Abnormalities characterized by increased lung opacity can be divided into two categories based upon their attenuation: ground glass opacity (GGO) and consolidation. Each of these findings tends to be nonspecific and has a long differential diagnosis. Clinical information, particularly the duration of symptoms, can limit the diagnosis when either of these findings is present.
GROUND GLASS OPACITY
On HRCT, GGO is characterized by hazy regions of increased lung opacity or attenuation in which vessels remain visible (Fig. 4.1). GGO represents the presence of abnormalities below the resolution of HRCT. It may reflect the presence of alveolar disease, interstitial disease, or a combination of both, and it may be a manifestation of lung infiltration, active inflammation, or fibrosis (Fig. 4.2). GGO may also result from atelectasis.
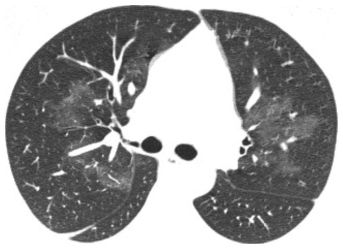
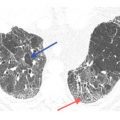
Figure 4.1
Ground glass opacity (GGO). Hazy regions of opacity are noted in the parahilar lung in this patient with acute pulmonary hemorrhage due to Wegener’s granulomatosis. Vessels are well seen in the areas of opacity; this finding defines GGO.
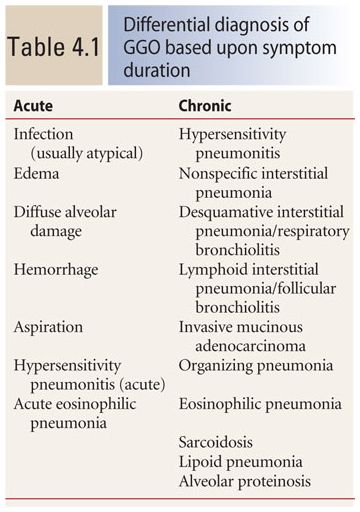
The differential diagnosis of GGO is broad and includes a variety of diseases in different disease categories. The duration of symptoms (i.e., acute or chronic) is important in limiting the initial differential diagnosis (Table 4.1). In general, the symptoms should be considered acute when they have been present for less than a few weeks and chronic if they have been present for 6 weeks or more.
GGO with Acute Symptoms
In a patient with acute symptoms, the most common causes of GGO include infection, most notably atypical infections such as viral pneumonia, Pneumocystis jiroveci, and atypical bacterial infections (e.g., Legionella, Mycoplasma pneumoniae, and Chlamydia pneumoniae); pulmonary edema, either hydrostatic or increased permeability edema; diffuse alveolar damage, the histologic abnormality present in patients with acute respiratory distress syndrome; pulmonary hemorrhage; and aspiration (Table 4.1). Additional causes include an acute presentation of hypersensitivity pneumonitis and acute eosinophilic pneumonia.
In the acute setting, the various causes of GGO are difficult to distinguish from one another based on their appearance. The specific distribution of GGO (diffuse, symmetric, patchy, nodular, or focal) is of limited use in narrowing the differential diagnosis (Fig. 4.3). Even processes such as pulmonary edema, which are commonly symmetric or diffuse, can produce patchy, focal, or nodular opacities in some patients (Fig. 4.4), suggesting a specific diagnosis in a patient with acute symptoms and GGO aided by history (e.g., immunosuppression or AIDS, exposures, and known cardiac disease) and the specific presenting symptoms (e.g., fever, sputum production, and hemoptysis).
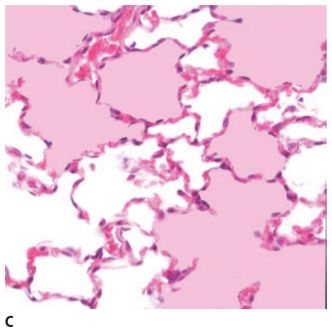
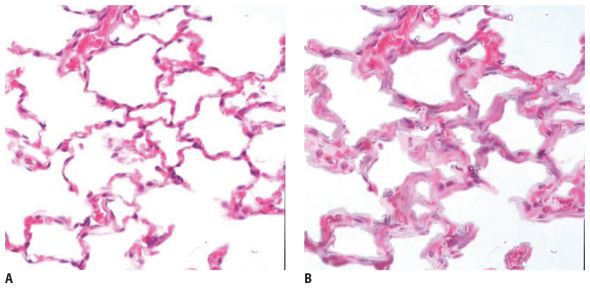
Figure 4.2
Causes of ground glass opacity (GGO). A. Normal alveoli. B. Simulated alveolar wall thickening in interstitial disease. Increased tissue within the volume scanned results in GGO. C. Simulated alveolar disease, with some alveoli filled with fluid. This results in increased attenuation, but because some alveoli remain aerated, consolidation does not result.
One HRCT finding that may be helpful in diagnosis is the presence of smooth interlobular septal thickening. When this finding is conspicuous and associated with GGO, pulmonary edema is the most likely diagnosis (Fig. 4.5). The presence of lung cysts associated with GGO suggests Pneumocystis jiroveci infection.
GGO with Chronic Symptoms
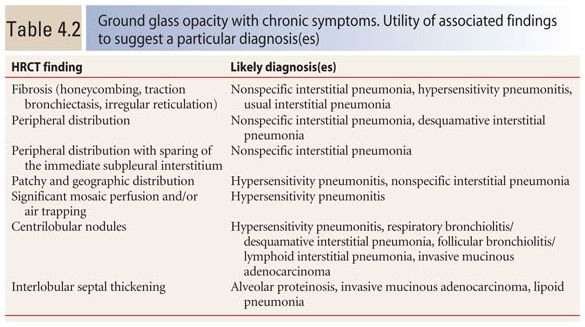
When GGO is associated with chronic symptoms, the differential diagnosis is different and very broad. Possible causes include hypersensitivity pneumonitis, nonspecific interstitial pneumonia (NSIP), desquamative interstitial pneumonia (DIP) and respiratory bronchiolitis (RB), lymphoid interstitial pneumonia (LIP) and follicular bronchiolitis, invasive pulmonary mucinous adenocarcinoma, organizing pneumonia (OP), eosinophilic pneumonia, sarcoidosis, lipoid pneumonia, and alveolar proteinosis. Several findings may be helpful in limiting the differential diagnosis (Table 4.2).
Distribution of GGO
When the distribution of GGO is strongly peripheral, an interstitial pneumonia is favored, most specifically NSIP or DIP, but eosinophilic pneumonia and OP may also show this appearance (Fig. 4.6). A peripheral distribution of findings with sparing of the immediate subpleural lung is highly suggestive of NSIP (Fig. 4.7).
A patchy and geographic distribution of GGO, with significant involvement of the central lung, is not typical of an interstitial pneumonia (i.e., NSIP, DIP, LIP, and OP), but is occasionally seen with NSIP in patients with connective tissue disease or LIP. This distribution is more suggestive of other causes of GGO such as hypersensitivity pneumonitis (Fig. 4.8).

Figure 4.3
Acute drug reaction with pulmonary edema and diffuse ground glass opacity (GGO). The differential diagnosis of GGO is broad. In a patient with acute symptoms, the distribution of GGO is of limited value in helping distinguish among the various possible causes. The diagnosis is often determined by the clinical history, as in this patient with drug toxicity resulting from treatment of lymphoma.
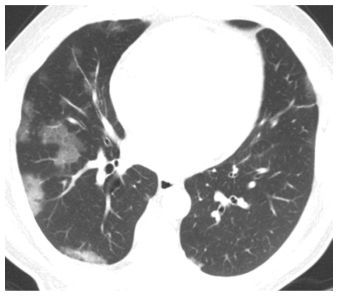
Figure 4.4
Acute pulmonary edema with patchy GGO. The distribution of GGO in the setting of acute symptoms is not particularly helpful in diagnosis. Even processes that are classically diffuse or symmetric, such as pulmonary edema, may occasionally present with focal or patchy abnormalities.
Associated Mosaic Perfusion and/or Air Trapping
If GGO is associated with significant mosaic perfusion and/or air trapping (involvement of multiple lobules in three or more lobes), the diagnosis of hypersensitivity pneumonitis is strongly favored (Fig. 4.9A, B). GGO associated with centrilobular nodules may be seen with hypersensitivity pneumonitis (Fig. 4.10), RB, follicular bronchiolitis, and invasive mucinous adenocarcinoma.
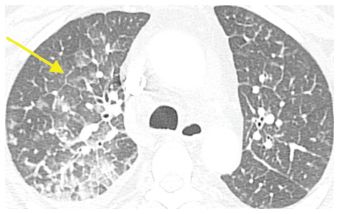
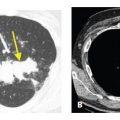
Figure 4.5
Pulmonary edema with a combination of ground glass opacity (GGO) and interlobular septal thickening. GGO in the acute setting is nonspecific, but when interlobular septal thickening (arrow) is a significant associated finding, pulmonary edema is the most likely etiology.
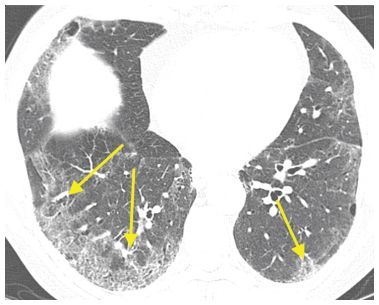
Figure 4.6
Desquamative interstitial pneumonia (DIP) with a peripheral distribution of ground glass opacity (GGO). In the chronic setting, GGO with a peripheral distribution (arrows) is suggestive of an interstitial pneumonia or more specifically nonspecific interstitial pneumonia, DIP, or usual interstitial pneumonia. This patient is a smoker with DIP.
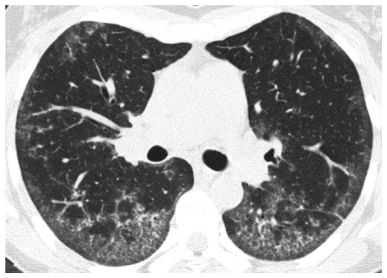
Figure 4.7
Nonspecific interstitial pneumonia (NSIP) with a peripheral distribution of ground glass opacity (GGO) and subpleural sparing. In this patient with NSIP, GGO shows a peripheral predominance, but the immediate subpleural lung is relatively spared. This distribution is typical of NSIP.
Figure 4.8
Hypersensitivity pneumonitis (HP) with a patchy and geographic distribution of ground glass opacity (GGO). In this patient with HP, the areas of GGO lack a peripheral predominance. This appearance is typical of HP.
Crazy Paving
The combination of GGO and smooth interlobular septal thickening in the same lung regions is termed “crazy paving.” This name refers to the appearance of irregularly shaped paving stones in an English garden.
While originally described as a typical HRCT finding in pulmonary alveolar proteinosis (Fig. 4.11), this finding is nonspecific and may be seen in any disease resulting in GGO. In the acute setting, the differential diagnosis is identical to that of isolated GGO and includes edema, atypical infections (Fig. 4.12), diffuse alveolar damage, hemorrhage, acute hypersensitivity pneumonitis, and acute eosinophilic pneumonia. In a patient with chronic symptoms, the list of diagnostic possibilities is the same as for GGO, but alveolar proteinosis, which is otherwise quite rare, should be considered a distinct possibility (Fig. 4.11).
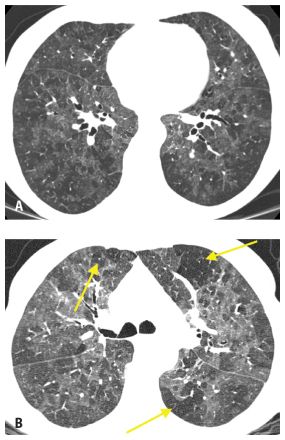
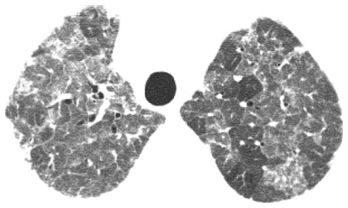
Figure 4.9
Hypersensitivity pneumonitis with patchy ground glass opacity (GGO) and air trapping. HRCT (A) shows nonspecific patchy GGO in a patient with chronic symptoms. Expiratory image (B) shows patchy air trapping (arrows). This combination of findings is strongly suggestive of hypersensitivity pneumonitis.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree