP and PA views in older children, in addition to a lateral view. AP, PA, and lateral views of the chest can be obtained with the patient in the supine or erect position. Exposure parameters of the chest radiography should be appropriately optimized. However, unnecessary radiation to nonthoracic structures such as the lower neck, proximal upper extremity, and upper abdomen should be avoided by using appropriate collimation and shielding.5,6 In contrast to a radiographic screen-film system, image acquisition and display are decoupled in digital radiography, which allows increased versatility of image manipulations.7,8 One of the most commonly used image processing techniques in digital chest radiography is unsharp mask filtering or edge enhancement, which facilitates the detection of thoracic fine linear abnormalities or structures such as pneumothorax, vascular catheters, and the interlobar fissures, even in newborns.9 Recently, optimization of digital radiographic techniques has been emphasized to reduce potentially unnecessary overexposure to pediatric patients.6,10 The increased likelihood of overexposure in digital radiography, the so-called dose creep, is attributed not only to the lack of a standardized exposure index but also to the difficulty in recognizing overexposed radiographs by radiologic technologists and radiologists. Fortunately, a new standardized exposure index for digital radiography was proposed recently.11 Optimized techniques of digital chest radiography in children often are different from those in adults. For instance, automatic exposure control and grids are not particularly helpful in small pediatric patients. Additional views such as expiratory, decubitus, and oblique views sometimes are necessary to clarify abnormalities detected on standard AP or PA views or to solve unanswered clinical questions. Expiratory views may be used to confirm air trapping due to an underlying airway obstruction. The lateral decubitus view generally is used to detect freely shifting pleural effusion or air; it is used infrequently to demonstrate an air-fluid level in an intraparenchymal cavitary lesion. In addition, the lateral decubitus view may be used to demonstrate air trapping in the dependent lung or to clarify poorly defined lung opacities in the nondependent lung in uncooperative infants and young children.12,13 Oblique views may be helpful for evaluating rib, soft tissue, hilar, carinal, and peripheral lung abnormalities. Fluoroscopy can be used to evaluate dynamic large airway and lung abnormalities, such as airway obstruction, air trapping, and diaphragmatic palsy/paralysis. Use of fluoroscopic techniques and equipment should be optimized to minimize exposure of both pediatric patients and operators to harmful ionizing radiation by following the “imaging gently” and “step lightly” principles.14 A fluoroscopy-guided airway study may be helpful in demonstrating dynamic airway abnormalities, such as laryngomalacia, tracheomalacia, obstructive sleep apnea, and vocal cord dysfunction syndrome.15–17 Additionally, a fixed airway disorder such as stenosis or stricture also can be identified and differentiated from a dynamic airway disorder. Compared with endoscopic procedures for evaluating large airways, a fluoroscopy-guided airway study generally is inexpensive and less invasive.18 In recent years, the diagnostic role of the fluoroscopy-guided airway study has begun to be replaced by dynamic airway CT with a low radiation dose technique.19 Dynamic airway CT is more accurate than a fluoroscopy-guided airway study for evaluation of the location, degree, and extent of both the dynamic and fixed airway abnormalities. Furthermore, dynamic airway CT can provide additional information about other intrathoracic structures, which is a valuable benefit.19 Ultrasound is a valuable and widely used imaging modality for evaluating the lungs and pleura, particularly in pediatric patients, because it is widely available, relatively easy to perform, and does not expose patients to radiation.20,21 Its real-time evaluation capability and portability are important additional benefits. Furthermore, crucial information regarding associated vascular structures or underlying blood flow also can be obtained with color Doppler ultrasound.20,21 Although chest radiography or CT is the main imaging modality of choice for evaluating the lungs and pleura, the complementary use of ultrasound may provide clinically relevant information in patients with certain conditions.20,21 The main clinical indication for ultrasound of the lungs in pediatric patients is to characterize a peripheral lung opacity (i.e., parenchymal versus pleural disease) that has been detected with chest radiography.20 Frequent underlying etiologies include atelectasis, consolidation, lung necrosis, a lung abscess, congenital lung lesions, and a primary or metastatic lung neoplasm (Fig. 49-1).20,21 For evaluation of these abnormalities, conventional chest radiography should be carefully reviewed to localize the area of interest so the clinical question can be specifically answered with the ultrasound evaluation.20,21 Ultrasound evaluation of the lungs typically is performed with the patient in the supine or upright position. However, to improve the visualization in some selected situations, the lateral decubitus view or the supraclavicular and/or suprasternal notch view may be beneficial. Optimal views can be achieved by placing a pillow or blanket on the dependent side or behind the shoulder to help extend the neck of the patient.20 Figure 49-1 Plain radiography and ultrasound in a 3-year-old girl with fever, cough, and respiratory distress. The choice of ultrasound transducer depends primarily on three factors: the age of the patient, the size of the patient, and the location of the abnormality.20,21 Although curved or linear array transducers typically are used to evaluate peripheral lung opacity, transducers that are smaller in size, such as sector or vector transducers, may be necessary for imaging in infants or young children who have a small available acoustic window (such as between the ribs). High-frequency transducers (e.g., 7.5 to 15.0 MHz) are helpful in evaluating the chest in infants and young children who do not have a substantial amount of subcutaneous fat because they provide higher resolution ultrasound images with a limited ability for soft-tissue penetration.20 Conversely, use of low-frequency transducers (e.g., <5 MHz) may be necessary when evaluating older children who have a large amount of subcutaneous fat because these transducers provide better soft tissue penetration, although the ultrasound image resolution is decreased.20 Color Doppler ultrasound is useful for evaluating lung lesions with underlying vascular structures in cases of pulmonary sequestration or blood flow in cases involving a neoplasm. Ultrasound can be useful in differentiating pleural fluid from atelectasis and/or consolidation when the diagnosis is equivocal on the basis of conventional radiography. Furthermore, ultrasound is more sensitive and accurate than conventional radiography or CT for characterizing pleural fluid, which may be simple or complex (Fig. 49-2).20 Ultrasound evaluation of patients in both the erect and lateral decubitus positions can be useful for differentiating between freely flowing and loculated pleural fluid. In addition, ultrasound can visualize the internal debris, septations, and pleural thickening often associated with parapneumonic collections. Such complex pleural effusion often requires a drainage procedure that can be facilitated with the guidance of ultrasound. CT is a valuable cross-sectional imaging study for evaluating pediatric airways and lungs, mainly because its images provide excellent air-tissue contrast. The development of multidetector CT (MDCT), which can provide a short scan time with a decreased rate of sedation, has increased the role of CT in the assessment of pediatric airways and lungs.22 Respiratory motion artifacts often degrade CT image quality in infants and young children who breathe freely during the scan. These artifacts can be reduced with the use of general anesthesia, and controlled ventilation.23,24 These techniques also can be used to control either the inspiratory or expiratory phases of respiration.23–25 In addition, recently introduced high-pitch dual-source spiral CT scanning is very helpful in reducing motion artifacts on chest CT scans of children who breathe freely during the procedure.26 Reducing the CT radiation dose while maintaining diagnostic image quality is of critical importance in pediatric patients because of the greater radiosensitivity and longer life expectancy of children, coupled with increasing CT use. Low-dose, body size–adapted chest CT protocols using variable tube voltages and tube currents have been established, usually on the basis of body weight.27,28 However, several recent studies have demonstrated that cross-sectional dimensions provide better CT dose adaptation to body habitus.29–31 A practical pediatric chest CT protocol based on a volume CT dose index individually determined by cross-sectional area and mean density of the body recently was developed for daily clinical use.32 The tube current always should be modulated if applicable because this modulation allows the CT dose to be reduced substantially without degrading image quality.33–35 Electrocardiogram-triggered sequential scanning may be used in CT of the chest in children to achieve fewer motion artifacts and a lower radiation dose.24,36 The image quality of CT of the chest in children may be further improved by adjusting kilovolt levels and reconstruction algorithms as follows: a low kilovolt level for enhanced CT and a high kilovolt level for unenhanced CT, a high-frequency reconstruction algorithm for lung evaluation, and a standard reconstruction algorithm for mediastinal evaluation. In addition to axial CT images, postprocessed and reconstructed images such as multiplanar reformatted (MPR) and three-dimensional (3D) images considerably increase diagnostic accuracy of pediatric chest CT (Fig. 49-3).37 CT scanning with thinner collimation (<1 mm) offers better quality MPR and 3D images. Various visualization techniques including maximum intensity projection, minimum intensity projection, volume rendering, and virtual bronchoscopy can help further visualize thoracic abnormalities (see Fig. 49-3). Figure 49-3 Multiplanar reformatted and three-dimensional (3D) computed tomography (CT) imaging. Anatomic details of the pediatric airways can be imaged with CT.38,39 However, small airways distal to the subsegmental level (i.e., airways <0.5 to 1.5 mm in diameter) often are invisible on CT because of their size. CT is less invasive than bronchoscopy in evaluating pediatric airways and provides cross-sectional imaging without superimposition. Various airway abnormalities, including fixed or dynamic obstruction, bronchiectasis, and wall thickening, can be diagnosed with CT. MRI may be used to evaluate large airways with comparable diagnostic accuracy, but MRI is clearly inferior to CT in evaluating small airways because of lower spatial resolution and a lower signal/noise ratio. A static airway CT study is performed mainly to assess a fixed airway narrowing or stenosis. Axial CT data are acquired in infants and young children while they breathe freely and in older children while they hold their breath at the end of an inspiration (Fig. 49-3, C). Anatomic details of the airway typically are well visualized, even in free-breathing studies, because of the fast scan speed of MDCT (>16 row MDCT). The extent and cause of airway abnormalities can be better evaluated with MPR and 3D CT images than with axial CT images alone. A paired inspiratory and expiratory CT study is performed primarily for the dynamic evaluation of a large airway disorder, most commonly tracheobronchomalacia.19 Expiratory CT is performed with the low radiation dose technique to minimize the dose delivered during this dual-phase study (Table 49-1). The resultant effective dose from this paired study typically is in the range of 3.5 to 7.5 mSv.19 Expiratory CT can be obtained with two different respiratory maneuvers: (1) holding the breath at the end of an expiration during end-expiratory CT and (2) forced exhalation during dynamic expiratory CT. In uncooperative infants and young children, general anesthesia with intubation, controlled ventilation, or respiratory triggering can be used.19,23,24,39 Table 49-1 Tube Current and Kilovoltage by Patient Weight for Central Airway Multidetector Computed Tomography From Lee EY, Boiselle PM. Tracheobronchomalacia in infants and children: multidetector CT evaluation, Radiology. 2009;252(1):7-22. In cine airway CT, axial sequential scans are acquired continuously at predefined noncontiguous slices with high resolution and use of the low radiation dose technique throughout the respiratory cycle.40 This technique allows changes in the cross-sectional area and shape of the airway to be demonstrated throughout the entire respiratory cycle, thus making the diagnosis of tracheobronchomalacia possible. To achieve the high temporal resolution required for cine airway CT, the fastest gantry rotation speed is used. The total scan time should be tailored to a range of one to two respiratory cycles to minimize the radiation dose. As a result, the radiation dose of cine airway CT is quite low—in the range of 0.2 mSv to 0.3 mSv.24 Cine airway CT is performed in infants and young children as they breathe freely or with a coughing maneuver in cooperative older children.19,41 Coughing exaggerates the expiratory collapse of the airway because it elicits a higher intrathoracic extra-airway pressure than does normal or forced exhalation, and thus it is the preferred technique for a cine airway CT study. In addition to dynamic airway evaluation, cine airway CT also can be used to detect trapping of air in the lung, which often is a secondary sign of underlying small airway disease.40 Increased longitudinal coverage (e.g., 4 cm for 64-section CT and 16 cm for 320-section CT) of modern MDCT makes a four-dimensional (4D) airway CT study feasible.42
Imaging Techniques
Conventional Radiography
Soft Tissue Neck Study
Chest Radiography
Fluoroscopy
Fluoroscopy-Guided Airway Study
Ultrasound
Evaluation of Lungs
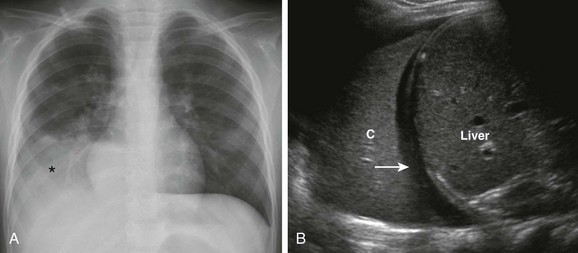
A, Frontal chest radiograph shows an opacity (asterisk) projecting over the right lower lung zone. B, Longitudinal ultrasound view of the right hemithorax demonstrates a consolidated lung (C), small effusion (arrow), and liver.
Evaluation of Pleura
Computed Tomography
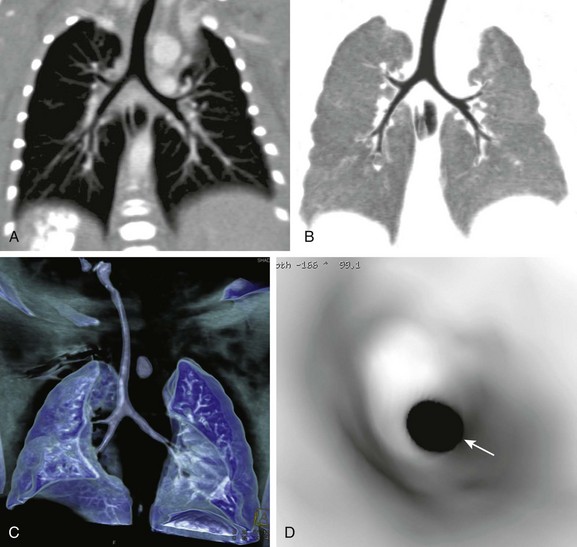
A, A coronal thin-slab CT image shows normal relationships between the airway and the pulmonary artery, indicating the thoracic situs solitus. B, A coronal minimum-intensity projection CT image shows anatomic details of the central airways. C, A volume-rendered CT image shows the 3D appearance of the lungs and airways. D, A virtual bronchoscopic image providing an endoscopic view of the trachea shows a concentric narrowing (arrow) from a tracheal web.
Evaluation of Airways
Static Airway CT Study
Dynamic Airway Computed Tomographic Study
Cine Airway Computed Tomographic Study
Four-Dimensional Airway Computed Tomographic Study
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Imaging Techniques