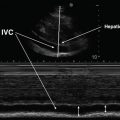
Fig. 13.1
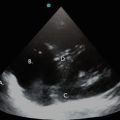
Color Doppler is used to distinguish the superficial (a) and deep (b) femoral arteries from the common femoral vein (c)
In situations where PE is a major concern, identification of a DVT allows the clinician to institute immediate anticoagulant therapy. However, caution must be exercised when no DVT is identified as up to 40 % of patients with a PE do not have a DVT [14]. Additionally, it is important to remember that the diagnosis of PE cannot be made explicitly with ultrasound. The utility of bedside echocardiography in the evaluation of PE augments clinical suspicion in hemodynamically unstable patients who cannot safely undergo a definitive test. Thus, ultrasonographic testing for PE is most helpful when typical findings of RV strain are absent, so that massive PE can be ruled out as part of a differential for shock of unknown etiology. Conversely, when submassive or massive PE is suspected in someone already known to have VTE, the presence of RV strain confers higher mortality.
Limited bedside echo performed to evaluate for signs consistent with PE is done using a phased-array, 2–4 MHz probe. The standard echo views are the parasternal long, parasternal short, subcostal long, and apical four-chamber. These views are easiest to obtain with the patient lying on the left side; however, this positioning is often not feasible for critically ill patients who cannot follow commands. Thus, these views are frequently obtained with the patient lying supine.
Image Acquisition and Interpretation
Sonographic diagnosis of a DVT is made by visualizing echogenic material within the lumen of a vein and/or by identifying a non-compressible venous segment. Determination of venous compressibility (visualizing complete collapse of the vessel lumen when adequate pressure is applied) or incompressibility (absence of venous collapse with adequate pressure) is the most reliable diagnostic sign when determining the presence or absence of a DVT [13]. Pressure is considered adequate when the walls of the adjacent artery become mildly deformed when attempting to compress the vein.
Lower Extremity
Examination of the LE venous system begins proximally at the common femoral vein and ends distally at the trifurcation of the popliteal vein, covering the entire proximal deep vein system. Vessels should be compressed every 1–2 cm between these two points while traveling down the leg. For symptomatic patients, a shorter exam with compression at only two separate points (the common femoral and popliteal veins) is adequate to identify most DVTs (sensitivity: 100 %; specificity: 99 % [15]; PPV 94 % [16]). However, clear evidence to demonstrate the diagnostic accuracy of this shorter examination when screening for asymptomatic DVT is insufficient. One study consisting of 2,704 symptomatic and asymptomatic subjects who required LE ultrasounds found that approximately 20 % of DVTs were missed when using the shorter exam compared to standard testing [17]. It remains unclear if this high rate of missed DVT was due to the inclusion of asymptomatic patients. Given that the critically ill patient is often unable to communicate, and missing a DVT in this population can have devastating consequences, compressive ultrasonography of the entire proximal venous system of the lower limb is recommended.
Veins in the proximal deep venous system that should be visualized include the common femoral, greater saphenous, superficial and deep femoral and popliteal veins (Fig. 13.2). Of note, the misleadingly named superficial femoral vein is a part of the deep venous system, and thrombus identified in this vein must be treated. Moving from proximal to distal the external iliac artery and vein become the common femoral vessels, with the common femoral vein generally seen medial to the artery. Continuing distally, the greater saphenous vein enters the common femoral vein from the superficial plane. There is no artery accompanying the greater saphenous vein. After this junction, the common femoral vessels divide into the superficial and deep femoral vessels, with all four vessels visible in the transverse ultrasound plane (Fig. 13.3). The superficial femoral artery and vein then become the popliteal artery and vein. Even more distal examination reveals the trifurcation of the popliteal vein into the anterior tibial, posterior tibial and peroneal veins.
Fig. 13.2
Deep venous anatomy of the lower extremity
Fig. 13.3
Venous anatomy moving from proximal to distal lower extremity. (a) Typical relationship of the common femoral artery (CFA) and common femoral vein (CFV), in inguinal region. (b) Moving distally, the greater saphenous vein (GSV) enters the CFV medially. (c) Continuing down the leg, first the CFA bifurcates into the superficial femoral artery (SFA) and deep femoral artery (DFA). (d) After the artery bifurcates, the CFV bifurcates into the superficial femoral vein (SFV) and deep femoral vein (DFV)
Typically, the superficial greater saphenous vein traverses the medial aspect of the leg from ankle to proximal thigh, emptying into the common femoral vein near the inguinal ligament. Because thrombus in the greater saphenous vein has a high likelihood of extending into the common femoral vein, this vein should be carefully evaluated and considered part of the deep venous system [18].
Deep veins of the calf include the anterior tibial, posterior tibial, and peroneal veins; however, debate exists regarding the management of calf DVTs, since the risk of embolization or extension into the proximal system is variable [19]. Routine full examination of the calf is not considered a necessary component of the bedside examination. In moderate to high-risk patients who have a negative initial study for proximal DVT, repeat CUS at a one-week interval is recommended [20]. This allows evaluation for any missed DVT that might have extended from the less concerning distal region into the more dangerous proximal region.
Lower Extremity Image Acquisition and Interpretation
The LE should be exposed from the inguinal region to the popliteal fossa. The leg should be externally rotated and the knee slightly flexed (Fig. 13.4). On the rare occasion when a barrier, such as a dressing, is obscuring the ability to perform an ideal exam, consider removing the barrier and using a sterile probe cover to create a clean interface between the probe and the patient’s skin.


Fig. 13.4
Proper positioning of the lower extremity: the leg is externally rotated and flexed at the knee
A high-resolution ultrasound machine with grayscale imaging and a high-frequency 7–10-MHz linear probe are needed for the examination. Place the transducer just below the inguinal ligament, holding the transducer in a transverse orientation with the indicator pointing toward the operator’s left. The common femoral vein and artery should be immediately visible where the vein is typically more medial than the artery (Fig. 13.5). Apply downward pressure until the vein completely collapses to the extent that the walls touch each other. When adequate pressure is applied (demonstrated by visualizing simultaneous deformity of the artery with downward pressure) and the vessel lumen does not collapse or if echogenic material is noted within the vein, the study is diagnostic for a thrombus. If the walls of the vein are seen to completely collapse, pressure is released, and the probe is moved distally by 1–2 cm to find the junction of the greater saphenous vein with the common femoral vein. The greater saphenous vein will be seen entering the common femoral vein medially. When compressed, the lumen of both the greater saphenous and the common femoral veins should completely disappear (Fig. 13.6).
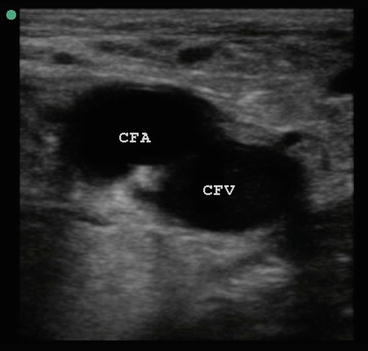
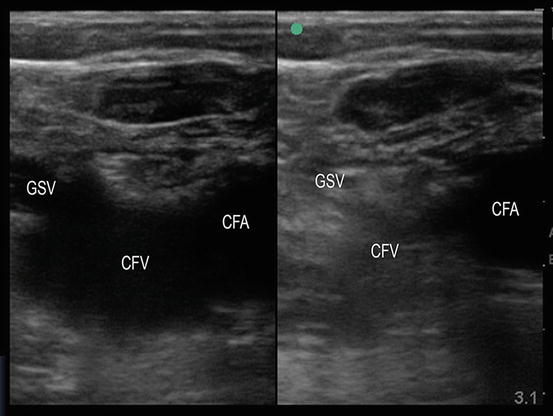
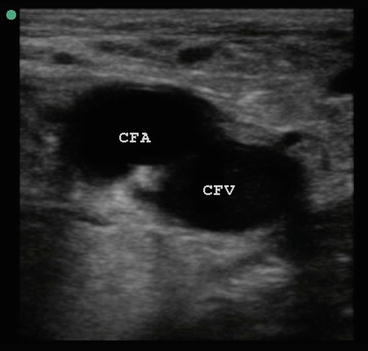
Fig. 13.5
Common femoral artery (CFA) and common femoral vein (CFV) with typical relationship of vein medial to artery in the groin region. Lateral designated by green dot in the left corner
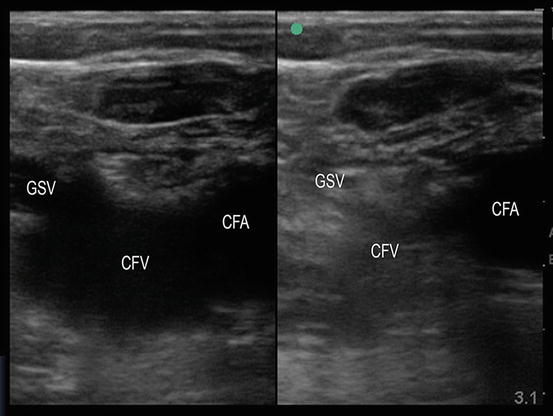
Fig. 13.6
Dual screen mode. Left: greater saphenous vein (GSV) enters the common femoral vein (CFV). Right: With compression, there is complete obliteration of the GSV and CFV lumen
After inspecting the greater saphenous vein, the next important landmark is the bifurcation of the common femoral artery into the superficial and deep femoral arteries, adjacent to the accompanying common femoral vein (Fig. 13.1). The common femoral vein then divides into the deep femoral and superficial femoral veins (Fig. 13.7). In this region distinguishing artery from vein may be difficult, especially with larger legs. Use of pulse wave and/or color Doppler is extremely helpful in distinguishing the superficial and deep arteries from the veins. Next, the superficial and deep femoral veins are evaluated in 1–2 cm segments until the deep femoral vein disappears, leaving the superficial femoral vein to be followed as distally as possible.
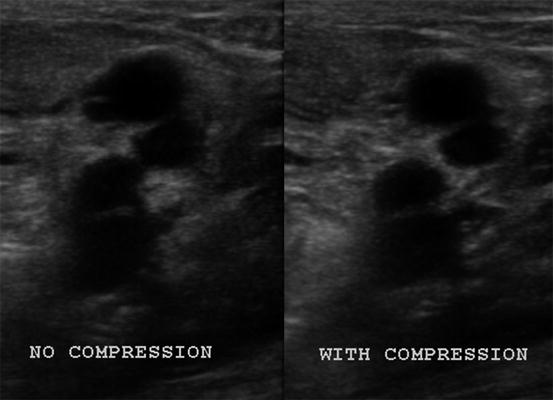
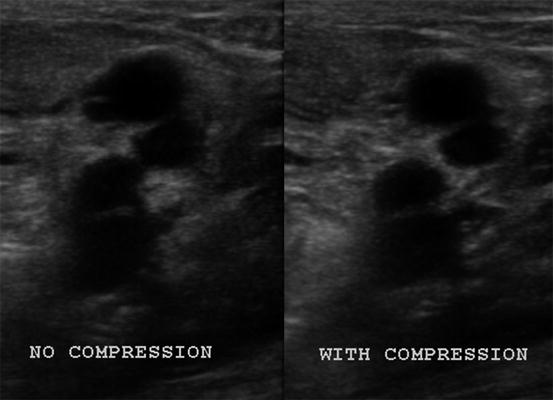
Fig. 13.7
Superficial femoral artery (SFA), superficial femoral vein (SFV), deep femoral artery (DFA), and deep femoral vein (DFV). With compression, none of the vessels collapse in this patient with a DVT in both the SFV and DFV
With the knee flexed 45°, place the transducer in the popliteal fossa to begin examination of the lower leg and popliteal region. After the popliteal artery and vein are identified, and compression of the vein is demonstrated (Fig. 13.8), move down the leg slightly until the veins just distal to the trifurcation of the popliteal vein are visualized and compressed. Though identification of a DVT in the calf veins (distal to the popliteal vein) does not mandate automatic treatment, knowledge of its presence warrants close follow-up with repeat CUS. The consideration to initiate full dose anticoagulation must be carefully weighed in high-risk ICU patients found to have a distal DVT [20].
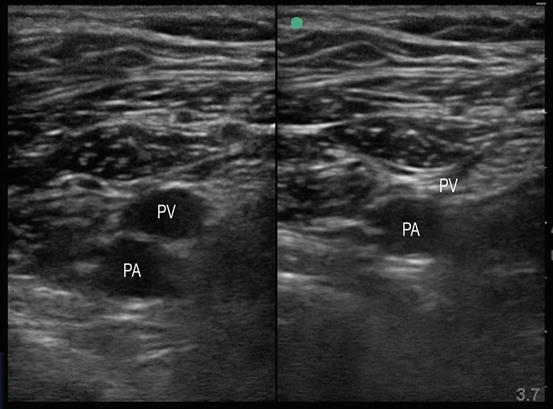
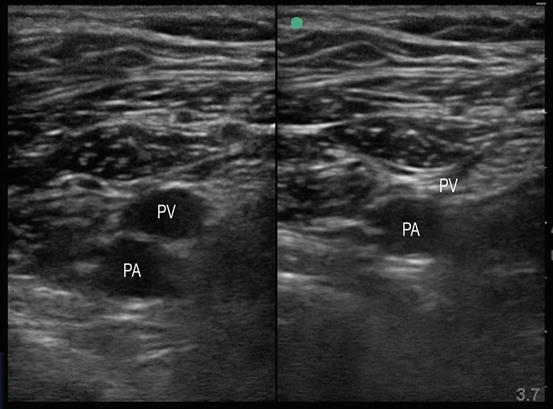
Fig. 13.8
Popliteal artery (PA) and popliteal vein (PV). Left screen shows no compression; right screen shows disappearance of lumen with compression
Once transverse imaging is complete, longitudinal views of the veins serve as a quick check and balance. Returning to the common femoral vein and rotating the ultrasound probe 90°, scan through the common femoral, superficial femoral, and popliteal veins in the longitudinal plane to ensure no intraluminal thrombus is seen. Just like with transverse views, compress the vessels with the probe to ensure that the vessels collapse completely. If thrombus was previously found in the transverse plane, the longitudinal view helps visualize the extent of intraluminal thrombus.
Augmentation can sometimes be used in difficult cases (e.g., morbid obesity or edema) to distinguish vasculature. This maneuver requires the application of color Doppler to the vein being visualized, then squeezing the leg at any area distal to the placement of the probe. Augmentation results in a rush of increased venous flow at the level of the probe. Theoretically, greater flow in the vessel rules out thrombus between the level of the vessel being visualized and where the leg is squeezed. However, augmentation does not provide additional meaningful information to the compression study [21] and 17–35 % of patients with DVT still show augmentation [22, 23]. For these reasons, augmentation is not a required part of the LE evaluation and should only be reserved for use when standard LE ultrasonography is inconclusive.
Upper Extremity
Upper extremity (UE) DVTs are not as rare or harmless as once thought. Though less common than LE DVT, they comprise between 10 % and 18 % of all DVTs and carry a risk of embolization, prompting current guidelines from the American College of Chest Physicians to recommend treatment of all proximal (axillary vein or higher) UE DVTs [24–26]. The incidence appears to be rising [27, 28], likely due to the association between UE DVTs and central venous catheters and an increased recognition that these DVTs are not benign. Because of frequent central venous catheterization, the critically ill population is particularly susceptible to UE DVT, and the possibility of an UE DVT must be given careful consideration in these patients.
The deep venous system of the UE begins with the radial and ulnar veins which meet in the antecubital fossa to become the brachial vein. This vein comprises of two vessels that travel on either side of the accompanying brachial artery throughout the upper arm. Continuing proximally, the basilic vein (a superficial vein) joins the brachial vein and forms the axillary vein; vessels proximal to and including the axillary vein encompass the proximal UE deep venous system. After passing under the clavicle the axillary vein becomes the subclavian vein, which joins the internal jugular (IJ) vein to become the brachiocephalic vein. Similar to the LE deep venous system, ultrasound examination of the UE system requires 1–2 cm compressions between the brachial and IJ veins.
Upper Extremity Image Acquisition and Interpretation
Starting in the supine position, identify the IJ in the transverse plane, sitting adjacent to the carotid artery. Evaluate the lumen of the IJ for visible thrombus, and perform compression. Typically, the IJ can be traced starting at the mastoid and progressing distally to its entry into the brachiocephalic vein. Since compression of the brachiocephalic is not possible because of the overlying clavicle, place color Doppler over the vein and watch for luminal filling from wall to wall. Pulse wave Doppler is then applied to look for presence of flow. Absence or reduction in flow is considered positive for the presence of a DVT. The subclavian vein is then found and traced toward the shoulder above the clavicle, but similar to the brachiocephalic vein, it is not compressible. Doppler interrogation with both pulse wave and color should be used throughout the course of the subclavian vein. Not only will pulse wave Doppler help to identify an area of the vein with clot, it will help to distinguish artery from vein in a confusing and difficult region. Small pulsations will be seen when pulse wave Doppler is applied to the vein, but these pulsations are generally less pronounced than in the artery. Further assisting in differentiation between artery and vein is the demonstration of respiratory variation with venous pulsations. Nearing the shoulder, the proximal portion of the axillary vein will also be obscured by the clavicle, therefore necessitating the continued use of Doppler interrogation of the vessel. Consider elevating and extending the arm outward to help engorge the veins if the distal subclavian and axillary veins are not visualized [29]. Once in the axilla, the brachial vein is compressible as it runs distally toward the antecubital fossa before splitting into the radial and ulnar veins. Throughout the UE examination, visible clot, a non-compressible segment, or lack of Doppler flow is diagnostic for a DVT.
Right Ventricular Evaluation
Limited echocardiography is used to risk-stratify a patient already diagnosed with PE or to determine whether PE might be causing shock. The basic four echocardiographic views to assess RV function are the subcostal long axis, parasternal long axis, parasternal short axis, and apical four-chamber views. On each of these views, the focus is on the RV to evaluate its function, appearance (dilation), and whether the interventricular septum intrudes into the left ventricle (LV), causing obstructive shock. Additionally, visible clot seen swirling in the RA or RV would further strengthen the case for an acute PE.
Right Ventricle Image Acquisition and Interpretation
A 2–4-MHz phased-array transducer is used to find four standard echocardiography windows: parasternal long axis, parasternal short axis, apical four-chamber, and subcostal long axis. Though all four windows should always be obtained, the most helpful windows are the parasternal short axis and the apical four-chamber. A good parasternal short view is generally created after successfully obtaining a clear parasternal long picture. The transducer is placed just to the left of the sternum in the 3rd–4th intercostal space, with the indicator facing toward the patient’s right shoulder. Once a clear parasternal long view is obtained showing the RV, LV, mitral valve, aortic outflow tract, and aortic valve (Fig. 13.9), the probe is then rotated 90° clockwise in the same position to produce the parasternal short axis view. This view provides a clear picture of the LV (typically round in appearance) with the RV seen to the top left of the image screen (Fig. 13.10). The transducer should be adjusted until the papillary muscles are clearly seen in the LV. The presence of RV strain is demonstrated by a dilated RV as it wraps around the LV. In cases where a PE is causing obstructive shock secondary to RV pressure overload, the septum between the RV and LV will be pushed into the LV lumen. The LV will then lose its round appearance and adapt a flattened shape, commonly referred to as a “D-shaped septum” (Fig. 13.11). The apical four-chamber view is obtained by sliding the probe laterally to the apex of the LV, at the point of maximum impulse, with the indicator facing the patient’s left side. This view shows the RA, RV, left atrium, and LV with the corresponding valves (Fig. 13.12). Knowing that the RV is normally approximately 60 % of the size of the LV, evidence of a large, dilated RV or an interventricular septum that pushes into the LV suggests hemodynamically significant PE in undifferentiated shock. This view also allows for evaluation of McConnell sign (normal apical movement with decreased RV free wall contractility) and for presence of abnormal echogenic densities within the RA or RV signifying the presence of clot. Absence of all of these findings makes PE an unlikely cause of shock.
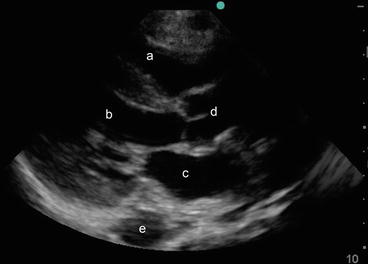
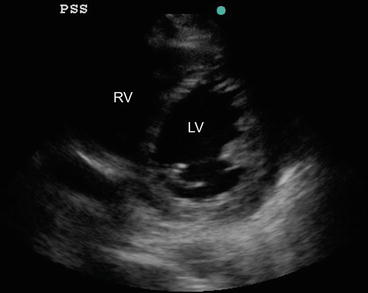
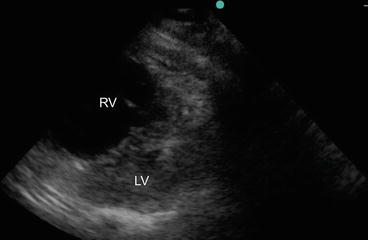
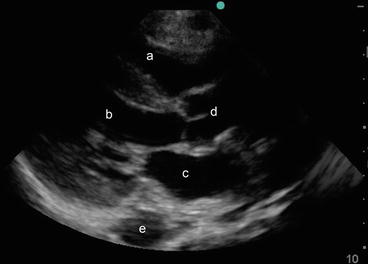
Fig. 13.9
Parasternal long axis view showing the right ventricle (a), left ventricle (b), left atrium (c), aortic valve and aortic outflow tract (d), and descending thoracic aorta (e)
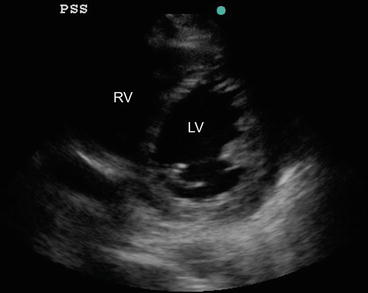
Fig. 13.10
Parasternal short axis view at the level of papillary muscles showing the right ventricle (RV) and circular left ventricle (LV)
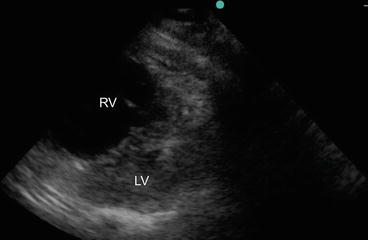
Fig. 13.11




Parasternal short axis view showing a large and dilated right ventricle (RV) with a flattened D-shaped septum and an almost obliterated left ventricle (LV) cavity during systole, due to pressure overload
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree