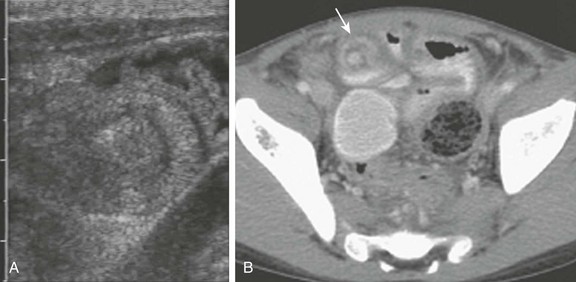
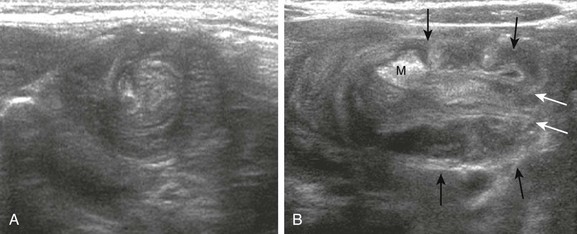
Chapter 108 Intussusception is an acquired invagination of the bowel into itself, usually involving both small and large bowel (Fig. 108-1). The more proximal bowel that invaginates into more distal bowel is termed the intussusceptum, whereas the recipient bowel that contains the intussusceptum is termed the intussuscipiens. Invagination of the bowel leads to edema, and ischemic changes eventually supervene; thus intussusception is an urgent condition, but prolonged delay in diagnosis is not uncommon, resulting in increased risk for patients to present with obstruction, necrosis, and bowel perforation. Figure 108-1 The common types of infantile intussusception, in longitudinal section. Intussusception occurs with an incidence of at least 56 per 100,000 children per year in the United States, and it is the most common cause of small bowel obstruction in children.1 In frequency, it is second only to pyloric stenosis as a cause of gastrointestinal tract obstruction in children, occurring in boys more often than girls at a ratio of 3 : 2. Classic pediatric intussusception involves invagination of the distal ileum into the colon, as ileocolic or ileoileocolic intussusception; however, intestinal intussusception may occur along the entire length of the bowel from the duodenum to the colon. Cases of intussusception range from the classic, symptomatic, and urgent presentation, to short-segment, transient, and asymptomatic events, typically isolated to the small bowel, and seen increasingly on ultrasound or on computed tomography (CT) of the abdomen performed for other indications (e-Fig 108-2).2 This chapter will focus on ileocolic and ileoileocolic intussusception. e-Figure 108-2 Transient intussusception of the small bowel. Most cases of ileocolic intussusception occurring in children are idiopathic. It is hypothesized that the typical childhood ileocolic intussusception results from hypertrophied lymphoid tissue in the terminal ileum (Peyer patches). Some reports suggest a viral etiology, most commonly adenovirus, but enterovirus, echovirus, and human herpes virus 6 also have been implicated.1,3 An accompanying pathologic lead-point mass lesion may be present in 5% to 6% of all children,4,5 particularly when intussusception occurs outside of the typical idiopathic age range or when symptomatic intussusception is confined to the small bowel or the colon. Shortly after the first rotavirus vaccine was introduced in the United States in 1998 for routine vaccination of infants at ages 2, 4, and 6 months, several reports to the Centers for Disease Control and Prevention suggested an association between the vaccine and intussusception. The vaccine was removed from the world market in 1999. Subsequent investigations have demonstrated clear benefits in reducing morbidity and mortality, although some authors report a very small risk of intussusception after rotavirus vaccination.6,7 Two new vaccines are now available. Approximately 5% to 6% of intussusceptions in children are caused by pathologic lead points, either focal masses or a diffuse bowel wall abnormality.4,5,8 The traditional view is that focal lead points are more common in older children. Although the absolute numbers of lead points are approximately equal in infants and in older children, the percentage of lead points in infants is lower because of the greater number of intussusceptions occurring in this age group.4 The most common focal lead points are (in decreasing order of incidence) Meckel diverticulum, duplication cyst, polyp, and lymphoma. In older children, lymphoma is the more likely lead point, typically Burkitt lymphoma. Diffuse lead points are most commonly associated with cystic fibrosis or Henoch-Schönlein purpura. Colonic polyps can result in colocolic intussusception. Idiopathic intussusception occurs most commonly in infants between 2 months and 3 years of age, with a peak at age 5 to 9 months; authors of studies with a large series report that 57% to 85% of cases present before the age of 1 year (average, 67%).8,9 The classic clinical presentation of the child with intussusception is colicky abdominal pain, vomiting, bloody stools, and a palpable abdominal mass.9 Children with intussusception should be diagnosed as early as possible to avoid bowel ischemia, necrosis, and surgery; however, this goal remains elusive. The clinical signs and symptoms of intussusception are often nonspecific and may overlap with those of gastroenteritis, malrotation with volvulus, and in older children, Henoch-Schönlein purpura. The classic triad of colicky abdominal pain (58% to 100% of cases), vomiting (up to 85% of cases), and bloody stools (up to 75% of cases)10,11 is present in less than 25% of children.10,12 No reliable clinical prediction models exist that can identify all children with intussusception.12–14 In one study, it was found that only 50% of children were correctly diagnosed at initial presentation to a health care provider.15 The most important factor, either alone or in combination with other factors, that predicts an unsuccessful enema reduction is a longer duration of symptoms; 48 to 72 hours typically is considered a significant delay.8,9 Other factors associated with lower rates of successful reduction include age less than 3 months, dehydration, small bowel obstruction, and intussusception encountered in the rectum (resulting in a 25% reduction rate).8,9,15–17 Additional findings that affect bowel edema, bowel viability, and success of nonsurgical reduction relate to imaging findings and are addressed in the next section. On the basis of sonographic or enema diagnosis before surgery, the rate of spontaneous reduction is estimated to be 10%.4,18,19 Box 108-1 summarizes the evidence regarding imaging management of intussusception. Abdominal radiographs have a limited sensitivity and specificity for the detection of intussusception, even when viewed by experienced pediatric radiologists.9,20 Sargent and colleagues16 reported a sensitivity of 45% in 60 children when they were evaluated prospectively by pediatric radiologists, using an enema as the reference standard. Adding a left side down decubitus has been shown to improve sensitivity.21 The presence of a curvilinear mass within the course of the colon (the crescent sign), particularly in the transverse colon just beyond the hepatic flexure, is a nearly pathognomonic sign of intussusception (Fig. 108-3). The absence of stool or recognizable colonic gas in the ascending colon is one of the more suggestive signs of intussusception on radiographs. However, fluid filling the ascending colon in a patient with gastroenteritis may falsely suggest intussusception, and small bowel gas located in the right abdomen on radiographs may mimic ascending colon or cecal gas. Figure 108-3 Ileocolic intussusception in a 4-year-old child. Ultrasound is highly sensitive in the detection of intussusception (see Table 108-1), even when it is performed by relatively inexperienced operators and with equipment that is no longer state of the art.22,23 Although the diagnosis can be confirmed when the enema procedure is performed, ultrasound is the primary imaging modality for the initial diagnosis outside of the United States; it is used by 93% of European pediatric radiologists,24 as well as by a growing number of pediatric radiologists in the United States. Initial evaluation by ultrasound circumvents the more invasive enema in patients who do not have intussusception, and it allows diagnosis of other conditions, such as mesenteric adenitis or colitis, for which performance of an enema would not be the procedure of choice.12,25,26 Table 108-1 Sensitivity and Specificity of Diagnostic Imaging for Ileocolic Intussusception Intussusception can be diagnosed by ultrasound when a donut, target, or “pseudokidney” sign is seen, most often in the right upper quadrant of the abdomen.27 This appearance arises from intussuscepted bowel and mesentery within the intussuscipiens, producing the donut or target appearance on transverse images and a hypoechoic mass with hyperechoic center on longitudinal images; the hyperechoic center represents the intussuscepted mesentery. Using a linear transducer, the more specific bowel-within-bowel appearance can be seen, and the leading edge of the intussusception can be inspected to confirm that a pathologic lead point is not present (Fig. 108-4). Optimal sonographic techniques are well described,26–28 and there are no known contraindications to, or complications resulting from, ultrasound used for this purpose. Figure 108-4 Intussusception. Ultrasound evaluation in children suspected of intussusception has been suggested to reduce cost, radiation exposure, and anxiety in both patients and parents over the discomfort of the enema.12 The accuracy of ultrasound evaluation approaches 100% with a sensitivity of 98% to 100% and a specificity reported at 88% to 100%.12,22,23,29 Its cost effectiveness, of course, depends on the prevalence of intussusception, because very few positive diagnoses would be expected in a population in which the prevalence of intussusception is very low. Anechoic fluid trapped between the intussusceptum and the intussuscipiens has been associated with lack of reducibility, whereas abundant flow on color Doppler interrogation is a predictor of reducibility (Fig. 108-5).25,30 Free intraperitoneal fluid in small or moderate amounts is present in approximately half of children,27 and reports are conflicting as to whether free peritoneal fluid is associated with fewer successful reductions.18,28 Similarly, authors of some reports note that a thicker bowel wall is associated with fewer successful enema reductions, but others have not been able to verify this association. Other authors report that the presence of lymph nodes within the intussusceptum complex is associated with decreased success of reduction.22,27,31 Although some of these findings are associated with fewer successful reductions, none represents a contraindication to enema reduction. Contraindications to enema reduction are signs of peritonitis or free intraperitoneal air. Figure 108-5 Intussusception. The detection of lead points by imaging is challenging. Ultrasound is the noninvasive standard of reference (Fig. 108-6). Ultrasound is reported to identify approximately 66% of lead points,32 whereas approximately 40% are identified by positive-contrast liquid enema.4,8,9,32 Air enema has a lower rate of detection (11%), leading some investigators to suggest that ultrasound be used afterward to search for lead points.19
Intussusception
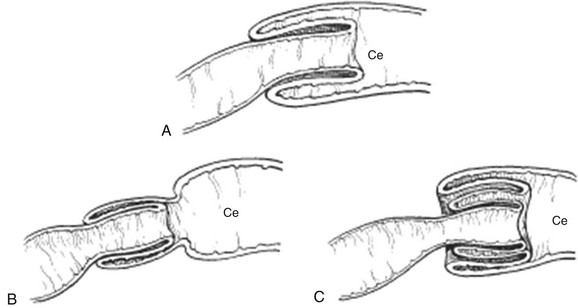
A, Ileocecal. B, Ileoileal. C, Ileoileocolic. Ce, Cecum.
A, A transverse image of ileoileal intussusception incidentally identified in an infant with gastroenteritis; on longitudinal image it measured <3 cm, and it could not be identified on rescanning of the area. B, An abdominopelvic computed tomography image of a young child undergoing routine follow-up imaging of a testicular tumor. An asymptomatic, short-segment, small bowel intussusception (arrow) resolved spontaneously. (A, Courtesy Dr. Marta Hernanz-Schulman, Nashville, TN.)
Etiology
Rotavirus Vaccine
Pathologic Lead Points
Clinical Presentation
Clinical Predictors of Intussusception and Nonsurgical Reduction
Diagnosis and Imaging
Abdominal Radiographs
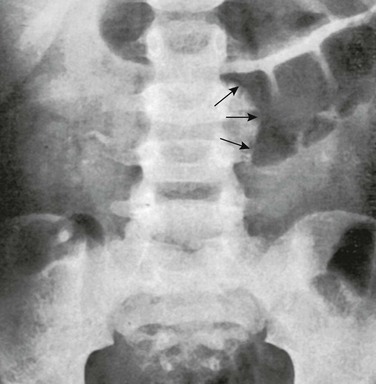
The leading edge of the intussusception (arrows) is seen on this radiograph outlined by gas within the transverse colon. No gas can be seen in the cecum or in the ascending colon.
Ultrasonography
Test
Sensitivity (%)
Specificity (%)
Abdominal radiograph
45
Unknown
Ultrasound
98-100
88-100
Enema*
100
100
A, A 3-month-old boy with intussusception. A transverse ultrasound image through the intussusceptum complex shows the donut or target sign, with intussusceptum composed of small bowel, nodes, and mesentery surrounded by the intussuscipiens. B, A longitudinal section of intussusception in the same patient as depicted in part A. The image shows the terminal end of the intussusception, with the inner and outer sleeves of the intussusceptum (white arrows) containing the intussuscepted mesentery (M). Black arrows outline the outer edge of the intussuscipiens. Note that no lead point is present. (Courtesy Dr. Marta Hernanz-Schulman, Nashville, TN.)
Ultrasound Predictors of Enema Reducibility and Bowel Necrosis
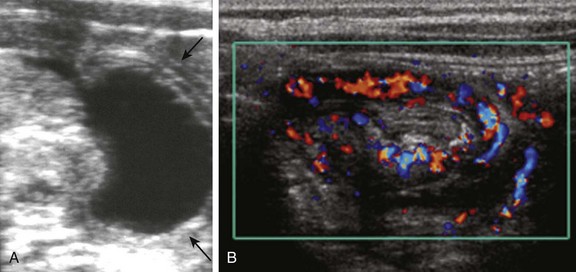
A, Trapped fluid in an infant with intussusception. Fluid is visible at the leading edge of the intussusceptum complex. Arrows point to the outer edge of the intussuscipiens. B, A color Doppler transverse image of the right flank in a different patient outlines abundant flow to intussusceptum and intussuscipiens. The intussusception was successfully and rapidly reduced with air enema. (A, Courtesy Dr. Marta Hernanz-Schulman, Nashville, TN.)
Pathologic Lead Points
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Intussusception





