CHAPTER 12 This chapter covers those clinical forms of arthritis and connective tissue disease that present on radiographs with a preponderance of inflammatory changes. Rheumatoid arthritis is a systemic autoimmune disease manifested in the musculoskeletal system by inflammatory polyarthritis of the small synovial joints. The pathogenesis is not understood, and no causative agent has been proved. Genetic factors affect susceptibility to and expression of the disease. Rheumatoid arthritis is usually distinguished from other arthritides by the presence of rheumatoid factor (RF) in the serum (see Chapter 11). Rheumatoid arthritis has a prevalence of 1% in the general population, with women affected more often than men by a 3:1 ratio. High RF titers often correlate with more severe disease. The typical age range of presentation is 25 to 55 years. In 70% of cases, the onset is insidious and occurs over weeks to months; in 20%, the onset occurs over days to weeks; and in 10%, the onset is acute and occurs over hours to days. The acute onset mimics the onset of septic arthritis. The clinical course of rheumatoid arthritis is progressive in 70% of cases, leading to disabling, destructive disease. The clinical progression may be rapid or slow. In 20%, the disease is intermittent with remissions generally lasting longer than exacerbations, and in 10%, remissions last several years. The clinical diagnosis is based on criteria that include morning stiffness, symmetric swelling of the proximal interphalangeal (PIP) joint, metacarpophalangeal (MCP) or wrist joints, rheumatoid nodules, serum RF, and specific radiographic findings. The underlying pathologic change in rheumatoid arthritis is chronic synovial inflammation with hyperemia, edema, and production of excess fluid. Chronicity leads to hypertrophy and fibrosis. Hypertrophic, chronically inflamed synovium is called pannus. Pannus dissolves the cartilage and bone by the actions of enzymes along its advancing margin. Commonly seen early radiographic findings include fusiform periarticular soft-tissue swelling—corresponding to synovial hypertrophy and joint effusion—and acute erosions at the margins of the joint. Articular cartilage may also be dissolved by enzymes released into the joint space, causing uniform narrowing of the joint space on radiographs. Synovial hyperemia causes juxta-articular osteoporosis. There is a characteristic lack of reactive bone formation. Common late radiologic findings include chronic generalized osteoporosis, progression of marginal erosions to severe erosions involving subchondral bone, synovial cyst formation, subluxations and abnormalities of alignment, and secondary osteoarthritis. Not all findings are present at any one time in individual patients; observation of combinations of these findings should lead to the correct diagnosis. The distinctive radiographic pattern of chronic osteoporosis, marginal erosions, and little if any reactive bone formation is the hallmark of rheumatoid arthritis. Although the appendicular skeleton tends to be extensively involved, the axial skeleton is usually spared except for the upper cervical spine. Bilaterally symmetric clinical involvement is usual, but the severity of radiologic involvement is not necessarily symmetric, especially when radiographs are obtained early in the clinical course. Secondary degenerative changes may occur if the inflammatory process remits for several years. Both rheumatoid arthritis and primary osteoarthritis are common conditions; patients with both diseases may have confusing radiographic findings. Sonography and MRI are more sensitive than radiography in detecting synovitis, the primary abnormality in rheumatoid arthritis. Subchondral bone marrow edema may occur with synovitis, and both are precursors of bone erosions. Erosions will not occur in the absence of synovitis. MRI criteria for diagnosing rheumatoid arthritis include periarticular contrast enhancement of the wrist or the MCP or PIP joints in both hands, marrow edema, erosions, joint effusion, synovial sheath effusion, and cartilage irregularity and thinning. Gadolinium helps distinguish nonenhancing joint fluid from enhancing synovial proliferation and pannus. Successful treatment of early rheumatoid arthritis with disease-modifying antirheumatic drugs that suppress synovitis may be evident on MRI as the reversion of synovitis and marrow edema to normal. MRI is also helpful in the evaluation of the complications of rheumatoid arthritis at the craniocervical junction and elsewhere. There is considerable variability in the distribution of radiographic abnormalities in rheumatoid arthritis, and the findings on radiographs may not correlate with the clinical features. The earliest radiographic changes are fusiform soft-tissue swelling and juxta- articular osteoporosis (Figs. 12.1 and 12.2). In the hand, rheumatoid arthritis classically involves the MCP and PIP joints. The earliest bone erosions are generally at the MCP joints (Fig. 12.3), often the second and third on the radial side. The PIP joint of the middle finger is another site of typical early involvement. Oblique radiographs may show subtle subchondral bone resorption. Fusiform soft-tissue swelling, juxta-articular osteoporosis, concentric loss of cartilage space, and acute marginal erosions may be seen (Fig. 12.4). Compressive erosions and remodeling of bone may result from the collapse of osteoporotic bone by muscle tension; this is especially common at the MCP joints. Loss of the normal balanced tension at the digits results in various alignment deformities, including the swan neck and boutonniere deformities of the fingers (see Fig. 11.15) and the Z-shaped deformity of the thumb (Fig. 12.5). Superficial erosions of the cortex may occur beneath the inflamed tendon sheaths, especially along the outer aspect of the distal ulna, the dorsal aspect of the first metacarpal, and the proximal phalanx of the first digit. FIGURE 12.1. Rheumatoid hand. A boutonniere deformity is present at the middle finger. Erosions are present at the PIP joint of the middle finger (short arrow) and the MCP joints of the index, ring, and little fingers (arrowheads). Fusiform soft tissue swelling is present at the PIP joint of the ring finger (long arrow). FIGURE 12.2. Rheumatoid arthritis with early erosive changes at the MCP joints. FIGURE 12.3. Rheumatoid arthritis involving the MCP joint of the ring finger. A: Radiograph shows early subchondral bone erosion (arrow). B: Coronal T2-weighted fat-suppressed MRI shows effusion (arrow). C: Coronal T1-weighted fat-suppressed MRI following gadolinium injection shows enhancement (arrow). FIGURE 12.4. Rheumatoid arthritis with juxta-articular osteoporosis. FIGURE 12.5. Hand deformities in rheumatoid arthritis. PA radiograph shows boutonniere deformity of the ring finger, Z-shaped deformity of the thumb, proximal dislocation of the first CMC joint, volar dislocation of the MCP joint of the little finger, and ulnar translocation of the carpus. In the wrist, pancompartmental involvement is usual (Fig. 12.6). The earliest bone changes are erosions at the ulnar and radial styloid processes and at the waists of the capitate and scaphoid bones. On MRI, erosions are evident as focal defects in the bone that are low to intermediate signal on T1-weighted images and high signal on T2-weighted images (Fig. 12.7). On T1-weighted images after gadolinium enhancement, the pannus within the erosions enhances. Malalignment in advanced disease results from loss of balanced muscular tension and ligamentous restriction. Involvement of tendons can be demonstrated by MRI (Fig. 12.8). On T2- weighted images, synovial sheaths show fluid and high signal. On T1-weighted images after the gadolinium injection, the inflamed synovium shows enhancement. The posttraumatic ligamentous instability patterns of the wrist described in Chapter 2 are often seen in advanced rheumatoid arthritis. FIGURE 12.6. Rheumatoid wrist. A: Early findings include juxta-articular osteoporosis and subtle erosions, including the scaphoid waist (arrow). B: The same patient 6 years later has severe erosions and subluxations. Ulnar translocation is present. The bones are diffusely osteoporotic, with no proliferative changes. The scaphoid waist erosion has become large (arrow). FIGURE 12.7. Rheumatoid arthritis involving the carpal bones. A: Coronal T1-weighted MRI shows erosions. B: Coronal T1-weighted fat-suppressed MRI following gadolinium injection shows enhancement in the erosions, corresponding to inflammatory pannus. FIGURE 12.8. Rheumatoid arthritis of left ankle with tenosynovitis. Axial T1-weighted fat-suppressed MRI following gadolinium administration shows thickened synovium with intense uptake (arrowhead). Effusion (e) is noted in the anterior ankle, and longitudinal split tears of the posterior tibialis tendon (white arrow) and peroneus brevis tendon (black arrows) are noted. In the elbow, synovial hypertrophy and effusion provide a fat pad sign. As in other joints, periarticular osteoporosis, uniform joint space narrowing, and erosions are seen. In the glenohumeral joint, erosions are especially prominent around the proximal humerus, and rotator cuff tear or atrophy causes superior subluxation of the humeral head and adaptive changes in the inferior surface of the acromion from the humeral head (Figs. 12.9 and 12.10). Resorption of the distal clavicle and widening of the acromioclavicular joint are frequently observed in rheumatoid arthritis. In the knee, meniscal invasion by pannus occurs early and may be detectable on MRI. Typical inflammatory changes may be superimposed on secondary degenerative changes, but the proliferative bone response is disproportionately modest in comparison to the loss of joint space (Fig. 12.11). On MRI, effusions, erosions, diffuse cartilage loss, bone marrow edema, and pannus may be demonstrated at the knee (Fig. 12.12). The hip is less frequently involved than the knee. Concentric uniform loss of joint space with axial migration is usual, but superior migration similar to that in osteoarthritis may also occur. Acetabular protrusion (protrusio acetabuli), fibrous ankylosis, subchondral cysts, erosions, and secondary reparative and degenerative changes are common. If steroids are administered, osteonecrosis of the femoral head is a potential complication. In the foot, changes may be seen early at the metatarsophalangeal (MTP) and interphalangeal (IP) joints of the great toe (Fig. 12.13). Although the usual changes of rheumatoid arthritis that are found elsewhere in the skeleton may be present in the foot, erosions tend to be small and infrequent. Soft-tissue involvement may lead to hallux valgus and planovalgus deformity of the foot. In the heel, retrocalcaneal bursitis, Achilles tendonitis, and plantar fasciitis may cause swelling and calcaneal erosions (Fig. 12.14). Spontaneous Achilles tendon rupture may occur. FIGURE 12.9. Radiograph of the shoulder in advanced rheumatoid arthritis shows osteopenia, erosion of the distal clavicle, and remodeling of the undersurface of the acromion and medial humeral shaft. FIGURE 12.10. Rheumatoid shoulder with osteoporotic bones and secondary glenohumeral degenerative change. The distal clavicle is eroded and remodeled. FIGURE 12.11. Rheumatoid knees. The bones are osteoporotic. Uniform joint space loss is present with minimal proliferative bone changes. Some secondary osteoarthritic changes are present in the lateral compartment of the left knee. FIGURE 12.12. Rheumatoid knee. A: Sagittal T2-weighted fat-suppressed MRI shows large effusion and Baker cyst with synovial thickening (arrows). Diffuse cartilage loss and subchondral edema are present. B: Coronal T1-weighted fat-suppressed MRI following gadolinium shows synovial and subchondral enhancement. FIGURE 12.13. Rheumatoid foot. The great toe is deviated laterally, and the remaining MTP joints are subluxated. Erosions are present at all of the MTP joints and the IP joint of the great toe; the other joints appear spared. Some erosions appear sclerotic, suggesting clinical quiescence. FIGURE 12.14. Rheumatoid arthritis. Swelling of the retrocalcaneal soft tissues is present with a large erosion in the adjacent bone (arrow). In the spine, the upper cervical spine is the only common site of involvement. As many as 70% of patients with rheumatoid arthritis are affected symptomatically at some time, and up to 85% of those with classic rheumatoid arthritis have radiographic changes at the upper cervical spine. The atlantoaxial articulation (C1–2) has a synovial joint anteriorly where the odontoid process articulates with the anterior arch of C1 and is stabilized posteriorly by the transverse ligament. A bursa is interposed between the odontoid process and the transverse ligament. Synovitis at these sites may cause erosions of the odontoid process and rupture of the transverse ligament (Figs. 12.15 and 12.16), resulting in a widened predental interval. One consequence is atlantoaxial instability, with imminent danger of quadriplegia or death. Below the level of C2, the cervical spine may be diffusely involved by joint space narrowing. Inflammatory pannus at the synovial uncovertebral joints (joints of Luschka) may extend into the intervertebral disks. The thoracic spine and lumbar spine are usually spared. Sacroiliac (SI) joint involvement is infrequent and, when present, is mild and asymmetric. FIGURE 12.15. Rheumatoid arthritis. Atlantoaxial subluxation is present with a wide gap between the anterior arch of C1 and the odontoid process (arrow). FIGURE 12.16. Rheumatoid arthritis. Sagittal T2-weighted MRI shows pannus (arrow) eroding the odontoid process and causing mass effect on the spinal cord. Extra-articular manifestations of rheumatoid arthritis include rheumatoid nodules, development of cutaneous fistulas, infections, hematologic abnormalities, vasculitis, renal disease, pulmonary disease, and cardiac complications. Systemic lupus erythematosus (SLE) is a chronic systemic disease, the pathogenesis of which is related to immune complex deposition. It is more common in women by an 8:1 ratio, and there is a component of genetic susceptibility. The fluorescent ANA test is virtually always positive at the onset of clinical disease. Manifestations in the musculoskeletal system are common and may precede other systemic manifestations by months or years. Nonerosive symmetric polyarthritis with a distribution similar to that of rheumatoid arthritis is present in 75% to 90% of patients with SLE. Early findings on radiographs are fusiform soft-tissue swelling and juxta-articular osteoporosis, but there should be no joint space narrowing or erosions. A deforming nonerosive arthropathy is also common in SLE. The hands are typically involved at the MCP and IP joints (Figs. 12.17 and 12.18). Thumb, wrist, and foot involvement are more common than shoulder and knee involvement, and 10% of patients may develop atlantoaxial subluxation. These deformities are initially reducible, and radiographs may be normal. Fixed deformities and secondary degenerative changes may develop with time. Osteonecrosis may involve the femoral head, femoral condyle, humeral head, and other sites, and commonly has a symmetric distribution. Myositis, tendon weakening and spontaneous rupture, and soft-tissue calcification are other musculoskeletal manifestations. FIGURE 12.17. Systemic lupus erythematosus with alignment deformities. A, B: Lateral and PA radiographs show swan neck deformities of the ring and little fingers, with PIP hyperextension of the middle finger.
Inflammatory Arthritis
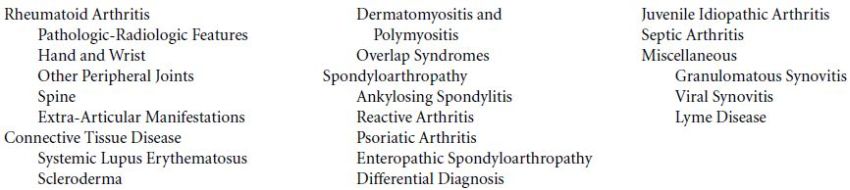
 RHEUMATOID ARTHRITIS
RHEUMATOID ARTHRITIS
Pathologic-Radiologic Features
Hand and Wrist










Other Peripheral Joints





Spine

Extra-Articular Manifestations
 CONNECTIVE TISSUE DISEASE
CONNECTIVE TISSUE DISEASE
Systemic Lupus Erythematosus


Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree