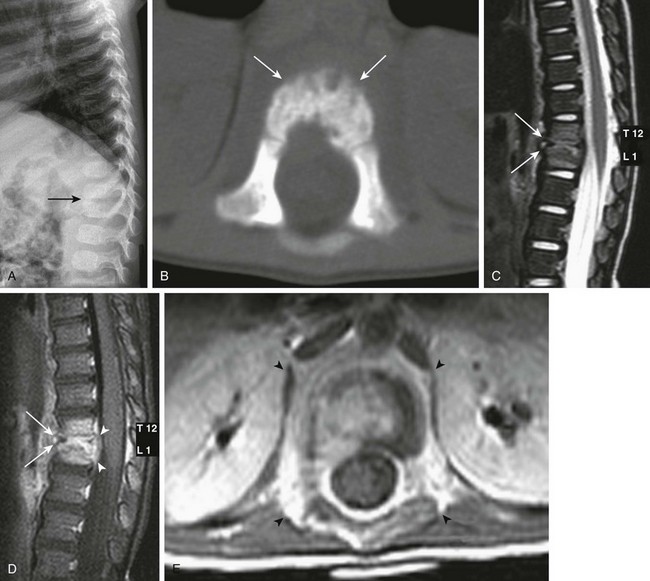
Chapter 44 Spinal infections in children are uncommon. Etiologies include direct and indirect (hematogenous) inoculation by bacterial, viral, parasitic, and fungal agents. Direct bacterial infectious inoculation may occur as a result of trauma, instrumentation, or via a preexisting congenital sinus tract or area of spinal dysraphism (i.e., a meningocele). In recent years, Lyme disease (Fig. 44-1) caused by a Borrelia burgdorferi infected tick bite has emerged as a cause of spinal cord infection, especially in the Northeastern United States. Mosquito-borne West Nile virus (Fig. 44-2), with cases initially appearing along the east coast of the United States, has since been discovered nationwide and also has emerged as a more recent spinal cord infectious agent. Tuberculosis (TB) of the spinal cord usually occurs in the thoracic region in children (Fig. 44-3) and manifests as an intramedullary tuberculoma, most often seen in patients with acquired immunodeficiency syndrome or other types of immunocompromise. TB is most prevalent in India, but it is also widespread in Africa and in Southeast Asia. Cysticercosis (Fig. 44-4) is the most common parasitic infection encountered within the spinal cord. It occurs after ingestion of uncooked pork infected with Taenia solium and is most prevalent in South America and Southeast Asia. Gnathostomiasis (Fig. 44-5) is caused by the nematode Gnathostoma spinigerum, which is acquired by ingesting contaminated fish or meat and presents clinically with myeloradiculitis. It is endemic in Southeast Asia and virtually unknown in North America, other than in persons with infections that are acquired abroad. Figure 44-1 An adult who was bitten by a tick and infected with Lyme disease. Figure 44-2 An adult patient who was bitten by a mosquito and infected with West Nile virus. Figure 44-3 An adult patient with tuberculosis exposure. Figure 44-4 A 20-year-old man who presented with paraparesis that developed over a few weeks was found to have cysticercosis. Figure 44-5 A 17-year-old boy from Thailand with gnathostomiasis. Disc space infection often coexists with vertebral osteomyelitis in children as a result of hematogenous spread through capillary tufts in vertebral body endplates and vascular channels of immature intervertebral disc spaces. Contrast-enhanced MRI is the study of choice and should be performed without delay in suspected cases (Fig. 44-6). Although infection can occur at any level, the midlumbar spine is most often affected. Staphylococcus aureus represents the most common etiologic organism. Worldwide, organisms such as TB are not uncommon etiologies. The first radiographic sign of infection is irregularity of the vertebral body endplates. The affected disc space is usually narrowed and demonstrates low signal intensity on T2-weighted MR sequences. Edema and postcontrast enhancement in adjacent vertebral body endplates indicate the presence of associated osteomyelitis and possible disc space abscess. Complicated cases demonstrate epidural and paravertebral abscess or phlegmon, which are well elucidated by MRI. Signs of late infection include vertebral body collapse and spinal deformity (Fig. 44-7). After treatment, vertebral body and disc space findings may persist for up to 24 and 34 months, respectively. Chronic recurrent multifocal osteomyelitis is the most severe form of chronic nonbacterial osteomyelitis and is of uncertain etiology. Although chronic recurrent multifocal osteomyelitis most commonly affects the metaphyses of long bones and the medial clavicles, vertebral column and pelvic involvement can occur.
Infections of the Spine and Spinal Cord
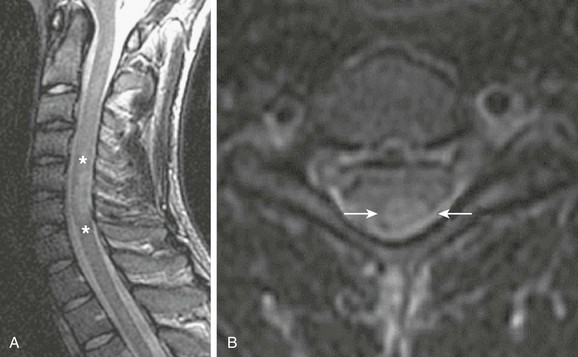
Sagittal (A) and axial (B) T2-weighted images of the cervical spine demonstrate T2 prolongation (asterisks in A and arrows in B) within the dorsal spinal cord at the level of C5/C6 as a result of demyelination. (Case courtesy Gul Moonis, MD, Beth Israel Deaconess Medical Center, Division of Neuroradiology.)
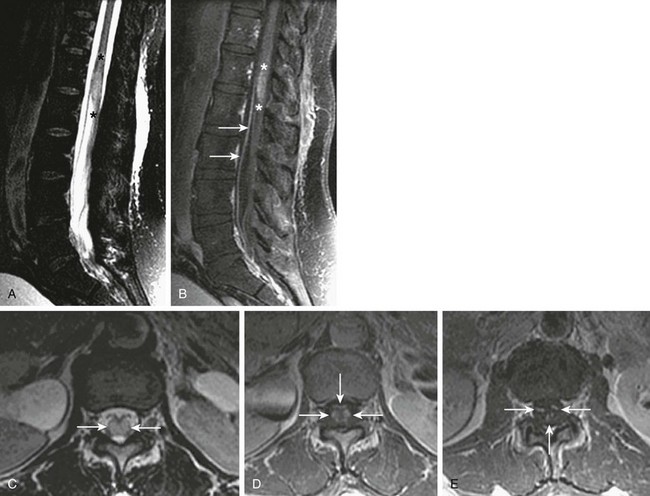
Sagittal and axial T2-weighted images (A and C, respectively), and sagittal (B) and axial (D and E) postgadolinium T1-weighted images of the lumbar spine demonstrate T2 prolongation (A, asterisks, and C, arrows) within the distal spinal cord/conus medullaris, as well as contrast enhancement of the distal cord (B, asterisks)/conus medullaris (D, arrows) and within the cauda equina (E, arrows) as a result of viral myeloradiculitis. (Case courtesy Gul Moonis, MD, Beth Israel Deaconess Medical Center, Division of Neuroradiology.)
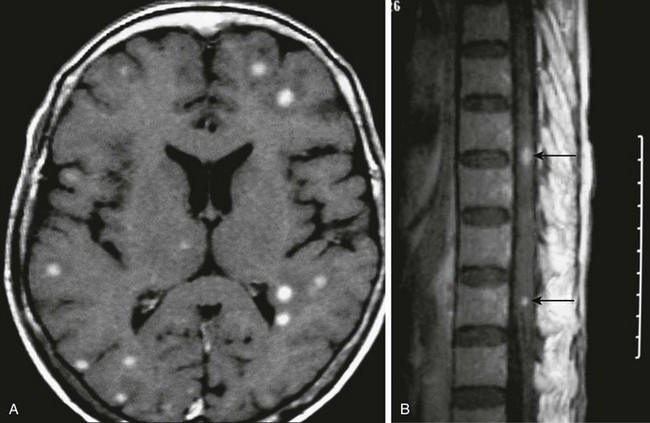
Axial postcontrast T1-weighted magnetic resonance imaging of the brain (A) and thoracic spine (B) demonstrate multiple enhancing intraaxial nodules corresponding to tuberculomas (arrows in B). (Case courtesy Drs. Pranjal Goswami, Nirod Medhi, and Pratul Kr. Sarma of Primus Institute in Guwahati, India.)
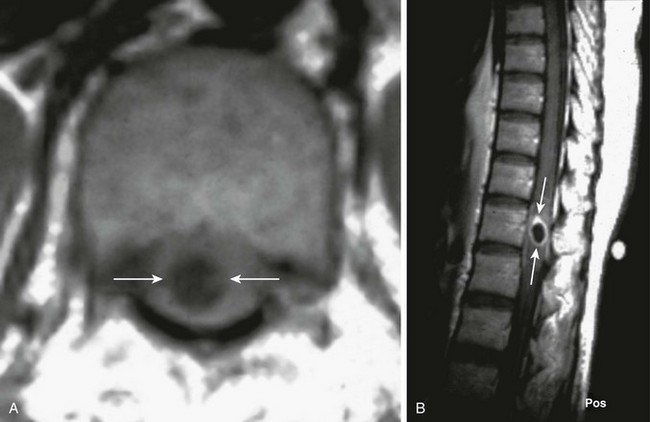
An axial T1-weighted image (A) and a sagittal postcontrast T1-weighted image (B) of the thoracic spine demonstrate central T1 prolongation within the spinal cord proper (arrows in A), with corresponding rim enhancement on the postcontrast image (arrows in B). (Case courtesy Dr. Manu Shroff of the Hospital for Sick Children in Toronto, Canada.)

Sagittal (A) and axial (B) postcontrast T1-weighted images of the thoracic spine demonstrate enhancing nodules (arrows in A and B) within the spinal cord proper as a result of a parasitic infection. (Case courtesy Dr. Jiraporn Laothamatas of Mahidol University, Bangkok, Thailand.)
Discitis and Osteomyelitis
Infections of the Spine and Spinal Cord