Fig. 57.1
Coronal T1-weighted MRI in a 31-year-old woman with wrist pain. The patient has ulnar-negative variance and low signal is seen in the lunate. Plain radiograph showed no pathology


Fig. 57.2
(a) PA radiograph of a wrist in a 11-year-old female showing sclerosis of the lunate with no collapse. (b) Coronal MRI (fat suppressed proton density) of the same patient showing increased T2 signal in the lunate consistent with possible ischemia and stage 2 Kienbock’s disease. (c) Coronal T1 weighted image of the same patient showing loss of normal fatty signal in the lunate, consistent with Keinbock’s disease. (d) Sagittal MRI of the same patient with increased T2 signal in the lunate consistent with possible ischemia and stage 2 Kienbock’s disease
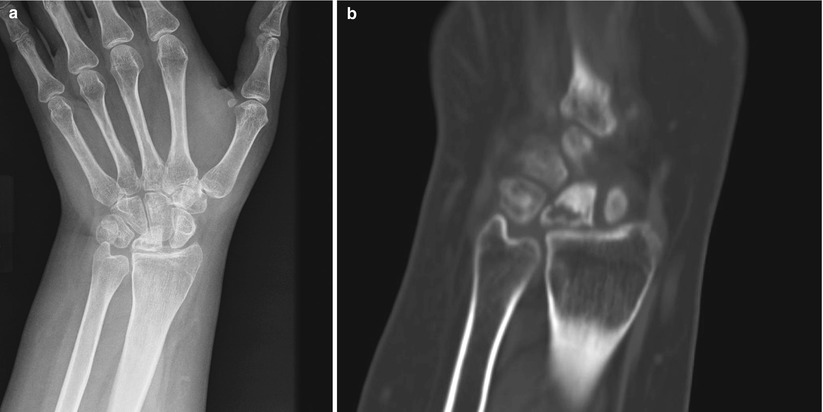
Fig. 57.3
(a) PA radiograph of the left wrist in a 20 year-old woman showing sclerosis of the lunate with early collapse, proximal migration of the capitate, and rotation of the scaphoid (Stage 3B). (b) Coronal and sagittal CT image of the same wrist showing sclerosis and collapse of the lunate with fracture line through a central lucent area

Fig. 57.4
PA radiograph of wrist showing avascular necrosis of the lunate with associated degenerative change
MRI may be useful for the early stages of the disease when no pathology is found on plain films. A decreased T1 signal will commonly be seen. Computed tomography scanning can also be useful to define the lunate collapse seen at later stages.
Table 57.1
Lichtman’s classification for Kienböck’s disease
Stage 1 | No findings on plain films, possible low signal on T1 MRI |
Stage 2 | Lunate sclerosis evident on plain films |
Stage 3a | Collapse of lunate articular surface but with normal carpal height |
Stage 3b | Collapse of lunate articular surface and with carpal collapse, fixed scaphoid in flexion, proximal capitate migration |
Stage 4 | Collapse of lunate with radiocarpal or midcarpal arthritis on plain films |
57.2.4 Treatment
The treatment recommendations for the early stages of this disease remain controversial as do the outcomes. The natural history of lunate osteonecrosis is not clear as there are few limited studies with suboptimal power and study design [8, 9]. A recent systematic review study on nonoperative versus operative treatment showed that in late stages of the disease, nonoperative treatment led to 63 % pain improvement compared to up to 90 % in surgically treated patients [10].
As with most orthopedic conditions, immobilization is the first line of treatment. Studies on conservative treatment have shown that radiographic severity of the disease does not always correlate with severity of symptoms [8, 9]. Thus, patients should be treated according to their symptoms in conjunction with their radiographs rather than by their radiographic disease progression alone. Many patients, including some with advanced radiographic changes, may have limited symptoms or functional limitations. As such, a trial of nonoperative management is recommended in most patients.
In symptomatic patients, after nonoperative measures have failed, surgery is indicated. Surgical options range from arthroscopic debridement, core decompression, osteotomies, to vascularized bone grafting and salvage procedures. Studies have not shown one operative treatment to be significantly superior to another [10].
A general algorithm of treatment begins with immobilization with a cast or splint, pins, or an external fixator for up to 12 weeks. This would predominantly apply to patients with minimal symptoms and to symptomatic patients in stage I of the disease. Arthroscopic debridement has been described in early stages with successful symptom relief [6, 11]. Core decompression has also been described in early stages (stages 1-3A) to provide good outcomes [12]. In this procedure, 2 × 0.5 cm cortical windows are created in the distal radius and ulna, and small curettes are used to decompress the metaphysis.
As the disease progresses to stages 2 and 3, treatment is focused on unloading the lunate and restoring vascularity. In patients with ulnar-negative variance, radial shortening osteotomies or ulnar lengthening procedures can help decrease radiolunate load. Radial shortening procedures are more commonly performed with better reported outcomes compared to ulnar lengthening secondary to higher rates of nonunion in the latter [5, 6, 13, 14]. Radial shortening osteotomy is contraindicated in patients with ulnar neutral or positive variance. Radial wedge or dome osteotomies can be performed in these patients to reduce radial inclination thereby increasing the radiolunate contact surface area. This has been shown to reduce the force across the radiolunate and capitolunate joints [5, 6, 15]. Capitate shortening may also unload the lunate in patients that are ulnar neutral or ulnar positive [16].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree