CHAPTER 16 This chapter describes the radiology of musculoskeletal infections, osteonecrosis and other marrow space disorders, and a few other skeletal conditions not covered elsewhere in this book. Acute osteomyelitis is a pyogenic infection of bone that typically occurs in a child who presents with an acute, systemic febrile illness. The infection is usually carried into the bone by the nutrient artery from a preexisting remote site of infection. Branches of the nutrient artery extend into the metaphysis, where they loop back and enter large sinusoidal veins. Slowing of blood flow in these sinusoidal veins permits bacterial colonies to grow and spread into the adjacent marrow where small abscesses form. Thrombosis from minor mechanical trauma may be an associated factor. From the initial focus in the metaphysis, the acute suppurative inflammatory process may extend throughout the medullary cavity. Edema and the collection of pus increase the pressure within the closed space of the medullary cavity, leading to decreased blood flow, thrombosis, and necrosis. Osteoclasts separate dead bone from living bone. Enzymes elaborated by inflammatory cells dissolve the necrotic bone. Under pressure, pus exudes through the cortex into the subperiosteal space by way of haversian and Volkmann canals. The periosteum becomes elevated by pus, stripping away the periosteal blood supply and leading to cortical osteonecrosis. Infection may penetrate the periosteum and extend into the soft tissues (Figs. 16.1–16.3). Where there is capsular investment of the metaphyseal cortex, the joint may become infected. Reactive periosteal bone forms a shell around the infection, called the involucrum (Fig. 16.4). The central, devitalized bone is called the sequestrum. Defects in the involucrum, called cloaca, may permit drainage of pus or extrusion of sequestra through fistulas. Hyperemia causes osteoporosis in the limb. Because the metaphyseal arteries do not penetrate the growth plate, the epiphysis is initially spared, but the infection may extend contiguously into the epiphysis, damaging the growth plate in the process. A solitary bone lesion that crosses the epiphyseal plate from the metaphyseal side is usually osteomyelitis. The common causative organism is Staphylococcus aureus. FIGURE 16.1. Acute osteomyelitis in the humeral metaphysis. A: Radiograph shows destruction (arrowhead) and involucrum (arrow). B: Coronal T2-weighted MRI shows marrow edema and subperiosteal pus (arrow). Source: From Chew FS, Schulze ES, Mattia AR. Osteomyelitis. AJR. 1994;162:942, with permission. FIGURE 16.2. Osteomyelitis in the femur. Axial T1-weighted fat-suppressed post-gadolinium MRI shows enhancement in the marrow and surrounding soft tissues, with a layer of periosteal reaction (involucrum) (arrow). FIGURE 16.3. Osteomyelitis in a child. A: Radiograph of the femur shows a lytic lesion in the distal metaphysis (long arrow). Periosteal reactive bone surrounds the femur (short arrow). B: Coronal T2-weighted MRI shows high signal within the lesion (long arrow), periosteal reactive bone (short arrow), and extensive surrounding soft-tissue edema. Soft-tissue extension of the infection is present. FIGURE 16.4. Osteomyelitis with layers of involucrum (arrow). Multifocal osteomyelitis is rare except in neonates. Because the nutrient vessels penetrate the epiphysis in neonates, early involvement of the epiphysis and growth plate is common, with extension into the joint. Effusion may be the only early radiographic clue to the presence of infection. Subsequent bony reaction is exuberant, with periosteal reaction often involving the entire bone. Fistula formation is rare. The organisms that commonly cause multifocal osteomyelitis in neonates are β-hemolytic Streptococcus and Escherichia coli. When infection is monostotic, S. aureus may also be a causative organism. Adults at risk for hematogenous osteomyelitis include patients who are debilitated or immunocompromised, elderly patients with genitourinary tract infections, patients with peripheral vascular insufficiency (especially diabetes), and intravenous drug abusers. Pathogens may also be implanted directly into the bone during trauma or surgery. Osteomyelitis does not occur in otherwise healthy adults. An antecedent history of trauma is common, and the bones of the hands and feet are commonly involved (Figs. 16.5 and 16.6). The feet are particularly vulnerable to infection as a complication of peripheral vascular disease. In adults, the initial location of infection is epiphyseal and subchondral because the nutrient artery loops into the sinusoidal veins at the ends of the bones. The common organism is Staphylococcus, unless the patient is immunocompromised. Contiguous spread of infection may involve the diaphysis, adjacent soft tissues, and joints. Fistula formation is frequent. Periosteal reaction may be minimal, especially in the feet. Because the periosteum is tightly applied, penetration of pus into the soft tissues is common, but subperiosteal collections are not. Multiple foci of infection do not occur. FIGURE 16.5. Osteomyelitis and septic arthritis involving the second and fourth MTP joints in an adult diabetic. The third toe and MTP joint were amputated previously. FIGURE 16.6. Diabetic osteomyelitis in the finger (arrow). Radiographic changes occur relatively late in acute osteomyelitis. Soft-tissue swelling with obliteration of fat planes may be seen 3 days after onset, at which time pus has already penetrated the cortex. Periosteal reaction and osteolysis may not be evident on radiographs until 5 to 7 days in children and 10 to 14 days in adults. If the suspected site contains fatty marrow, CT can reveal marrow infiltration by fluid and pus early in the course of osteomyelitis, before bone destruction is detectable. CT extends the radiographic ability to define sequestra, soft-tissue abscesses, sinus tracts, intramedullary and soft tissue gas, bone destruction, and reactive bone. MRI is highly sensitive and specific in distinguishing between osteomyelitis and adjacent soft-tissue infection, even in the presence of previous surgery, fracture, or chronic osteomyelitis. Early marrow edema is evident well before other imaging studies become abnormal, and subperiosteal or soft-tissue collections of pus can be identified early. The key finding on MRI is abnormal signal within the marrow, low signal on T1-weighted images, and high signal on T2-weighted images. Enhancement is generally seen after gadolinium injection on T1-weighted images. Abscesses have high signal on T2-weighted images with rim enhancement after gadolinium injection on T1-weighted images. The radionuclide bone scan is typically positive within 24 hours of onset, and a normal bone scan at this time eliminates osteomyelitis as a diagnostic possibility. Foci of acute osteomyelitis appear as areas of intense activity because of the hyperemia and reactive osteoblastic activity. Reactive hyperemia and osteoblastic activity are more extensive than the actual infected area. Devitalized, avascular areas of bone may appear as focal areas of decreased or absent activity, but the surrounding bone always has increased tracer uptake. Previous surgery, trauma, and other bone disease may complicate the interpretation of positive bone scans. Additional problem-solving imaging tools in suspected osteomyelitis are nuclear scans with labeled leukocytes or with gallium. Both of these radiopharmaceuticals localize at sites of WBC aggregation, such as collections of pus, but both may require delayed imaging 24 to 72 hours after injection. The gallium scan may be particularly useful in following the course of treatment to confirm healing and obviate concern about possible chronic osteomyelitis. Treatment of bacterial osteomyelitis with systemic antibiotics is effective when begun early. If there is pus formation and bone necrosis, the pus must be drained and the necrotic bone removed. Acute osteomyelitis may be complicated by chronic osteomyelitis. Chronic osteomyelitis may exist many years after acute osteomyelitis, even if the acute infection was treated appropriately. Systemic antibiotics are ineffective against organisms sequestered in necrotic bone. Blood cultures are almost always negative, and cultures of the lesion are often negative as well. A rare complication of longstanding, chronic, and draining osteomyelitis is development of malignancy—mostly squamous carcinomas—along the sinus tract. In chronic osteomyelitis, foci of bacteria persist within bone cavities that are filled with granulation tissue. Dense bone surrounds the site, and the cortex may be thickened as a result of long-term deposition of reactive medullary and periosteal bone (Fig. 16.7). Serpiginous sinus tracts may extend to the skin surface. Abscesses, sinus tracts, and sequestra may be obscured by the dense reactive bone, so that CT or MRI may be required. The radionuclide bone scan shows areas of increased uptake. Scans with gallium or labeled leukocytes should also be positive. FIGURE 16.7. CT scan of chronic sclerosing osteomyelitis of the clavicle. A Brodie abscess is a local, subacute bone abscess that is a fairly common cause of a solitary bone lesion. Symptoms of recurrent pain and local tenderness with swelling and erythema may be present for months or years. Most cases occur in adolescents and young adults, but the reported age range is from 6 to 61 years. Men are affected more often than women (by 2:1). The typical location is the metaphysis or diaphysis of the femur or tibia. A Brodie abscess may begin de novo, develop in the same site as a preceding episode of acute osteomyelitis, or follow an acute episode of osteomyelitis at another site. S. aureus appears to be the offending organism. Radiographically, a Brodie abscess appears as a well-defined lucent area in cancellous bone with smooth, rounded geographic margins and a thick sclerotic rind that may merge imperceptibly with the surrounding bone (Figs. 16.8 and 16.9). The lesion may appear lobulated with lucent, serpentine tracts extending along the bone. CT is valuable for defining the reactive sclerosis and can permit identification of tracts in the bone. The corresponding pathology is an avascular cavity, typically 1 to 4 cm in size, lined with granulation tissue and filled with fluid but not frank pus. Thickening of trabeculae adjacent to the lesion by reactive endosteal bone formation may form the sclerotic rind around the cavity. FIGURE 16.8. Brodie abscess in the distal tibia. FIGURE 16.9. Brodie abscess in the proximal tibia. A: Coronal T1-weighted MRI shows central lesion (arrow) with surrounding sclerosis. B: Coronal T1-weighted gadolinium-enhanced MRI shows enhancement of the periphery of the lesion (arrow), but not the center. Although Brodie abscesses have a characteristic appearance, they may be confused with other focal bone lesions, including tumors. The key radiologic feature of a Brodie abscess is the extensive reactive bone formation that has a sharp interface with the lesion but merges gradually with surrounding normal bone. Pyogenic vertebral osteomyelitis occurs in elderly adults with genitourinary tract infections, patients who are immunocompromised, and intravenous drug abusers. Organisms from genitourinary tract infections ascend the vertebral column by way of the vertebral plexus of Batson, a valveless, venous bed that allows retrograde blood flow. The initial site of infection is the subcortial bone of the vertebral body adjacent to the intervertebral disk. The infection typically extends through the endplate, involving the disk and the adjacent vertebral body. Multiple levels of involvement are not uncommon, and the levels may be contiguous or noncontiguous. Lateral extension causes a paraspinal abscess; posterior extension can result in epidural abscess, cord compression, and meningitis. The radiographic finding is disk space narrowing with destruction of the facing vertebral endplates. As the process evolves, increasing reactive bone production and sclerosis occur in the affected vertebral bodies on both sides of the involved disk space, often making it appear widened (Figs. 16.10–16.12). Bony ankylosis is one eventual outcome of this process. Paravertebral soft-tissue swelling may indicate extension into the soft tissues. CT and MRI can delineate the anatomic extent of involvement. FIGURE 16.10. Vertebral discitis and osteomyelitis with destruction of the adjacent inferior and superior endplates (arrow). FIGURE 16.11. Lumbar vertebral discitis. A: Sagittal inversion recovery MRI shows fluid at the L4–5 disk space (arrow) and edema of adjacent vertebral body endplates. B: Sagittal T1-weighted fat-suppressed post-gadolinium MRI shows enhancement (arrow) around the L4–5 disk space. FIGURE 16.12. Vertebral discitis, osteomyelitis, and epidural abscess. A: Sagittal T1-weighted MRI shows infection of the C6–7 level with epidural mass (arrow). B: Sagittal T1-weighted gadolinium-enhanced MRI shows an enhancing inflammatory mass with a low signal in the center. C: Axial CT scan at C6 shows vertebral body destruction. Tuberculosis is becoming more common in North America but is usually associated with immunocompromised patients or immigrant populations. Musculoskeletal disease is the result of hematogenous spread, typically from the lungs. Perhaps half of all cases of musculoskeletal tuberculosis affect the spine. The body of L1 is the site most commonly affected, but involvement of multiple contiguous levels is frequent, and involvement of the cervical and thoracic region, posterior elements, and SI joints is known to occur. The infection usually begins in the anterior aspect of the vertebral body at an endplate. Infection may spread by extending into the disk space, along the subligamentous space, or into the paraspinal soft tissues (Fig. 16.13). Paravertebral psoas abscesses may burrow into the groin or thigh. FIGURE 16.13. TB spondylitis. A: Radiograph at presentation shows loss of height at the L3–4 disk level and early inferior endplate destruction at L3 (arrow). B: CT shows bone destruction and paraspinal inflammation. C: Axial T2-weighted MRI shows paraspinal inflammatory mass (short arrow) with left psoas muscle abscess (long arrow). D: Radiograph after 1 month shows further destruction of L3.
Infection and Marrow Disease
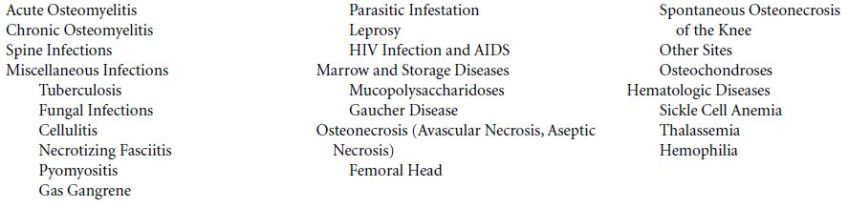
 ACUTE OSTEOMYELITIS
ACUTE OSTEOMYELITIS



 CHRONIC OSTEOMYELITIS
CHRONIC OSTEOMYELITIS


 SPINE INFECTIONS
SPINE INFECTIONS




 MISCELLANEOUS INFECTIONS
MISCELLANEOUS INFECTIONS
Tuberculosis

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree