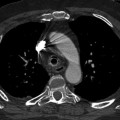
Fig. 7.1
Guide wire displaced in right pulmonary artery
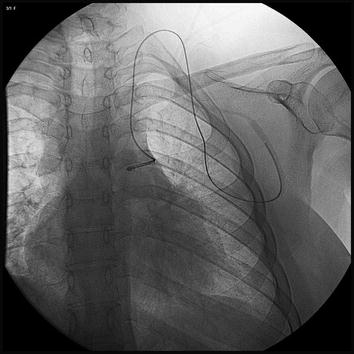
Fig. 7.2
Central venous catheter displaced in left subclavian vein
The major causes of intravascular catheter embolization were catheter injury during explantation, pinch-off syndrome, catheter disconnection, and catheter rupture [3–5]. Poor guide catheter/guide wire support, proximal vessel tortuosity, and vessel calcification are risk factors that can result in device (e.g., stent) loss (Figs. 7.3 and 7.4).

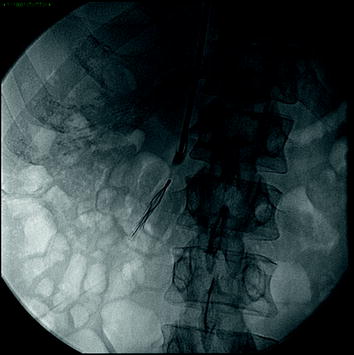

Fig. 7.3
Broken pacemaker electrodus in left subclavian vein
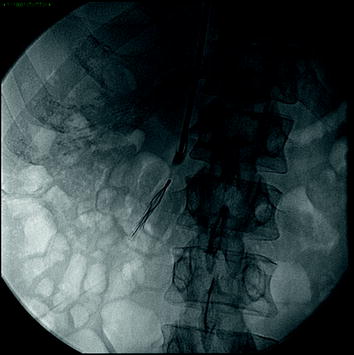
Fig. 7.4
Vena cava filter opened in the hepatic vein
In addition to faults and manufacturing defects, a high proportion of lost IFBs result from technical error and the lack of experience on the part of the operator. As we can find in the literature, the majority of migrated lines have resulted from tunneled catheters being inappropriately cut by inexperienced staff at the time of attempted line removal. To avoid this complication, good training and knowledge of the devices being used is essential. Good case planning with appropriate equipment in the range of the operator’s experience and training will be helpful.
Particular mention is required of portacath implanted in the subclavian vein, a location that carries a particular catheter injury risk, exposing them to greater total repetitive traumatic injury and risk of fragmentation. The most common location of the catheter fracture is the infraclavicular region secondary to the so-called pinch-off syndrome or thoracic inlet syndrome. Previous data suggest that material fatigue may play a key role in catheter fracture [6].
The first step in IFB research is an accurate medical history of the patient; it is necessary to have information about the type of catheter, the shape, size, and the possible location of the object.
Depending on the type of catheter and its primitive location, the first diagnostic orientation should be based on its possible presence in the arterial, venous, or pulmonary vessels. In fact, on the basis that most IFBs are fragments of devices, their detachment follows an embolization in the direction of blood flow, in almost all cases. For these reasons, for central venous catheters and peripheral venous catheters the vessels of probable location will be the central veins, the right heart, and the pulmonary circulation, while for IFBs that originate in an artery we have to turn our attention to a possible peripheral embolization.
As regards imaging, plain film is the first-line investigation followed by fluoroscopy. Catheter fragments are generally fluoroscopically poorly visible because they are small and are made of material that poorly attenuates X-rays. Overlying tissues and movement-related artifacts (e.g., cardiac motion) further reduce fluoroscopic image clarity. Some authors suggest to use computed tomography (CT) as a first-line investigation, but we have to consider the higher risk of radiation exposure for the patient []. Catheter fragments may be very small, and it could be hard to identify them even on CT. Magnetic resonance imaging (MRI) is done when we are sure that the foreign body is known to be MRI compatible in cases of peripheral embolization. In the case of metallic lost IFBs, a gradient echo sequence will result in susceptibility artifacts. Ultrasound, sometimes, can be helpful in detachment. To avoid further device migration, once localized, the interval to subsequent attempted device retrieval should be minimized.
7.3 Noniatrogenic Intravascular Foreign Bodies
The majority of noniatrogenic intravascular foreign bodies consist in gunshot bullets.
A bullet embolus should be suspected in any patient who has a gunshot wound without an exit wound, when the signs and symptoms do not correlate with those expected from the suspected course of the missile, and when radiological investigations show that missile location deviates from the path of penetration [7, 8]. Bullet emboli access the vascular system by direct propulsion or erosion into the vessel lumen. Eighty percent are arterial in nature with only 20 % being venous. Arterial embolization is symptomatic (claudication, peripheral ischemia, and thrombophlebitis) in 80 % of cases, and typically originates from the pulmonary artery, heart, or great vessels with embolization to peripheral vessels causing limb ischemia, particularly in the lower extremities. Venous embolization is symptomatic (dyspnea, haemoptysis, and chest pain) in 30 % of cases, with embolization from the large peripheral veins, vena cava or liver, to the right side of the heart, particularly the right ventricle or pulmonary arteries [8].
There are two rare documented subgroups of embolization. First is retrograde embolization seen in 15 % of venous cases and defined as projectile movement against the normal direction of blood flow. Second is paradoxical embolization, defined as the passage of a foreign body from the venous to the arterial system by communication through a right to left shunt. Causes include arteriovenous fistula, atrioventricular perforation, ventricular septal defect, or patent foramen ovale [9]. Diagnosis of foreign body emboli is through X-ray, computerized tomography, and echocardiography.
Unlike iatrogenic embolization, the traumatic patient hemodynamically stable undergoes an evaluation of imaging by CT in almost all cases. So CT is often the first method used. However, repeated X-ray examination is the best method for an accurate assessment of possible vascular migration of missile. Even in these cases ultrasound can demonstrate the hyperechoic IFB with the characteristic trailing band of increased echogenicity (comet tail) [10].
The MRI is strictly contraindicated for the magnetic nature of bullet.
7.4 IFB Retrieval
The first case of IFB was documented in 1954 [11], the case report detailing a CVC found in the right atrium of a patient during autopsy. A few years later, in 1964 [12], Thomas described the first percutaneous retrieval, through a bronchoscopic forceps, of an IFB, a fragment of guide wire migrated into the right atrium. The technique was quickly adopted as an alternative to surgical removal and nowadays the percutaneous intravascular recovery is considered the “gold standard” [13]. Key factors to achieve a successful outcome are appropriate knowledge of the equipment available, the different techniques, and obviously the operator experience. We have already considered the need for careful imaging to detect the foreign body and also planning the procedure to minimize the risks connected. The presence of the anesthesiologist is important, as in any interventional procedure, to ensure the right management of the patient [13]. It is also necessary to adequately inform the patient about the procedure, the risks associated, and the possible alternative treatments [14]. It is essential to have in one’s arsenal, ready for use, all necessary devices such as snares, intravascular forceps, sheaths of various sizes, guide wires, various shaped catheters, and occlusion balloons. Previous planning can optimize the procedure choosing the best way to go.
7.5 Removal Techniques and Devices
The loop snare is frequently the first choice device for the removal of an IFB. The modern design allows the loop to emerge at 90° to the catheter facilitating by far the tracking of the loop and then the capture of IFB. There are snare loops of various sizes, including microsnares (e.g., Radius Medical) from 2 gauges up to 35 mm (Gooseneck, EV3, Welter retrieval loop, Cook, Trefoil ensnare/TriSnare Merit Medical). All models of loop snares are designed on the same principle: the use of moveable nitinol wire loop which passes through a guiding catheter. The snares have an excellent safety profile, are relatively atraumatic, simple to use, and effective even in less experienced hands [13, 15].
7.6 Proximal Capture Technique
This is the basic technique when using a loop snare. It is necessary to use a loop snare of a size appropriate to the vessel; i.e., the fully open loop must be of a size equal to or slightly smaller than the vessel where the IFB is located [13, 16]. The snare loop proceeds to the target vessel on a previously positioned guide wire. When the snare is in position within the target vessel the external catheter is withdrawn allowing the loop to fully open within the vessel lumen. The whole system is then advanced to positioning the open loop around the IFB, or around a specific part of it. Now the loop is closed by advancing the catheter to tighten the IFB. When the complete control of IFB occurs, the entire system, along with the IFB, is pulled back into the sheath. To be successful, a free end on the IFB is needed. On the contrary, there are two options: either the approach from a different direction, or the use of a shaped catheter like an SOS Omni or a balloon that can be used to stop, move, or bend the IFB to allow the access to a free end of the same. When the snare holds the IFB, this one could lie perpendicularly: if it is a floppy one, no problem occurs because it folds into half [13




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree