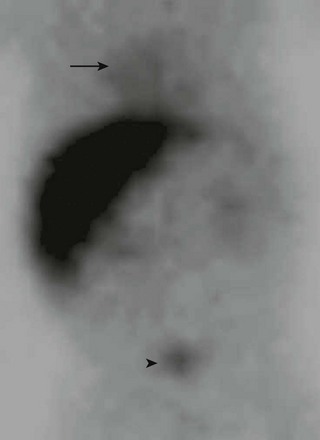
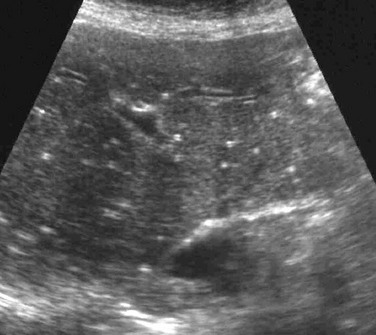
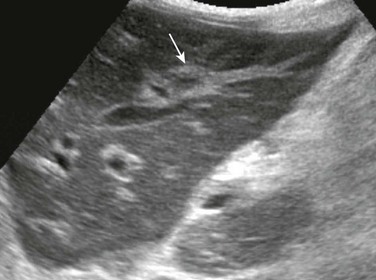
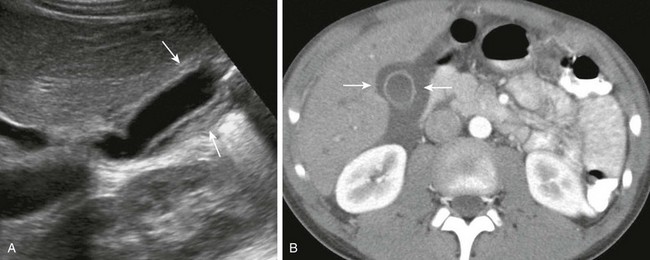
Chapter 91 Viral hepatitis is the most common diffuse infection of the liver in otherwise healthy children.1 Although parasites are more common worldwide, they typically involve the biliary tree, as in ascariasis, or produce focal infections of the liver, as in echinococcosis or amebiasis. In immunocompromised patients, other infections, particularly fungal infections, become more common. Overview: Viral hepatitis presents a spectrum of clinical severity, which can range from subclinical infections to fulminant hepatitis or progression into cirrhosis. Etiology: Beyond the neonatal period, viral hepatitis is most commonly caused by the hepatitis A, hepatitis B, and hepatitis C viruses.1 A number of other viruses have been implicated in childhood hepatitis, including mumps, measles, varicella-zoster, herpes simplex, cytomegalovirus, adenovirus, Coxsackie virus, and Epstein-Barr virus. Most affected patients have a short-lived acute disease with complete recovery. Complications include subacute and chronic active hepatitis, evolution into cirrhosis, and development of hepatocellular carcinoma.2 Imaging: Diagnosis is made clinically and on the basis of laboratory data. If imaging is performed during the acute phase of the illness, the liver may be enlarged or normal in size. Sonography of the affected liver may demonstrate increased parenchymal echogenicity and heterogeneity.3 Increased thickness of the portal triads related to periportal edema may be seen (Fig. 91-1), which leads to the “starry sky” pattern, and the gallbladder wall can appear thickened.1,4–6 Lymphadenopathy may be present at the porta hepatis. Computed tomography (CT) scans sometimes show heterogeneous changes in attenuation, but more commonly they show hepatomegaly, gallbladder wall thickening, and periportal low attenuation (Fig. 91-2). In patients with fulminant hepatitis and subsequent hepatic regeneration, imaging differences have been described between necrotic areas and regenerating nodules. Regions of necrosis have central low attenuation on noncontrast CT relative to regions of regeneration. After intravenous (IV) administration of contrast material, areas of necrosis and regeneration may enhance similarly such that they become indistinguishable, or the regenerating nodules may show diminished enhancement, which can simulate a neoplastic lesion. Similarly, magnetic resonance imaging (MRI) may show nonspecific periportal high intensity on T2-weighted images and hepatomegaly.3 On MRI, areas of nodular regeneration show high signal on T1-weighted images and low signal on T2-weighted images relative to adjacent parenchyma.4 Figure 91-1 Periportal edema in a 12-year-old boy with viral hepatitis. Figure 91-2 Gallbladder wall thickening in a 10-year-old boy with viral hepatitis. Although it is used less frequently today than in the past, nuclear scintigraphy may be performed in infants suspected of having biliary atresia or hepatitis. Because liver function is decreased, there is poor uptake of the radiopharmaceutical agent with delayed excretion through the biliary tree into the small bowel and vicarious excretion through the kidneys (Fig. 91-3). Overview: Pyogenic infection with hepatic abscess formation is caused by microbial liver infection with subsequent inflammatory cell response and pus accumulation. The mortality rate is 6% to 14%.5 Immunocompromised