Chapter 15 Overview: The pharyngeal wall and tonsillar fossa are common locations of infection, particularly in children. Acute pharyngitis, which is diagnosed more than 7 million times per year, does not require imaging for diagnosis. However, when a peritonsillar abscess is suspected, imaging is indicated for diagnosis and surgical management in some cases.1 Etiology: Most pharyngitis cases are self-limited viral infections. Accounting for up to 30% of cases, acute bacterial pharyngitis is most often secondary to group A beta-hemolytic Streptococcus (GAS).1 Children with pharyngitis present with sore throat, fever, and odynophagia. Lack of improvement with antibiotics suggests the possibility of a peritonsillar abscess. The peritonsillar space is the most common abscess location in the neck.2 Imaging: Routine pharyngitis and tonsillitis do not require imaging.1 However, in children suspected of having complications, contrast-enhanced CT is performed.3 Findings of uncomplicated tonsillitis include unilateral or bilateral enlarged, enhancing tonsils with inflammatory stranding of the parapharyngeal fat. Abscess formation is suggested by a central hypodense fluid collection, with peripheral enhancement within or immediately adjacent to an enlarged tonsil (Fig. 15-1).3 Follow-up imaging is only performed in children with complications and persistent clinical symptoms.1,2 Figure 15-1 Parapharyngeal abscess in a 7-month-old male with fever and difficulty swallowing. Treatment: Viral tonsillitis is self-limiting and requires only supportive treatment, but GAS infections, confirmed by a rapid antigen test or throat culture, are initially treated with antibiotics. Children with recurrent tonsillitis are candidates for tonsillectomy.4 Those with focal fluid collections identified by CT may require surgical aspiration and drainage. Tonsillar and peritonsillar infections have an excellent prognosis.1,2 Overview: Also known as suppurative thrombophlebitis of the internal jugular vein, Lemierre syndrome is an uncommon complication of oropharyngeal infection occurring most often in previously healthy teenagers.5 Although rare, complications, including septic dissemination with abscess formation in other parts of the body (most commonly in the lungs), osteomyelitis, and arterial vasospasm or occlusion leading to infarction, may be severe.6 Etiology: Lemierre syndrome is caused by Fusobacterium infection, an anaerobic gram-negative bacterium found in normal oral flora.6 Fusobacterium necrophorum is the most common species, with F. nucleatum, F. mortiferum, or F. varium occurring less often. Recognition is important because of the high rate of morbidity and mortality associated with this syndrome.5,7 Infection spreads from the peritonsillar space into the internal jugular vein, causing thrombus formation.5 From the jugular vein, septic emboli may seed other organs such as the lungs and brain, leading to abscess formation.7,8 Spread to adjacent neck spaces, including the retropharyngeal space and osseous structures, may occur, causing osteomyelitis. Patients present with a recent history of sore throat, tenderness, swelling of the lateral neck, and fever.5 With pulmonary involvement, tachypnea, tachycardia, and hypoxia may be present. Blood cultures are positive for the causative organism.9 Imaging: As with other head and neck infections, Fusobacterium infections present acutely, requiring rapid evaluation. Contrast-enhanced CT is the initial imaging modality of choice. CT findings include inflammatory changes that may involve various spaces of the neck and lack of enhancement within the jugular vein indicating thrombus.5 Inflammatory findings range from enhancing soft tissues of cellulitis to focal fluid collections indicating an abscess (Figs. 15-2 and 15-3). Chest CT may be concurrently performed if respiratory symptoms are present, and a search for osseous involvement is part of the CT evaluation. Color Doppler ultrasonography is useful to visualize and follow thrombophlebitis but is not reliably able to visualize deep neck infection as may occur with Lemierre syndrome.5,6 Acute neurologic symptoms may be evaluated with CT or MRI, and both may be augmented by angiographic techniques as well.7 Figure 15-2 Lemierre syndrome (Fusobacterium necrophorum infection) complicated by stroke in a 6-year-old female presenting with fever, difficulty swallowing, and nuchal rigidity. Figure 15-3 Lemierre syndrome (Fusobacterium necrophorum infection) complicated by osteomyelitis in a 9-year-old with fever, neck pain, and sore throat. Treatment: High-dose intravenous antibiotics, including metronidazole, penicillin, and clindamycin, are the mainstay for treatment of Fusobacterium infection and have a high success rate. Anticoagulation therapy is used in up to 27% of patients, although its role is not completely clear.5 Follow-up imaging is performed in patients who do not defervesce as expected and those with complications that may require closer follow-up. Although the prognosis of Fusobacterium infections is good with prompt recognition and treatment, the rates of morbidity and mortality are higher than with other head and neck infections.2,9 Overview: Retropharyngeal abscesses in children commonly result from suppurative lymphadenitis associated with tonsillitis, as well as with sinonasal and dental infections.10,11 Retropharyngeal abscess may rarely be caused by pharyngeal or esophageal perforation. The retropharyngeal space, the second most common location of abscess in the deep neck after the peritonsillar space, is a potential space that extends from the nasopharynx to the superior mediastinum.10 Abscesses extending below the T4 vertebra cause concern with regard to what is termed danger space infections, which have a high rate of morbidity. Other uncommon conditions that cause thickening of the retropharyngeal tissues include hemorrhage (especially in hemophilia), neuroblastoma, and rarely anterior myelomeningocele. Etiology: Retropharyngeal abscesses are sequelae of GAS, but Staphylococcus aureus and infrequent anaerobes have also been reported as causative organisms.2,10 The most common presenting symptoms are fever, neck pain, dysphagia, palpable neck mass, and sore throat. Cervical lymphadenopathy and torticollis are often present.11 Imaging: Plain radiography, often ordered as the initial study to screen for large fluid collections, is otherwise limited in its ability to distinguish between cellulitis and abscess, both of which may cause convex abnormal thickening of the prevertebral soft tissues (>8 mm at C2).4 Anterior displacement of the pharynx, esophagus, larynx, trachea, or all of these is seen from C1 to C4 (Fig. 15-4). Grisel syndrome is inflammation-induced laxity of the atlantoaxial joint, which may result in atlantoaxial rotatory subluxation or other malalignment of C1 and C2. This self-limiting sequence of symptoms and signs disappears with resolution of the inflammatory process. Contrast-enhanced CT is the study of choice to further check for hypoattenuating, rim-enhancing abscess collections and to determine the need for surgical drainage.4,10 If an abscess is present, CT is able to define the extent of the collection, to check for mediastinal involvement, and to detect other complications that may occur with head and neck infections such as thrombophlebitis and osteomyelitis.4 Figure 15-4 Retropharyngeal abscess in a 3-year-old female with sore throat and fever.
Infection and Inflammation
Pharyngotonsillitis and Peritonsillar Abscess
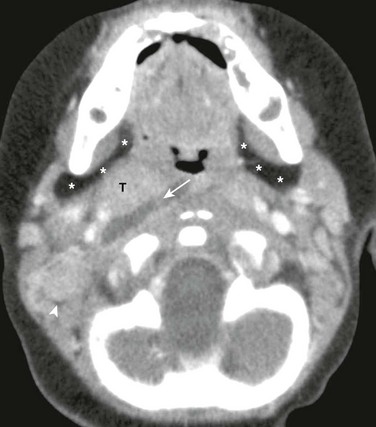
Axial contrast enhanced computed tomography image of the suprahyoid neck just below the skull base shows a well-defined, right-sided, low-attenuation fluid collection (arrow) adjacent to the tonsils (T). The right parapharyngeal fat (asterisks) and carotid spaces are displaced laterally. Also, note right-sided prominent lymph nodes (arrowhead) and normal left parapharyngeal fat (asterisks).
Lemierre Syndrome
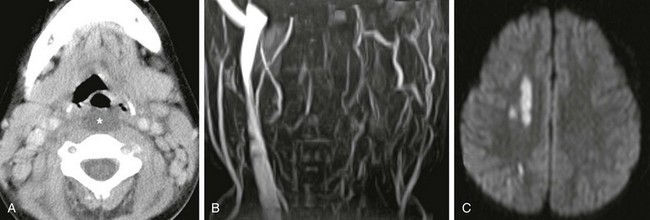
A, Axial contrast enhanced computed tomography image shows low-attenuation retropharyngeal fluid (asterisk). B, Magnetic resonance imaging 2 days later, performed because of acute left arm weakness, confirms lack of left internal jugular vein patency on magnetic resonance venogram. C, Diffusion-weighted image of the brain reveals multiple small foci of bright signal infarction secondary to emboli from thrombophlebitis, vasospasm, or both.

Sagittal reconstructed contrast enhanced computed tomography image demonstrates enlarged adenoids, a low-attenuation retropharyngeal fluid collection (asterisk), and a subperiosteal fluid collection along the ventral clivus (arrow). Air within and dorsal to the clivus due to osteomyelitis (arrowhead) is also seen. Venous occlusion was also present (not shown).
Retropharyngeal Abscess
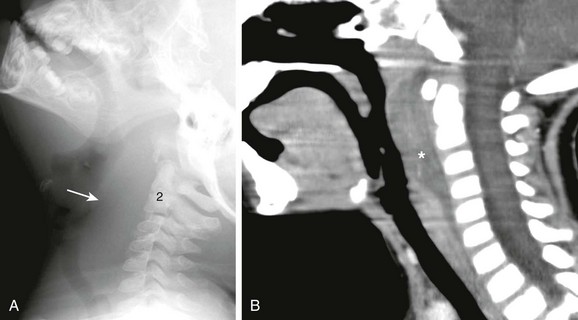
A, Lateral soft tissue neck radiograph reveals extensive soft tissue swelling displacing the airway anteriorly from the skull base to C6 (arrow). B, Sagittal reconstructed contrast-enhanced computed tomography confirms thickened, enhancing retropharyngeal soft tissues indicating cellulitis. Region of hypoattenuating fluid is concerning for retropharyngeal abscess (asterisk).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree