© Springer International Publishing Switerzland 2016
Carsten Nieder and Johannes Langendijk (eds.)Re-Irradiation: New FrontiersMedical Radiology10.1007/174_2016_76Re-irradiation in Head and Neck Cancer
(1)
Department of Radiation Oncology, University Medical Center Groningen, University of Groningen, Groningen, The Netherlands
Abstract
Re-irradiation for loco-regional failure of head and neck cancer or second primary tumours in previously irradiated areas after a full course of (chemo-)radiation poses a challenging problem for radiation oncologists. Salvage surgery remains the standard of care, which however, is the case in only 20 % of the cases. Chemotherapy alone is not considered a curative treatment option.
Curatively intended (chemo-)radiation should be considered in well-selected cases and can be administered safely with a reasonable chance of long-term survival (approximately 15–20 %) but at the cost of severe increased acute and late toxicity. The results of taxane-based chemo-re-irradiation protocols are most promising.
In case of adverse prognostic factors, immediate postoperative (chemo-)re-irradiation after salvage surgery can be administered safely and significantly improves loco-regional control. Severe treatment-related morbidity remains of major concern. However, most series on re-irradiation published so far did not use fractionation schedules and techniques considered most optimal. Improvement of the therapeutic ratio can be expected from altered fractionation schedules, by limiting the target volume to the high-risk areas and by using more advanced radiation technologies.
Future studies should focus on new developments that proved to be effective in the primary treatment of head and neck squamous cell cancer (HNSCC). In this respect, new induction chemotherapy regimens using TPF and the addition of cetuximab to radiation are of great interest as these approaches might improve loco-regional control and overall survival without increasing treatment-related morbidity.
The original version of this chapter was revised. An erratum to this chapter can be found at 10.1007/978-3-319-41825-4_78.
1 Introduction
Radiotherapy plays a pivotal role in the curative treatment of head and neck squamous cell carcinoma (HNSCC). Currently, the majority of patients with HNSCC have locally advanced disease and are treated with radiotherapy either alone or in combination with other modalities, such as surgery, chemotherapy and/or biological targeting agents. Despite the advances made in the primary treatment of HNSCC, still 30–50 % of all curatively treated patients will develop a loco-regional recurrence (Blanchard et al. 2013, 2015). In addition, for those who survive, there is a constant threat of the development of a new head and neck tumour. In a meta-analysis, the incidence of second primary tumours (SPTs) was 14.2 % (Haughey et al. 1992). Given that most patients received radiation treatment to the primary site as well as to the regional lymph node areas, the vast majority of these recurrences and SPTs will occur in previously irradiated areas.
In most cases the previous radiation dose administered is just below the generally accepted tolerance dose of the normal tissues, and although some recovery is likely to occur over time, the exact additional dose that can be administered safely to these normal structures remains to be determined. Therefore, in the re-irradiation setting, most radiation oncologists are much more reluctant with regard to the radiation dose to the normal tissues in general and in particular to the most critical structures, such as the spinal cord, the larynx and the optic nerves and chiasm. On the other hand, in order to achieve satisfactory rates of loco-regional tumour control, the total dose administered to the high-risk areas should at least be in the range of what is normally considered curative. Therefore, recurrent and second primary HNSCC after curative (chemo-)radiation in previously irradiated areas poses an important and difficult therapeutic challenge for radiation oncologists. In this chapter, a number of issues related to curatively intended re-irradiation either or not in combination with other modalities will be discussed.
2 A Changing Population
In the last decades, a major progress has been made in the treatment of patients with HNSCC. In particular, the addition of concomitant chemotherapy (Langendijk et al. 2004; Pignon et al. 2009; Blanchard et al. 2013, 2015) and cetuximab (Bonner et al. 2006, 2010) to radiation and the introduction of altered fractionation schedules (Baujat et al. 2010; Blanchard et al. 2011) have resulted in a significant improvement of loco-regional tumour control and overall survival. These new treatment regimens have gained conceptual acceptance and are now considered standard among patients with HNSCC in the organ preservation as well as in the unresectable setting. In most studies reporting on the results of (chemo-)re-irradiation in HNSCC, patients included received their initial treatment before the 1990s most likely with conventional fractionation schedules and without the addition of chemotherapy (Weppelmann et al. 1992; Spencer et al. 1999; Schaefer et al. 2000; De Crevoisier et al. 1998, 2001). Moreover, in that period, planning CT scans and 3D dose calculations were not routinely used, and most patients were treated after direct simulation. The same accounts for patients treated with primary surgery and postoperative radiotherapy. Since the publication of the results of two prospective randomised studies, an increasing number of patients are now treated with postoperative concomitant chemo-radiation instead of postoperative radiotherapy alone (Bernier et al. 2004; Cooper et al. 2004), in particular in case of high-risk factors for loco-regional failure, such as positive surgical margins and lymph node metastases with extranodal spread (Bernier et al. 2005). As a consequence of these changes in what is currently considered standard treatment, there are two major concerns. First, it should be noted that loco-regional failures among patients currently treated with CT-guided 3D conformal radiotherapy or intensity-modulated radiotherapy (IMRT) with altered fractionation schedules and/or in combination with concomitant chemotherapy are less frequent than after conventional RT alone, suggesting the selection of more radioresistant cases compared to those described in earlier studies. Therefore, it should be questioned as to whether translation of the results obtained from these earlier studies on re-irradiation to patients that underwent more effective initial treatment regimens is justified. Tumours recurring in previously irradiated areas after more effective chemo-radiation regimens will originate from perhaps more radioresistant clonogens, and we cannot rule out that (chemo-)re-irradiation could be less effective in these patients than after conventionally fractionated radiotherapy alone. Indeed Nagar et al. found that both disease-free survival and overall survival after chemo-re-irradiation were markedly and significantly worse among those that were initially treated with chemo-radiation as compared to those who initially received radiotherapy alone (Nagar et al. 2004). In that study, none of the patients that received chemo-radiation as initial treatment were disease-free at 1 year and all patients died within 2 years after chemo-re-irradiation. Moreover, in a retrospective study including re-irradiated HNC patients from nine consecutive phases I–II trials, initial treatment with chemo-radiation was an adverse prognostic factor for overall survival (Choe et al. 2011). These results support the hypothesis that the current population of patients with recurrent HNC in previously irradiated areas considered for re-irradiation have less favourable outcome when initially treated with chemo-radiation than those included in earlier reports that mainly included patients initially treated with radiotherapy alone.
3 Patient Selection
As re-irradiation, either or not in combination with other modalities, is associated with a considerable risk on severe acute and late treatment-related side effects, proper selection of patients is essential to further improve the therapeutic ratio. From this point of view, identification of reliable and validated prognostic factors is essential. Moreover, the possibility of alternative treatment approaches should be taken into consideration, and the previous radiation treatment should be analysed thoroughly.
3.1 Prognostic Factors
There are a number of methodological problems with regard to the identification and validation of prognostic factors in the re-irradiation setting, including (1) differences in eligibility criteria and subsequent heterogeneity of the study populations among the different studies, (2) the retrospective design of most studies, (3) the relatively limited number of patients included with insufficient power to detect clinically relevant prognostic factors and (4) the large variety of treatment regimens used. Nevertheless, despite these methodological shortcomings, there are a limited number of prognostic factors that seem to be important.
Tanvetyanon et al. reported on a retrospective analysis on prognostic factors for survival among patients treated with curatively intended salvage re-irradiation for head and neck cancer (Tanvetyanon et al. 2009). The study population was composed of patients with recurrent tumours as well as SPTs, and 46 out of 103 patients underwent salvage surgery and postoperative re-irradiation. With this nomogram, the probability of death at 24 months after initiation of re-irradiation can be predicted with a combination of prognostic factors, including comorbidity (based on the Charlson index), organ dysfunction prior to re-irradiation, isolated neck recurrence, tumour bulk and time interval between completion of previous therapy and initiation of re-irradiation. The performance of this nomogram showed good agreement between predicted and observed outcomes, with a C-index of 0.75. The factors included in this nomogram generally reflect the most frequently reported prognostic factors in the re-irradiation setting (Stell 1989; Spencer et al. 2001, 2008). However, the number of patients in this analysis was relatively small, and other potential prognostic factors such as recurrent versus SPT, total dose of radiation, previous chemo-radiation (Spencer et al. 2001, 2008) and radiation technique were not identified as significant prognostic factors. Nevertheless, the nomogram could be a useful tool to select patients with favourable outcome for the more intensified (chemo-)re-irradiation strategies.
Choe et al. reported on a retrospective multivariable analysis of 166 previously irradiated patients with locally advanced non-metastatic HNC that were either treated with salvage surgery followed by adjuvant concurrent chemo-re-irradiation or definitive chemo-re-irradiation (Choe et al. 2011). They identified four independent prognostic factors for overall survival, including salvage surgery before chemo-re-irradiation (yes/no), previous chemo-radiation (yes/no), total dose of re-irradiation (<60/≥60 Gy) and interval between end of first treatment to initiation of chemo-re-irradiation (<36/≥36 months). The 5-year overall survival of patients with 0–1 adverse prognostics factors was around 30 %, compared to 10 % and 0 % for those with 2 and 3–4 adverse prognostic factors, respectively. This latter model is a rather simple and therefore very practical tool to stratify patients into distinct risk groups and to support decision-making for the most suitable salvage strategy.
More recently, Riaz et al. reported on the development of a nomogram that predicts 2-year loco-regional control after re-irradiation either as single modality or combined with surgery or concurrent chemotherapy. This nomogram included five prognostic factors, including stage, tumour site, organ dysfunction, salvage surgery and total dose of re-irradiation (Riaz et al. 2014).
An important finding in two of the aforementioned studies was that comorbidity and pre-existing organ dysfunction were important prognostic factors (Tanvetyanon et al. 2009; Riaz et al. 2014). More specifically, the median overall survival among patients with neither significant comorbidity nor pretreatment organ dysfunction was 59.6 months which was markedly better compared to those with both comorbidity and organ dysfunction, in whom the median survival was only 5.5 months with no survivors beyond 2 years of follow-up (p < 0.001) (Tanvetyanon et al. 2009). These two factors are probably important because they may increase the risk of cancer-related death due to poor treatment tolerance and compliance and/or increase the risk of non-cancer-related death. Moreover, organ dysfunction, which is mainly due to radiation-induced toxicity from the previous treatment, may also be a surrogate marker of a more aggressive biological behaviour of the tumour. Hence, given the large impact on overall survival, both factors may interact negatively with (chemo-)re-irradiation, but may also be a competing risk of death.
3.2 Alternative Treatment Options
Before deciding for (chemo)re-irradiation, other treatment options should be taken into account as well. In particular in case of resectable loco-regional recurrences and/or SPTs, surgery should be considered and is traditionally regarded as the standard of care (Gilbert and Kagan 1974; Pradhan et al. 1980; Goodwin 2000), while chemotherapy and (chemo-)re-irradiation have been reserved for unresectable cases or as adjuvant modality after salvage surgery (De Crevoisier et al. 1998, 2001). However, only approximately 20 % of the patients are candidates for curative resections (Ridge 1993; Mabanta et al. 1999). In addition, the results of salvage surgery are relatively poor. The results of a meta-analysis on salvage surgery in HNSCC, based on 1,633 patients from 32 studies, revealed a 5-year overall survival rate of approximately 40 % (Goodwin 2000). The 5-year survival tended to be better among patients with recurrent cancer of the larynx (48 %) and oral cavity (43 %) than among those with recurrent disease in the oropharynx (26 %). Better outcome of salvage surgery in patients with laryngeal and hypopharyngeal cancer with loco-regional recurrences after concurrent chemo-radiation has been confirmed in a recent retrospective study (Putten et al. 2015). Of the 66 patients that developed loco-regional recurrence after concurrent chemo-radiation, 22 underwent salvage surgery (33 %). Independent favourable predictive factors for salvage surgery were younger age and laryngeal cancer. The 5-year overall survival rate was 27 % as compared to 0 % in patients that were not salvaged by surgery. However, this higher survival rate came at the cost of 14 % major complications.
It should be noted that survival data were not available stratified by stage or interval between primary and recurrence, demonstrating one of the limitations of the aforementioned meta-analysis (Goodwin 2000). In this regard, Zafareo et al., who reported on the results of a retrospective study on the role of salvage surgery in patients with recurrent squamous cell carcinoma of the oropharynx (Zafereo et al. 2009), showed that the outcome after salvage surgery may depend on a number of other prognostics factors. These authors identified 199 patients with locally recurrent oropharyngeal cancers, after excluding patients with regional metastases only or distant metastases, who had been treated with definitive radiotherapy in the past. Out of these 199 patients, only 41 (21 %) were selected for salvage surgery and the 3-year overall survival was 42 %. The results of that study indicated that favourable surgical salvage candidates are younger, have smaller recurrent tumours for which it is possible to obtain free surgical margins and have no recurrent neck disease. Other studies showed that the interval between the previous treatment (Stell 1991; Llewelyn and Mitchell 1997; Agra et al. 2006) and recurrence and disease stage (Lacy et al. 1999; Goodwin 2000; Agra et al. 2003, 2008) are important adverse prognostic factors for salvage surgery as well. Nevertheless, the risk of developing a second recurrence after salvage surgery remains high, with approximately two-thirds of the patients developing such an event within the first year of salvage surgery (Kim et al. 2007; Zafereo et al. 2009), emphasising the potential importance of postoperative (chemo)re-irradiation, which will be discussed later.
The results after salvage surgery alone and the fact that postoperative (chemo-)re-irradiation may be indicated after salvage surgery should be taken into account when deciding for either primary (chemo-)re-irradiation or salvage surgery. From this point of view, it is worthwhile to notice that the outcome after salvage surgery followed by postoperative (chemo-)re-irradiation appears to be superior to that after (chemo-)re-irradiation alone. Salama et al. reported a 5-year progression-free survival of 51 % after postoperative (chemo-)re-irradiation, which was significantly better as compared to (chemo-)re-irradiation in which the progression-free survival was only 19 % (Salama et al. 2006). In addition, Kasperts et al. reported on the results of a retrospective study that included 39 patients that underwent surgery for SPTs or loco-regional recurrences followed by postoperative re-irradiation without chemotherapy (Kasperts et al. 2006). All patients had positive surgical margins and/or lymph node metastases with extra-nodal spread and were therefore considered to have a high or very high risk for loco-regional failure. In this study, the 3-year loco-regional control and overall survival rates were 74 % and 44 %, respectively. These results did not significantly differ from the results obtained among patients that underwent surgery and postoperative radiotherapy as initial treatment.
It should also be noted that, as in the case of intensified (chemo-)re-irradiation, complications after salvage surgery in a previously irradiated area are an important problem as well, reported in approximately 20–40 % of the cases (Goodwin 2000). As expected, the frequency of complications is larger following more extensive surgery required for stage III and IV disease. Wound complications seem to be a manageable problem, although occurring in a considerable proportion of patients (approximately 50 %) (Langendijk et al. 2005; Agra et al. 2008; Putten et al. 2015). However, perioperative deaths are relatively rare. Nowadays, the availability of myocutaneous flaps, as well as free flaps with microvascular anastomosis, provides the surgeon with a wide array of opportunities to bring non-irradiated tissue into the surgical field for reconstruction.
Chemotherapy alone for recurrent HNSCC is generally not considered a curative treatment option, although progress has been made in the treatment of metastatic and recurrent disease among patients not suitable for more aggressive local treatments such as salvage surgery or re-irradiation. In case of systemic treatment alone, platinum-based chemotherapy is considered the current standard (Hong et al. 1983; Forastiere et al. 1992; Arnold et al. 2004; Gibson et al. 2005; Sacco and Cohen 2015). The only regimen that showed significant outcome improvement as compared to platinum-based chemotherapy alone in approximately 30 % is the combination of platinum, fluorouracil and cetuximab (Sacco and Cohen 2015). The addition of cetuximab to platinum-based chemotherapy with fluorouracil revealed an overall survival improvement from 7.4 months with chemotherapy alone group to 10.1 months after chemotherapy plus cetuximab (Vermorken et al. 2008). Although these results are encouraging, systemic treatment alone cannot be regarded as curative treatment option in the long term and should be reserved for patients with recurrent disease that are not eligible for intensified loco-regional treatment anymore and/or for those with distant metastases. Indeed, in a retrospective analysis, Datta et al. found that patients with residual or recurrent disease after curative radiotherapy showed better outcome after chemo-radiation compared to chemotherapy alone with a 5-year overall survival rate of 19 % after chemo-radiation versus no survivors at 5 years after chemotherapy alone (Datta et al. 2003). However, randomised controlled trials comparing these two strategies are still lacking, and we can therefore not rule out that selection bias may account for at least part of the beneficial effect of chemo-radiation compared to chemotherapy alone.
3.3 Recurrence Analysis
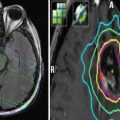
Given that patients developing loco-regional recurrences and/or SPTs in previously irradiated areas have been treated with more aggressive regimens and the fact that more advanced radiation delivery techniques, such as IMRT, are being used, allowing for better dose conformation to the target volume reference to the tissues outside the target volume, it becomes increasingly important to analyse the exact location of the loco-regional recurrence reference to the initial radiation dose distributions. If the radiation dose at the site of recurrence is significantly lower than the prescribed dose at the gross tumour volume (GTV), e.g. in the case of a recurrence in an electively treated neck, or in case of geographical miss, that loco-regional failure is less likely to be due to intrinsic radioresistance, and (chemo-)re-irradiation will probably be more effective than in case of loco-regional failures occurring in a high-dose area. For this reason, all cases considered for (chemo-)re-irradiation should be subjected to a thorough 3D reconstruction and analysis of the initial treatment portals and dose distributions. This so-called ‘recurrence analysis’, using both planning CT of the initial treatment co-registered with the CT scan of the recurrence preferably combined with other advanced imaging modalities such as positron emission tomography (PET) and/or MRI, is an essential step in the decision process for curative (chemo-)re-irradiation.
4 Primary (Chemo-)re-irradiation
As most patients initially underwent a full course of radiotherapy, it is reasonable to assume that radiation-resistant tumour clonogens exist and that a second course of radiation alone to the same or lower dose would not likely sterilise these resistant clones. There are a number of potential options to overcome the problem of radioresistance, including dose escalation and by radiation-sensitising strategies, e.g. the addition of chemotherapy and/or molecular-targeting therapies.
4.1 Re-irradiation Alone
A number of authors reported on the results of re-irradiation with external beam radiotherapy alone. In the older studies, patients were generally treated with standard fractionation and conventional radiation techniques (Stevens et al. 1994), sometimes combined with brachytherapy. In these older studies, the local control rates varied from 27 % in case of recurrent tumours to 60 % in case of SPTs, while the 5-year overall survival rate varied from 17 % among patients with recurrent tumours to 37 % among those with SPTs (Skolyszewski et al. 1980). For some subsets, the outcome was markedly better, e.g. in the series of Wang et al. who only included early-stage second primary laryngeal tumours, the 5-year overall survival was 93 % (Wang and McIntyre 1993). The problem with the reports on re-irradiation alone is that they are all retrospective, based on single centre experiences, including highly selected patient and heterogeneous patient groups, treated with rather outdated radiation technologies.
More recently, some authors reported on re-irradiation alone with more modern techniques, such as 3D-CRT and IMRT (Dawson et al. 2001). A total of 34 patients with a SPT (n = 26) or loco-regional recurrence (n = 8) were treated with a second course of high-dose radiotherapy. Patients were selected for re-irradiation in case of inoperable and/or unresectable tumours to a total dose of 60 Gy with conventional fractionation. The loco-regional control rate after 2 years was 27 % and the 3-year overall survival was 22 %.
4.2 Is There a Dose-Effect Relationship?
In the primary treatment of HNSCC, dose escalation by hyperfractionated regimens provides higher loco-regional control rates without a significant increase in late radiation-induced morbidity. Although there are no phase III studies on dose escalation in the re-irradiation setting, the results of retrospective analyses suggest that higher radiation doses are associated with better loco-regional tumour control.
A significant association between total re-irradiation dose and outcome was found by Datta et al. (2003). The population of this study was composed of 124 patients with residual or recurrent lesions treated with either re-irradiation alone or in combination with induction or concomitant chemotherapy. The total response rate was significantly higher when the total dose of re-irradiation was ≥40 Gy (91 versus 33 %, p < 0.001), which also translated in a significant difference in overall survival (multivariate analysis).
Schaefer et al. treated 32 patients with external beam split-course radiation therapy with concomitant hydroxyurea and 5-fluorouracil for 5 days followed by 9 days of rest (Schaefer et al. 2000). This cycle was repeated every 2 weeks until a cumulative soft tissue radiation dose of 110 Gy (including prior radiation therapy) was reached. In this study, the median overall survival and progression-free survival among patients treated with ≤50 Gy were 9.0 and 14.2 months compared to 0.0 and 5.0 months, respectively, among patients that received a total dose of 40–49 Gy.
In another study, patients that received a dose of >50 Gy had a significantly better overall survival rate compared to those that received ≤50 Gy, which remained significant in the multivariate analysis (HR 0.45; 95 % CI 0.26–0.76; p = 0.002) (Choe et al. 2011). Similar results were shown by Riaz et al. who found that radiation dose was an independent prognostic factor for loco-regional control in a multivariable analysis, with a hazard ratio of 0.57 (95 % ci, 0.38–0.85) for patients treated with 50 Gy or higher as compared to patients treated with a dose of less than 50 Gy (Riaz et al. 2014).
Salama et al. (2006) reported on the results achieved in 115 patients with loco-regionally recurrent non-metastatic or second primary HNSCC treated in seven consecutive phases I–II protocols at the University of Chicago with high-dose chemo-re-irradiation. In patients treated with a total dose ≥58 Gy, the 3-year loco-regional control rate, progression-free survival and overall survival was 56 %, 38 % and 30 %, respectively, which was significantly better compared to those treated with a total dose of <58 Gy, in which the 3-year loco-regional control rate, progression-free survival and overall survival was 33 %, 21 % and 6 %, respectively. The total dose turned out to be an independent prognostic factor in the multivariate analysis. This dose-effect relationship was most pronounced in the subset of patients with unresectable disease. More recently, Choe et al. found that the total dose of re-irradiation was an independent prognostic factor for overall survival, with a hazard ratio of 0.35 (95 % ci, 0.23–0.53; p < 0.001) for patients that received <60 Gy versus patients that received 60 Gy or more (Choe et al. 2011).
However, in other studies no significant dose-effect relationships were found, which may also be due to the low number of patients included in these studies resulting in too low statistical power to detect clinically relevant differences between the various dose levels.
These results at least suggest that higher dose levels of re-irradiation result in better loco-regional control and/or overall survival rates. However, it remains difficult to determine the most appropriate dose level in this setting, as it remains unclear if the better survival rates after higher dose levels may be contributed to better patient selection. Given that most patients with recurrent tumours already failed after a curative dose of 66–70 Gy of the previous treatment, it is very unlikely that sufficient loco-regional control rate can be achieved when a much lower dose will be used in the re-irradiation setting. The same line of reasoning is applicable for SPTs in previously irradiated areas. There is no reason to believe that a lower dose of radiation than usually applied in the primary setting will result in satisfactory loco-regional control rates.
Therefore, in case of curatively intended (chemo-)re-irradiation, a total dose of at least 60 Gy with standard fractionation or a biologically equivalent dose using hyperfractionation is required. Preferably, hyperfractionation with a moderate reduction of the overall treatment time of radiation (Fu et al. 2000) will be most optimal in this setting.
4.3 Chemo-re-irradiation
In a previous report, an overview regarding the results achieved with chemo-re-irradiation was provided (Kasperts et al. 2005). In summary, in most of these series, chemotherapy mainly consisted of 5-FU and hydroxyurea, as originally described by Vokes et al. (1989) using alternating chemo-re-irradiation protocols. In these series, 2-year overall survival rates varying between 5 and 45 % have been reported (Weppelmann et al. 1992; Spencer et al. 1999; Schaefer et al. 2000).
The first prospective multi-institutional trial testing a re-irradiation plus chemotherapy regimen was conducted by the RTOG (RTOG protocol 9610) (Spencer et al. 2008). In this study, 79 patients with unresectable recurrent and second primary tumours were enrolled and analysed. The 2- and 5-year survival rates were 15 % and 3.8 %, respectively. The 5-year overall survival rate in this study was somewhat disappointing, but is similar to that reported by others (De Crevoisier et al. 1998). These results were obtained at the cost of considerable acute and late toxicity. In total, 17.7 % and 7.6 % of the patients experienced grade 4 and grade 5 mainly haematological acute toxicity. Late toxicity was mainly related to radiotherapy with 19.4 % grade 3 and 30 % grade 4 toxicities. Approximately 70 % of the patients were tube-feeding dependent at the last follow-up.
The trials that reported higher survival rates generally used more effective chemotherapy regimens and higher total doses of re-irradiation and/or included patients treated with postoperative chemo-re-irradiation (Langendijk et al. 2006; Milano et al. 2005).
In the primary setting, the results of a number of prospective studies showed that induction chemotherapy with taxanes, cisplatin and 5-FU (TPF) followed by radiotherapy or concomitant chemo-radiation is more effective than induction chemotherapy with cisplatin and 5-FU alone. The addition of taxanes in the chemo-re-irradiation setting is of interest as the results of preclinical data suggest that taxanes are particularly effective in radiotherapy-resistant squamous cell carcinoma cell lines (Britten et al. 1998).
During the last 5 years, a number of authors reported on (chemo-)re-irradiation protocols containing taxanes (Hehr et al. 2005; Kramer et al. 2005; Langer et al. 2007).
Kramer et al. (2005) reported on the results obtained in 38 patients with recurrent unresectable HNSCC that were treated in two prospective phases I–II trials at the Fox Chase Cancer Center. Patients were treated with split-course re-irradiation and concomitant cisplatin and paclitaxel. In this study, the 2-year overall survival was 35 %, with a progression-free survival at 1 year of 33 %, with increased but acceptable treatment-related morbidity.
Of note is the phase II study conducted by the RTOG (RTOG protocol 9911) (Langer et al. 2007). The study population of this study was composed of 105 patients with loco-regional recurrences or SPTs in previously irradiated areas. The protocol consisted of twice-daily radiation (1.5 Gy per fraction bid) for 5 days every 2 weeks up to a total dose of 60 Gy combined with cisplatin 15 mg/m2 daily and paclitaxel 20 mg/m2 daily for 5 days every other week. The protocol showed reasonable compliance with 74 % of the patients completing the planned chemotherapy and 76 % of the patients receiving at least 52.5 Gy of radiation. However, the toxicity of this protocol was substantial, with a relatively high incidence of treatment-related deaths and late grade 4 or worse toxicities. Grade 4 or worse acute radiation-induced and haematologic toxicity presented in 28 % and 21 % of the cases, respectively. There were 8 % treatment-related deaths of which 5 % in the acute phase. In addition, there were three fatal late complications, including two carotid haemorrhages and one death attributable to oral-cutaneous fistula and soft tissue necrosis. The median overall survival was 12.1 months and the 1- and 2-year overall survival rates were 50.2 % and 25.9 %, respectively, which was significantly better than observed in RTOG 9601 in which the 1- and 2-year survival rates were 47.1 and 16.9 % (p = 0.044).
It should be stressed that definitive conclusions from these relatively small phase II studies are difficult to draw, but the results of taxane-based chemo-re-irradiation regimens are certainly promising with relatively impressive tumour control and survival rates but at the cost of increased and significant acute and late morbidity. As compared to the previously reported RTOG protocol (RTOG 9601), the results of taxane-based chemo-re-irradiation protocols appear to be better.
Based on these results, the question arises as to whether concurrent chemo-re-irradiation yields better results than chemotherapy alone containing cisplatin either or not in combination with taxanes, which was investigated in a prospective randomised study (RTOG 0421) (Wong et al. 2006). Unfortunately, this study was terminated due to poor patient accrual.
4.4 Re-irradiation Combined with Cetuximab
The results of a phase III randomised study in the primary setting demonstrated that the epidermal growth factor receptor (EGFR) inhibitor cetuximab given concomitantly with radiotherapy significantly improved LRC and OS compared to radiotherapy alone without any increase in radiation-induced toxicity (Bonner et al. 2010). Therefore, the use of agents directed against specific molecular targets in general and the EGFR receptor in particular might be a more promising approach. This is supported by the fact that the use of anti-EGFR targeting alone (cetuximab) has been shown to be effective in refractory HNSCC patients, progressing under salvage chemotherapy (Baselga et al. 2005). The number of reports on the combination of re-irradiation and cetuximab is increasing (Balermpas et al. 2009; Jensen et al. 2010; Lartigau et al. 2013; Dornoff et al. 2015).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree