Fig. 21.1
Schematic diagram demonstrates the blood supply of the anterior abdominal wall. Note that the anastomosis between the deep superior epigastric artery (DSEA) and the deep inferior epigastric artery (DIEA) is situated in the segment of the rectus muscle above the umbilicus (From Taylor GI: Plast Reconstr Surg 81:721–724, 1988 [3])
Scheflan et al. [6, 7] divided the skin island of the flap into four zones, according to the reliability of its circulation and survival (Fig. 21.2). Zone 1 is located directly over the muscle and represents its primary cutaneous territory. Zone 2 is directly across the midline of the abdomen, which extends from the midline of the abdomen to the lateral edge of the contralateral muscle. Zone 2 of the skin island has proved reliable because the circulation is provided by the subdermal and deeper vascular communications of musculocutaneous perforating vessels from the rectus muscle beneath zone 1. Zone 3 is the portion of the skin island lateral to zone 1. Zone 4 is the most distant portion from zone 1 located between the lateral edge of the contralateral rectus sheath and the iliac crest. These two lateral zones, zone 3 and zone 4, are less reliable considering circulation based on one rectus abdominis muscle. In general, most of zone 4 and the lateral aspect of zone 3 are discarded because of inadequate perfusion. In addition the blood flow from the epigastric perforators through DSEA seems to be insufficient for the patients with obesity, heavy cigarette smoking, and advancing age to maintain the viability of the adipose mass of large TRAM flap [8]. Therefore, the microvascularly augmented TRAM flap, which is a superiorly based unipedicled TRAM flap with microvascular anastomosis between either the contralateral or ipsilateral inferior epigastric vascular system and available vessels close to the defect, is usually applied for the breast reconstruction in need of a large volume of soft tissue [9, 10]. Whichever procedure is applied, it is difficult to evaluate how much the circulation can be augmented to the flap.
Fig. 21.2
Vascular zones of the conventional pedicled TRAM flap (From Scheflan M, Dinner MI: Ann Plast Surg 10:120–129, 1983 [7])
21.3 Operative Procedures
21.3.1 Preoperative Markings and Preparations
Preoperative markings are completed at the standing position including the vertical midline from the suprasternal notch to the pubis passing through the umbilicus, the inframammary fold of the remaining breast, and its transferred line as a mirror image to the defect side (Fig. 21.3). The skin island of the TRAM flap is marked between the umbilicus and the pubic hair line extending between both anterior iliac spines at the spine position. In general, the superior margin of the skin island is located 1 or 2 cm superior to the umbilicus because of a large concentration of perforators to supply the overlying fat and skin around the umbilicus. We always use color Doppler sonography for the mapping of perforators. During surgery, the inferior margin of the skin island may be moved superiorly when direct closure appears difficult or too tight with retraction of the superior abdominal flap.
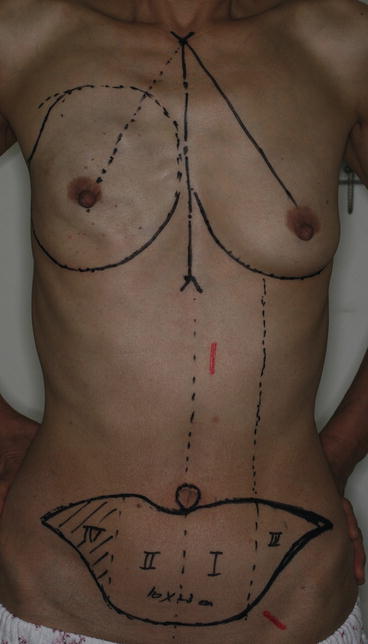
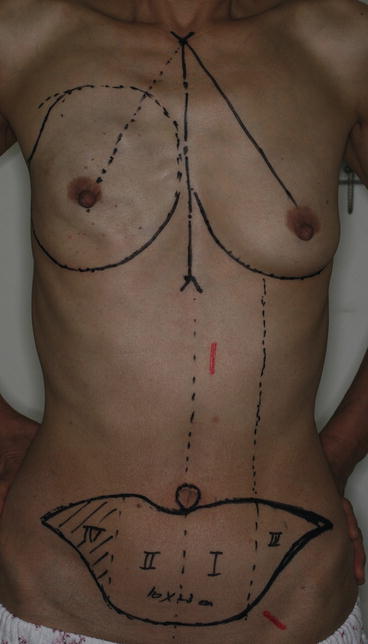
Fig. 21.3
Preoperative markings in the case of secondary breast reconstruction after skin-sparing mastectomy. The conventional pedicled TRAM flap is designed. The red lines indicate the location of superior epigastric artery and deep inferior epigastric artery. The shaded area indicates zone 4
21.3.2 Elevation of TRAM Flap
The procedure starts with the incision around the umbilicus to allow release of the umbilicus stalk to the midline fascia as described in the text [11]. The superior skin island incision is completed with a bevel of subcutaneous tissue superior to the skin incision to capture as many perforating vessels as possible and to add fatty tissue to the flap for the breast mound reconstruction. The superior abdominal skin and subcutaneous tissue are elevated from the abdominal fascia to the costal margin and to the sternum in the midline to transfer the pedicled TRAM flap through a generous tunnel into the breast area. After the abdominal flap elevation is completed, the superior-based abdominal flap is advanced toward the pubis to make sure that it covers the marked inferior incision for the TRAM skin island without tension. We usually use the contralateral TRAM flap in which the arc of rotation results in less twisting of the muscle below the skin island and in less disruption of the inframammary line. The ipsilateral side (zone 2 and zone 4) of the skin island is first elevated from external oblique and anterior sheath. After that a central strip of anterior rectus sheath is incised to expose the rectus muscle in the contralateral side (zone 1) of the skin island. The exposed muscle is dissected from two parallel incisions located approximately 2 cm lateral to the medial edge of the sheath and 2 cm medial to the lateral edge of the sheath extended to the anterior sheath superior to the skin island.
The skin island is now elevated from the external oblique fascia to the side of the rectus muscle flap and to the midline fascia on the opposite side of the abdomen. DIEA and the paired venae comitantes are dissected as long as possible so that the pedicle can be used to revascularize the flap through microvascular anastomosis on the chest wall when the pedicle of DSEA proves to be inadequate to support the flap. If a TRAM flap is designed as larger than usual, the inferior epigastric system on the ipsilateral side is necessary for microvascular anastomosis just like DIEP flap (Fig. 21.4).
Fig. 21.4
(a) Preoperative marking in the case of secondary breast reconstruction. (b) The contralateral pedicled TRAM flap with the deep inferior epigastric flap (DIEP flap) on the ipsilateral side for microvascular augmentation is elevated in this case
The contralateral rectus muscle including the skin island is elevated from the posterior rectus sheath based on the superior epigastric system. The pedicled TRAM flap is now passed through tunnel into mastectomy defect. After the contralateral or ipsilateral inferior epigastric vascular pedicles are anastomosed with appropriate recipient vessels when needed, the circulation of the flap is evaluated by indocyanine green (ICG) fluorescence angiography.
21.3.3 Evaluation of Flap Circulation by ICG Fluorescence Angiography
We performed intravenous injection of indocyanine green (ICG) to evaluate perfusion of the flap after the flap transposition and inset. After the injection of 5 mg of ICG (Diagnogreen 0.5 %; Daiichi Pharmaceutical, Tokyo, Japan), fluorescent images were obtained with a newly developed near-infrared camera system (PDE, Hamamatsu Photonics K.K. Hamamatsu, Japan) [12]. After intravenous injection, ICG binds strongly to plasma proteins. In the absence of capillary protein leakage, it is exclusively distributed within the intravascular space [13]. Penetrating deeper into the skin, the excitation light induces fluorescence from blood vessels in the deep dermal plexus and subcutaneous fat, instead of only the superficial dermis [14]. The induced fluorescence is not trapped in the skin and can be recorded by PDE because the skin is relatively transparent to the ICG fluorescence wavelength. In the conventional unipedicled TRAM flap without microvascular augmentation, the arteries in the rectus abdominis muscle showed strong fluorescence about 30 s after the injection of ICG. Some linear fluorescent stains can be seen in the flap about 40 s after the injection followed by diffuse stain of fluorescence. The time taken before the fluorescent stain can be seen in the flap after the injection is decided by blood tension of the patient and the thickness of skin and subcutaneous fat. When the flap has good circulation, it showed homogeneous, rapid filling and strong fluorescence. The area of zone 4 in the conventional pedicled TRAM flap usually showed very weak or no fluorescence, which indicated poor perfusion (Figs. 21.5 and 21.6). Furthermore, the distal portion of zone II and III sometimes reveals weak fluorescence. The area under suspicion of skin and fat necrosis was resected primarily in favor of a smaller final breast volume, and all of the remaining flaps survived without clinically significant skin and fat necrosis. In the case of needing a large volume of soft tissue, we always planned the microvascularly augmented pedicled TRAM flap (Fig. 21.7), which has microvascular anastomosis between either the contralateral or ipsilateral inferior epigastric vascular system and the recipient vessels. The very short half-life of ICG allows sequential monitoring of skin perfusion with short intervals within 30 min between injections [15].