The vulnerability of the knee, the largest joint in the body, to direct trauma makes knee injuries very common throughout life. Most acute injury to the knee is sustained during adolescence and adulthood, with motor vehicle accidents and athletic activities being the major causing factors. Fractures are much more common than dislocations, but injuries to the cartilaginous and soft-tissue structures, such as tears of the menisci and ligaments, are the most common types of injuries, particularly in older adolescents and younger adults. The symptoms accompanying knee trauma vary according to the specific site of injury and thus constitute important indications of the type of injury. However, clinical history and physical examination are rarely sufficient for making a precise diagnosis. Radiologic examination plays a determining role in diagnosing the various traumatic conditions involving the knee joint.
Anatomic-Radiologic Considerations
Conventional radiographs are the first-line approach to the traumatized knee, and often they are sufficient for evaluating many traumatic conditions of the joint. However, the great incidence of cartilaginous and softtissue injuries, occurring either as isolated conditions or in association with fractures, requires the use of ancillary imaging techniques for adequate evaluation of the joint capsule, articular cartilage, menisci, and ligaments.
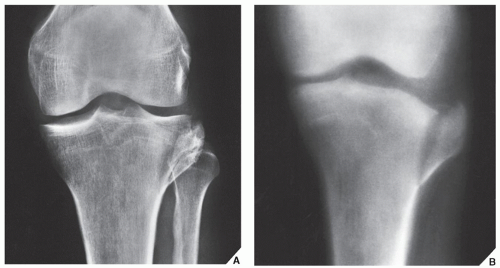
The standard radiographic examination usually consists of obtaining radiographs of the knee in four projections: the anteroposterior, the lateral, and the tunnel projections, as well as an axial view of the patella. The
anteroposterior radiograph of the knee allows sufficient evaluation of many of the most important aspects of the distal femur and proximal tibia: the medial and lateral femoral and tibial condyles, the medial and lateral tibial plateaus and tibial spines, and the medial and lateral joint compartments and the head of the fibula (
Fig. 9.1). However, the patella is not well demonstrated on this view because it is superimposed on the distal femur. Proper evaluation of this structure requires a
lateral projection (
Fig. 9.2) on which the relationship of the patella and femur can also be assessed. Proximal (superior) displacement of the patella is called
patella alta; distal (inferior) displacement is called
patella baja. The length of the patella is measured from its upper pole (base) to the apex. The length of the patellar ligament is measured from its proximal attachment, just above the apex, to the notch on the proximal margin of the tibial tubercle. These two measurements are approximately equal and the normal variation does not exceed 20% (
Fig. 9.3). In addition to imaging the patella in profile, the lateral radiograph of the knee allows evaluation of the femoropatellar compartment, the suprapatellar bursa (pouch), and the quadriceps tendon. The femoral condyles overlap on this projection, and the tibial plateaus are demonstrated in profile. Occasionally, a cross-table lateral view of the knee—obtained with the patient supine, the affected leg extended, and the central beam directed horizontally—may be required to demonstrate the intracapsular fat-fluid level (fat-blood interface [FBI] sign of lipohemarthrosis; see
Fig. 4.38B). An angled posteroanterior projection of the knee, known as the
tunnel (or
notch)
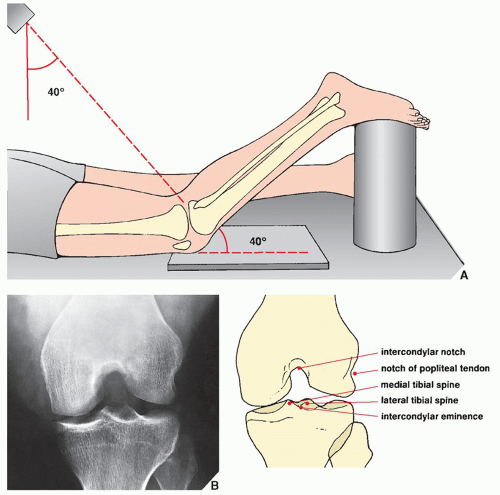
view, is also obtained as part of the standard radiographic examination (
Fig. 9.4). This view is useful in visualizing the posterior aspect of the femoral condyles, the intercondylar notch, and the intercondylar eminence of the tibia.
To demonstrate an
axial view of the patella, various techniques are available. The one most commonly used provides what has been called the
sunrise view (
Fig. 9.5). However, the degree of flexion required to obtain this view results in depressing the patella more deeply within the intercondylar fossa; consequently, the articular surfaces of the femoropatellar joint are not well demonstrated, and subtle subluxations of the patella may not be detected. To overcome this limitation, Merchant and colleagues have described a technique for obtaining an axial view of the patella that demonstrates the femoropatellar joint to better advantage (
Fig. 9.6). It is particularly effective in detecting subluxations of the patella because it allows specific measurements to be made of the normal relations of the patella to the femoral condyles. Subtle abnormalities in these relations may not be seen on the standard axial view because of the degree of knee flexion required for that view, which prevents the patella from subluxing.
The measurements of the femoropatellar relations obtainable from Merchant axial projection concern the sulcus angle and the congruence angle (
Fig. 9.7). Normally, the
sulcus angle, which is described by the highest points of the femoral condyles and the deepest point of the intercondylar sulcus, measures approximately 138 degrees. By dissecting this angle with two lines—a reference line drawn from the apex of the patella to the deepest point of the sulcus and a second line from the lowest point of the patellar articular ridge to the deepest point of the sulcus—Merchant and colleagues were able to determine the degree of congruence, or the
congruence angle, of the femoropatellar joint. When the deepest point of the patellar articular ridge fell medial to the reference line, the angle formed was assigned a negative value; when it fell lateral to the reference line, the angle was designated with a positive value. In 100 normal subjects included in their study, the average congruence angle was −6 degrees. An angle of +16 degrees or greater was found to be associated with various patellofemoral disorders, particularly lateral patellar subluxation (see
Fig. 9.46). On occasion, patellofemoral disorders that are more difficult to diagnose may require, as Ficat and Hungerford recommended, additional tangential views obtained with 30, 60, and 90 degrees of knee flexion.
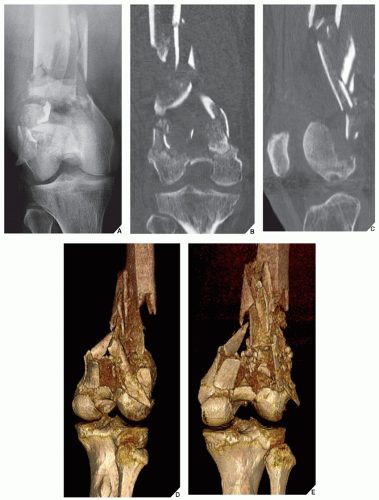
Among the ancillary techniques available for the evaluation of injuries to the knee, arthrography, computed tomography (CT), and magnetic resonance imaging (MRI) provide crucial information. CT is especially useful in the evaluation of complex fractures of the distal femur, the tibial plateaus, and the patella. In fractures of the tibial plateaus, it is effective in determining the amount of depression of the articular surface and in identifying small comminuted fragments that may be displaced into the joint, as well as comminution about the tibial spines, which may indicate avulsion of the cruciate ligaments. Tomography, by its ability to demonstrate the integrity of the anterior cortex, is also helpful in planning a surgical approach to the treatment of tibial plateau fractures.
Arthrography used to be the procedure of choice in evaluating injuries to the soft-tissue structures of the knee, such as the joint capsule, menisci, and ligaments (
Fig. 9.8). It is still valuable in examination of the
articular cartilage, particularly when subtle chondral or osteochondral fracture is suspected, or when confirmation of the presence or absence of osteochondral bodies in the knee joint is required in suspected osteochondritis dissecans. However, in the evaluation of the menisci, cruciate ligaments, and collateral ligaments, arthrographic examination has been almost completely replaced by MRI.
The medial and lateral menisci (or semilunar cartilages) of the knee are crescent-shaped fibrocartilaginous structures attached, respectively, to the medial and lateral aspects of the superior articular surface of the tibia (
Fig. 9.9). Normally, the medial meniscus is visualized on arthrography as a triangular structure intimately attached to the joint capsule and tibial (medial) collateral ligament; its smooth borders are coated by positive contrast agent and surrounded by injected air. The normal arthrogram shows no air or contrast within the substance of the meniscus or at its periphery (
Fig. 9.10A-C). Although the lateral meniscus is structurally very similar to the medial meniscus, it has a very important distinguishing feature. The popliteal muscle’s tendon and its sheath pass through a portion of the posterior horn of the lateral meniscus, separating it from the joint capsule. This anatomic site, known as the
popliteal hiatus, gives an arthrographic impression of separation of the periphery of the lateral meniscus from the capsule; it should not be mistaken for a tear (
Fig. 9.10D,E). An important fact to remember is that not all areas of the menisci are well demonstrated by knee arthrography. Only the parts seen tangentially can be assessed accurately. For example, the posterior part of the posterior horn of the lateral meniscus constitutes a blind spot because it extends deeply into the knee joint (see
Fig. 9.9).
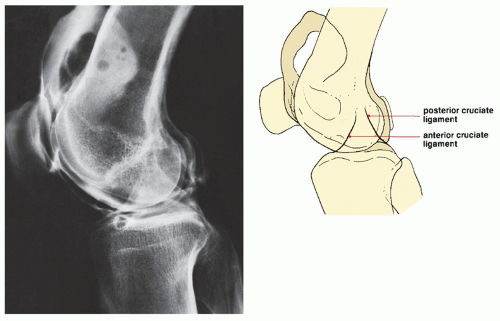
The cruciate ligaments of the knee are also structures commonly subject to injury (
Fig. 9.11). In the evaluation of these ligaments, arthrography was the procedure of choice before the MRI era and is even now occasionally performed. The radiograph is obtained to best advantage in the lateral projection with 60 to 80 degrees of knee flexion and with the examiner applying pressure to the posterior aspect of the proximal tibia. When tensed, the anterior cruciate ligament (ACL) normally projects as a straight line extending from the intercondylar notch to a point approximately 8 mm posterior to the anterior margin of the tibia. The posterior cruciate ligament is seen as a straight or slightly bulging line extending to the posterior margin of the tibial plateau (
Fig. 9.12).
In the past decade, MRI of the knee has gained wide acceptance in the diagnosis of traumatic abnormalities and currently is the method of choice in evaluating various knee structures, particularly the menisci, cruciate ligaments, and collateral ligaments. Routinely, T1-weighted and T2-weighted images are obtained in the sagittal, coronal, and axial planes. The sagittal plane is generally the most effective for evaluation of the cruciate ligaments, menisci, patellar ligament, and quadriceps tendon. Coronal sections are needed for evaluation of the medial and lateral collateral ligaments, as well as the menisci. The axial plane is best to evaluate the patellofemoral joint compartment. The axial plane is also helpful in evaluating the popliteal cysts and their relationship to the surrounding structures of the popliteal fossa.
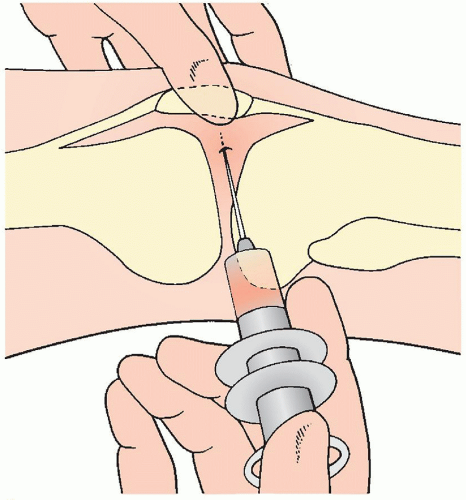
MR arthrography (MRa) is effective in evaluating residual or recurrent meniscal tears after meniscal surgery. It is also a valuable technique to demonstrate loose intraarticular chondral or osteochondral bodies, synovial plicae, and to evaluate the stability of various osteochondral lesions, including osteochondritis dissecans and osteochondral fracture. MRa of the knee is performed by injecting up to 40 mL of diluted gadolinium solution into the joint using the same technique as described for conventional knee arthrography (see
Fig. 9.8). Coronal, sagittal, and axial images are obtained, most commonly with fat-suppressed T1- (or proton density) and T2-weighted sequences.
The menisci are seen on MRI as wedge-shaped or bow tie-shaped structures of uniformly low signal intensity in practically all pulse sequences (
Fig. 9.13). The anterior and posterior cruciate ligaments, like the menisci, are seen as low-signal intensity structures on all spin echo sequences. The ACL is straight and fan shaped (slightly wider at its femoral attachment) and demonstrates low-to-intermediate signal intensity (
Fig. 9.14A). The posterior cruciate ligament is arcuate in shape when the knee is in extension or mild flexion and becomes increasingly taut as the knee is flexed. Normally, it has very low signal intensity (
Fig. 9.14B). Anteriorly to the posterior cruciate ligament, one can observe a small bulge produced by the anterior meniscofemoral ligament, also known as the
ligament of Humphrey (
Fig. 9.14B,C). Posteriorly, a small bulge is created by the posterior meniscofemoral ligament, known as the
ligament of Wrisberg (
Fig. 9.14D,E).
The medial collateral ligament consists of two components: superficial and deep. The superficial component, which is the principal medial stabilizer of the knee, arises from the medial femoral epicondyle just below the adductor tubercle and inserts into the medial aspect of the tibia, approximately 5 cm below the joint line. The deep layer of the medial collateral ligament, which is considered part of the fibrous capsule, attaches loosely to the peripheral margin of the body of the medial meniscus. The lateral collateral ligament attaches to the lateral epicondyle of the femur superiorly just above the popliteus groove, in which region it merges with the outer surface of the capsule. From here, it extends inferiorly and posteriorly to attach to the anterior portion of the apex of the fibular head. Both collateral ligaments are best demonstrated on the images obtained in the coronal plane. Like the menisci and cruciate ligaments, they also display low signal intensity (
Fig. 9.15).
During evaluation of MRI of the knee, it is helpful to use a checklist as provided in
Table 9.1.
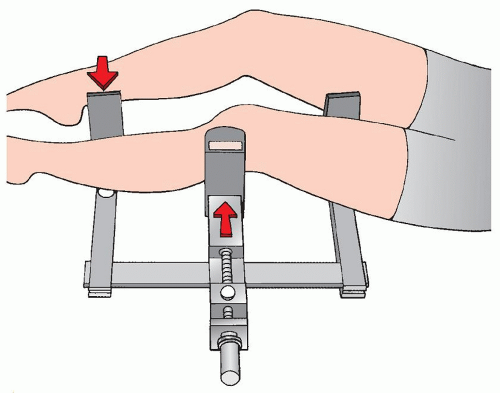
Evaluation of knee instability caused by ligament injuries may require obtaining stress views. These techniques are most commonly performed in cases of suspected injury to the medial collateral ligament (
Fig. 9.16; see also
Fig. 9.83). They are less frequently performed during the evaluation of insufficiency of the anterior and posterior cruciate ligaments (
Fig. 9.17). These examinations should preferably be performed under local anesthesia.
Arteriography and venography may need to be used in the evaluation of concomitant injury to the vascular system, although recently more often MR angiography is performed for this purpose. CT is effective in the evaluation of tibial plateau fractures, and it is occasionally used to evaluate injury to
the cartilage and soft tissues, particularly the menisci and cruciate ligaments. CT used in conjunction with arthrography (computed arthrotomography) is useful in the evaluation of osteochondritis dissecans (see
Fig. 9.60C,D) and in detecting nonopaque osteochondral bodies in the knee joint.







 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access