patients with chronic granulomatous disease of childhood or those who have undergone bone marrow transplantation are at particularly high risk for liver abscesses. Other susceptible states include chemotherapy, congenital or acquired immunodeficiency, and intraabdominal infection, such as appendicitis and inflammatory bowel disease.2 Hepatic abscesses are most common in the right hepatic lobe, and most are solitary.6 Etiology: Staphylococci, streptococci, and Escherichia coli are the most common pathogens involved in a pyogenic abscess. However, Klebsiella pneumonia, which typically is more common in Asian countries, is increasing in incidence in North America.6,7 Imaging: Hepatic abscesses often have an insidious presentation, leading to a delay in diagnosis. They range from single, well-defined, homogeneous, circular foci to heterogeneous, poorly defined, multiloculated, septated, debris- or gas-containing lesions (Fig. 91-4). Air-fluid levels may be related to gas-forming organisms. Enhanced through-transmission in a hypoechoic mass on ultrasound and lack of central flow with Doppler are useful in confirming a cystic, rather than a solid, lesion.2 Other sonographic findings in persons with a pyogenic liver abscess include a hypoechoic or anechoic mass, a hypoechoic surrounding ring of edema, internal fluid-debris levels, and septations. Common CT findings include lack of central enhancement after contrast administration, an enhancing abscess wall, and a surrounding rim of low-attenuation hepatic edema.2,8 Abscesses in patients with chronic granulomatous disease may heal with formation of granulomas, which frequently calcify. MRI of hepatic abscesses typically show decreased or nearly isointense signal on T1-weighted images, increased signal on T2-weighted images, and peripheral ringlike contrast enhancement.8 Multiple abscesses are most commonly the result of biliary disease, biliary obstruction, or hepatic trauma. Hematogenous spread of pyogenic organisms may result in multiple abscesses (Fig. 91-5). A tuberculous abscess cannot be differentiated on imaging studies from other pyogenic infections.9 Resolved tuberculosis may result in hepatic calcifications. Figure 91-4 Pyogenic abscess in a 2-month-old boy with fever. Treatment and Follow-up: Treatment of pyogenic abscesses ranges from antibiotics alone for small lesions (usually <5 cm) to percutaneous aspiration and catheter drainage for larger lesions. Percutaneous abscess drainage has markedly reduced case mortality from 40% to 2%.2,5,10 Because amebic abscesses are readily treated medically, serology or aspiration diagnosis of this entity can help avoid drain placement.11,12 The techniques used for percutaneous drainage in children are similar to those used for adults, although IV sedation or general anesthesia may be necessary.13 The rare complications that occur after percutaneous drainage include bleeding, peritonitis, and less often, septicemia, pneumothorax, and empyema.2 Surgical drainage is used only if catheter drainage fails or treatment of an underlying cause of abscess is required.11 Overview: Fungal infection occurs frequently in the setting of immune compromise, such as leukemia and chronic granulomatous disease; a reported increase in systemic fungal infection may be the result of longer survival of immunocompromised hosts.14,15 Etiology: The most common causative organism is Candida albicans, which may affect any organ system. However, other ubiquitous fungi such as Aspergillus, Histoplasma, Coccidioides immitis (in endemic areas), and opportnistic bacteria such as Nocardia have been identified in persons with immune compromise.14 Imaging: The imaging appearance depends on the host’s immune response. In neutropenic patients, disease is microscopic and lesions may be occult on imaging. Formation of microabscesses is possible when the patient recovers from neutropenia and mounts an immune response. On sonography, four imaging patterns of candidiasis within the liver are reported. All four patterns have multiple, small (<3 mm to 4 mm) lesions scattered diffusely throughout the liver parenchyma.16 Early in the disease process, the “wheel-within-a-wheel” appearance is seen, representing a hyperechoic nidus of necrotic fungus, surrounded by echogenic inflammatory cells, in turn surrounded by a peripheral zone of fibrosis. The bull’s-eye or target appearance, consisting of an echogenic center with a hypoechoic rim, is seen when the host mounts an immune response.2 The most common appearance is seen later and consists of diffuse uniform hypoechoic foci throughout the liver resulting from formation of tiny microabscesses (<4 mm) and fibrosis (Fig. 91-6). Last is the pattern of calcified, hyperechoic tiny foci in persons with a healed or healing fungal infection (1 to 4 mm) (Fig. 91-7).16,17 Findings on CT include multiple foci of low attenuation of variable size (2 to 20 mm), with or without enhancement and calcification.2,16 Arterial phase scans have been shown to be more sensitive for detection.18 MRI may reveal tiny lesions of low signal intensity on T1-weighted imaging and high signal intensity on T2-weighted imaging; T1-weighted gradient echo sequences have been reported to show greater sensitivity than the spin-echo sequence.19 However, the appearance remains relatively nonspecific compared with the more distinct patterns described on sonography.16 Figure 91-6 Hepatic candidiasis in a 7-month-old boy with immune deficiency. Overview: Cat scratch disease usually is a self-limited infection that most often involves the lymph nodes. In 5% to 10% of cases it spreads systemically to variably involve the liver, spleen, bone, and, rarely, the central nervous system with meningoencephalitis or neuroretinitis. Patients with acquired immunodeficiency syndrome may present with bacillary angiomatosis.20,21 Children usually present with painful lymphadenopathy; however, systemic spread may cause low-grade fever and various complaints related to involvement of virtually any organ system.20
Infectious Causes of Liver Disease
Viral Hepatitis
A longitudinal sonogram demonstrates increased perivascular echogenicity along the portal triads (arrow).
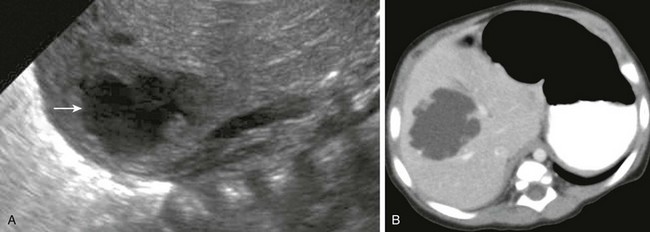
A, A longitudinal sonogram shows a thick, hyperechoic gallbladder wall (arrows). B, Computed tomography with intravenous contrast confirms gallbladder wall thickening (arrows) and periportal edema.
Pyogenic Abscess
A, A longitudinal sonogram of the right hepatic lobe reveals a hypoechoic region with irregular margins (arrow) and a halo of decreased parenchymal echogenicity. B, Axial contrast-enhanced computed tomography image confirms the low attenuation region. Staphylococcus was found upon subsequent percutaneous needle aspiration.
Fungal Infections

A longitudinal sonogram shows diffuse, homogeneous, hypoechoic foci consistent with microabscesses throughout the liver. A tiny amount of fluid in the Morrison pouch is noted (arrow) adjacent to the right kidney.
Cat Scratch Disease
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree