Chapter 67 Spin echo and gradient echo sequences are used for cardiac evaluation. Spin echo, or “black blood,” imaging gives excellent contrast resolution between the endocardium or vessel wall and the blood-filled lumen. Double inversion recovery imaging adds additional nonselective and selective 180-degree pulses to further null the blood signal. The double inversion recovery pulse sequence is the current backbone of spin echo morphologic cardiac imaging in teenagers and adults, but it requires that the patient hold his or her breath (Fig. 67-1). More traditional T1-weighted sequences are used in uncooperative or sedated children. T1-weighted sequences are longer but do not require that patients hold their breath. Blood has a high signal in gradient echo sequences and is the basis for “white blood” or “bright blood” imaging. Balanced SSFP (b-SSFP) is the state-of-the-art gradient echo sequence for bright blood imaging. b-SSFP sequences are faster than earlier gradient echo sequences and have better contrast between myocardium and blood. As with double inversion recovery imaging, b-SSFP is ideally performed with the patient holding his or her breath. Respiratory motion artifacts are minimized in the sedated or uncooperative patient by increasing the number of excitations. This technique is the preferred sequence for evaluating cardiac motion and quantifying cardiac function. Stenosis and turbulent flow appear as a black jet in the white blood on gradient imaging (Fig. 67-2). MRI is the gold standard for cardiac function assessment and is markedly superior to echocardiography in assessing right ventricular function. A stack of short-axis cine images through the ventricles in end-systole and end-diastole is used to measure ventricular volumes.1 The product of the endocardial cross-section tracing and the section thickness is the section volume. The section volumes are summated to determine end-diastolic and end-systolic volumes for the right and left ventricles. The same images are used to measure the left ventricle mass by performing epicardial and endocardial tracings. The difference in the volumes circumscribed by the epicardium and endocardium is the left ventricle myocardium volume, from which mass is determined. The stroke volumes of the right and left ventricles are the same in the structurally normal heart. Differences in stroke volumes are caused by shunts and valve regurgitation. Using MR, both shunt size and regurgitant fraction can be calculated from the stroke volumes. Shunt size, or the pulmonary to systemic flow ratio (Qp : Qs), is determined by dividing the larger stroke volume by the smaller. The valvular regurgitant fraction is determined by dividing the regurgitant volume, which is the difference of ventricle stroke volumes, by the larger ventricle stroke volume (Fig. 67-3). The regurgitant volume may result from atrioventricular valve or semilunar valve or a combination of both. Figure 67-3 Pulmonary regurgitation. where volume1 is the larger of the two ventricular stroke volumes. Quantitative phase-contrast imaging uses gradient echo sequences to measure phase shift. Flow quantification using a plane of imaging perpendicular to the vessel or valve of interest allows quantification of blood flow and velocity. Flow quantification gives both magnitude and directional information (Fig. 67-4). Shunt volumes and regurgitant fractions are quantified. Regurgitation is quantified by: The pressure gradient across a stenosis is calculated using the modified Bernoulli equation: Figure 67-4 Tetralogy of Fallot. where ΔP is the peak instantaneous pressure gradient across the stenosis and v is the velocity across the stenosis measured by flow analysis. Contrast-enhanced magnetic resonance angiography (CE-MRA) is performed after injection of a gadolinium chelate bolus. The technique relies on T1 shortening of blood and requires rapid imaging. A time-of-flight spoiled gradient sequence with a short echo time is used. Conventionally, CE-MRA is not an electrocardiographic-gated technique but ideally is performed as the breath is held. Recently the free-breathing time-resolved CE-MRA technique has proved to be feasible in children with a higher heart rate with use of a keyhole approach with parallel imaging.1
Magnetic Resonance Imaging for Congenital Heart Disease
Pulse Sequences
Functional Evaluation
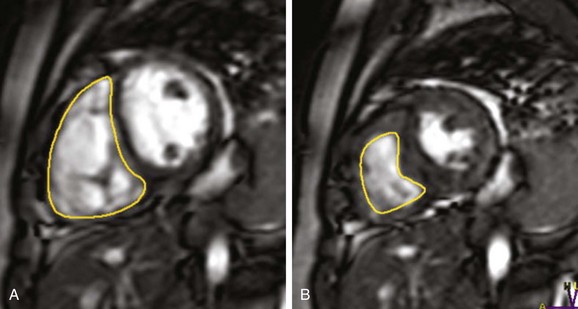
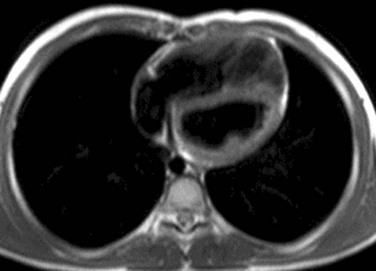
Endocardial contours are drawn on a short-axis steady-state free precession image of the right ventricle from base to apex in end-diastole (A) and end-systole (B) in a patient with a history of pulmonary stenosis after a pulmonary valvectomy and now with pulmonary regurgitation. The pulmonary regurgitant fraction was calculated to be 37% by right and left ventricular stroke volume differences.
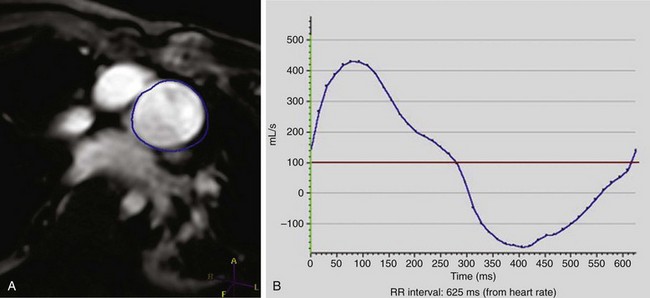
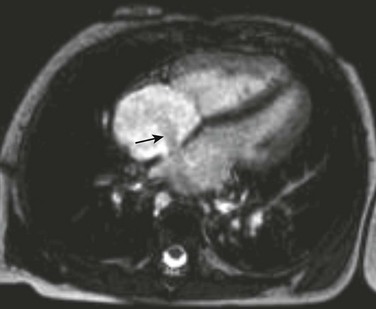
Phase contrast velocity mapping of the pulmonary artery in a 15-year-old with a history of tetralogy of Fallot after patch augmentation of the subpulmonary outflow tract obstruction. The blue region of interest is around the pulmonary outflow tract (A). The flow curve demonstrates moderate pulmonary regurgitation of 34% (B).
Magnetic Resonance Angiography
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Radiology Key
Fastest Radiology Insight Engine