Managing a Magnetic Resonance Imaging System
Objectives
At the completion of this chapter, the student should be able to do the following:
Key Terms
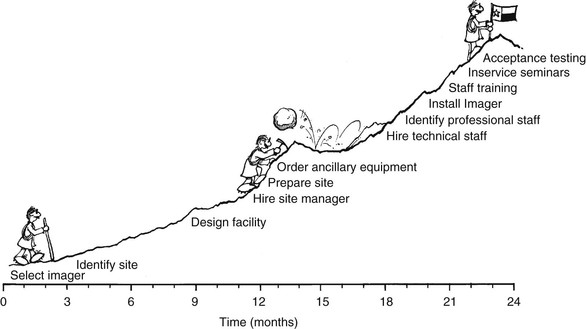
The time to begin preparing for the daily operation of a magnetic resonance imaging (MRI) facility is at least 1 year before the scheduled turnover date from the manufacturer. The reasons for this long planning time become clear as soon as all that needs to be accomplished before the first patient enters the magnet is considered. A fair amount of research and thought are required in producing a workable clinical environment (Figure 30-1).
For the establishment of a properly functioning MRI facility, the time from conception to operation may take up to 2 years. In Chapter 13, it is pointed out that the first step in this process is selection of the imaging system. Then, site selection and design of the facility are the next processes. Approximately 1 year before operation, attention should be focused on personnel, equipment, and administration.
First, all of the necessary ancillary equipment must be identified and purchase orders submitted. Then, a competent staff must be hired and sufficient time allowed for adequate training of these new employees. Staff scheduling must be arranged and imaging protocols established; service and safety arrangements are also necessary.
Ancillary Equipment
Routine daily magnetic resonance (MR) operations require a certain level of ancillary equipment support. As patient care becomes more and more intense, such as with sedation or anesthesia, ancillary equipment becomes more sophisticated.
Considerable thought should be given to services that will be offered at a particular site, and then appropriate selection of equipment can be made. Box 30-1 lists the equipment necessary for the initial start-up and operation of most MRI systems. This list is offered as a planning guide.
Nonmagnetic equipment for use with an MRI system is now readily available from several suppliers. The primary materials used in such equipment are sturdy plastics, aluminum, wood, and high-grade stainless steel. Other metals and alloys are also nonmagnetic, but it is always best to check any large metal object with a small magnet before it enters the imaging room.
Nonmagnetic gurneys are available from many x-ray supply companies. Nonmagnetic stretchers are more difficult to find and considerably more expensive but are more versatile and adaptable because they have more options, such as a raised head and adjustable height. Nonmagnetic wheelchairs are also available, as are nonmagnetic intravenous poles and step stools.
Stainless steel or aluminum oxygen cylinders, holders, and respirators are required. The cylinders can be obtained from either a local gas supply company or the cryogen supplier. Specify that the tanks be labeled “nonmagnetic” and verify that replacement tanks are the same. A respirator that works in the magnetic field is primarily plastic with no metal gauges. The fittings should be nonmagnetic brass or aluminum.
Tools can be purchased from the MRI vendor or other companies that provide nonmagnetic supplies for research laboratories. Nonmagnetic fire extinguishers should be kept in the area to prevent any unfortunate accidents during an emergency; a local supply company should be consulted for this.
Apparatus is required for monitoring sedated patients, elderly patients, and any patient with impaired communication skills. One sedated patient each day is a representative average. Minimal patient monitoring requires nonmagnetic devices for assessing blood pressure, pulse rate, and blood oxygen level.
When considering the purchase of ancillary equipment, the administrator should not overlook the role played by small equipment in the front office area of a busy MRI facility. Today’s competitive world requires an electronic office for general communications and for prompt magnetic resonance (MR) report delivery and filing.
Human Resources
Staffing
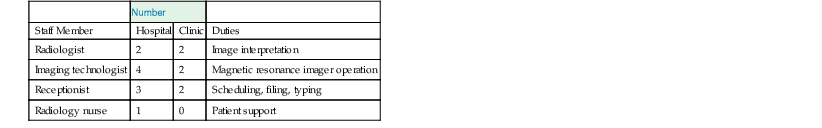
Staffing differs among facilities and also between a hospital and an imaging center. The number of staff depends principally on the patient load. Table 30-1 identifies a representative start-up staff for both a hospital and an imaging center.
After a few months of operation, it may be necessary to increase hours and days of imaging. Many MRI facilities eventually operate 18 hours a day, 6 days a week. This creates a great demand for MRI technologists and radiologists to perform complete diagnostic examinations in the most efficient and timely manner. It may be necessary to schedule staggered shifts rather quickly after start-up.
What training and experience should be required for MRI operation? Increasingly, more formal programs are available to train competent technical personnel, specifically in MRI. In addition, many continuing education seminars are offered. Training provided by MRI vendors is usually excellent but tailored to specific equipment.
Radiologic technologists with extensive experience in computed tomography (CT) are an obvious choice to be MRI technologists. Such individuals have already demonstrated competence as imaging technologists by completing a minimum 2-year training program and passing the examination of the American Registry of Radiologic Technologists (ARRT). Their experiences in patient care, patient positioning, anatomy, and computer operation can shorten the learning time required for operating an MRI system. Ultrasound and nuclear medicine technologists are also likely choices.
For the technical staff to develop the necessary competence to not only operate the MRI system but also exercise independent judgment about imaging techniques, they should receive appropriate continuing education. It is very important for MRI technologists to have a basic understanding of what occurs during MRI so that they can provide adequate physician assistance. Technologist certification in MRI by the ARRT is now required in keeping with appropriate standards of care.
The physical basis for MRI is totally different from that for x-ray imaging. Thought processes equating more dense tissue to white and less dense tissue to black on a radiograph cannot be applied to MRI. Thus MRI is much more complex. Technologists and physicians need to think in terms of signal intensity.
Strong signal intensity results in a bright image, and weak signal intensity results in a dark image. A complicating factor is that MR signal intensity can be completely reversed depending on the nature of the MRI pulse sequence.
Becoming comfortable with and understanding the physical principles of MRI are another matter. The technical staff must develop the necessary competence to exercise independent judgment about imaging techniques as they operate the MRI system. Each staff member must receive continuing education on a regular basis, with the support of a site administrator who remains committed to continuing education.
Scheduling
Experience has shown that approximately 30 to 45 minutes per examination should be allowed initially. Early experiments with radiofrequency (RF) pulse sequences and patient positioning require considerable time. However, with experience the average examination time can be shortened considerably. At that time, the scheduling of technologists can be somewhat altered. Fast imaging pulse sequences that shorten examination times considerably are now routine.
The extremely competitive market for MRI mandates the ability to offer same-day service and expeditious report turnaround time. It is not unusual for a patient to leave a site, having had the MRI examination completed, with a copy of the films and at least a preliminary report. The radiologist must be in a position of readiness to accommodate the referring physician by being available for consultation.
Patient scheduling should not be so tight that those who arrive on time must wait. In today’s competitive atmosphere, patients who arrive on time and are properly prepared should not have to wait.
Technologist Scheduling.
During the initial start-up phase, every aspect of the procedure is slow because of such factors as unfamiliarity with operating controls, difficulty in setting up imaging protocols, and selection of appropriate hard copies. Depending on the institution, this period lasts 1 to 6 months. The technologists should become involved and be a part of the final product. The entire department benefits from this interaction. Time and effort expended initially will bring rewards later.
Patient Scheduling.
Seldom should it be necessary to repeat an examination of a patient. This not only increases the workload but also disrupts the schedule. Nevertheless, reexamination is sometimes required because of an inability to complete the examination.
Occasionally, upon review of the images by the radiologist, the appearance of a questionable area requires reexamination. The patient is contacted, and additional imaging is carried out as soon as possible. In general, 15 to 30 minutes of image time can be expected. The patient should be handled carefully and should be made to feel as comfortable about the return visit as possible.
The magnet should not remain idle because of misinformation or scheduling inefficiency. All outpatients should be called the day before their scheduled examination for confirmation of appointment. At that time, staff should verify that patients know the time of their appointment and should give instructions and directions to the MRI facility. Time should be taken to answer questions or discuss fears patients may have. Such attention will help tremendously in ensuring their arrival on time.
It is helpful to schedule similar examinations back to back. If possible, separate segments of each day should be scheduled for head, body, and surface coil imaging. This eliminates the need for switching equipment or coils from patient to patient and saves considerable time. An efficient facility should strive to have the next patient enter the examination room as the previous patient exits.
Request Form.
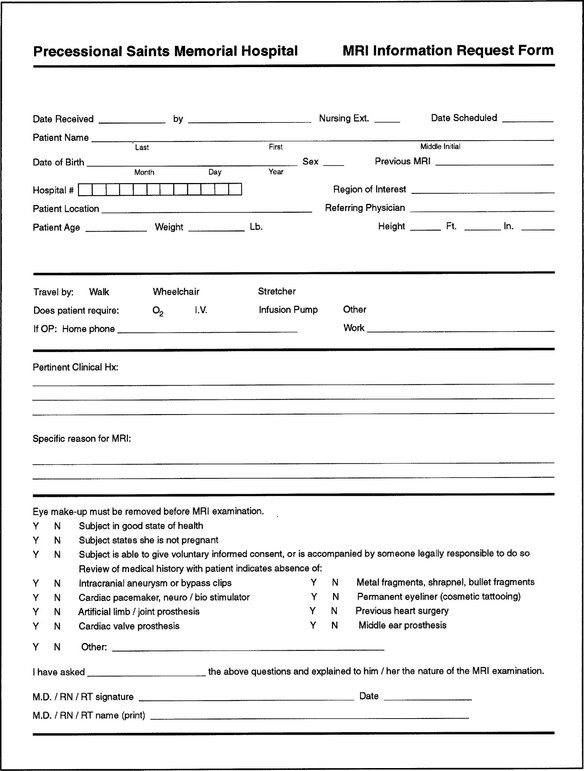
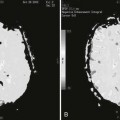
No patient should be examined without a proper request completed by the referring physician (Figure 30-2). As much medical information as possible should be provided with the request. In addition to giving standard identification data, the requesting physician should provide pertinent information from the clinical history of the patient and specific information about the reason for MRI.
In particular, the referring physician should be required to determine and state that the patient has no intracranial aneurysm or bypass clips, cardiac pacemaker, artificial limb, metal prosthesis, or metal fragments. If the presence of any such items is questionable, radiography or CT images should be obtained to confirm their absence. This should be done before the MRI procedure is scheduled.
Consent Form.
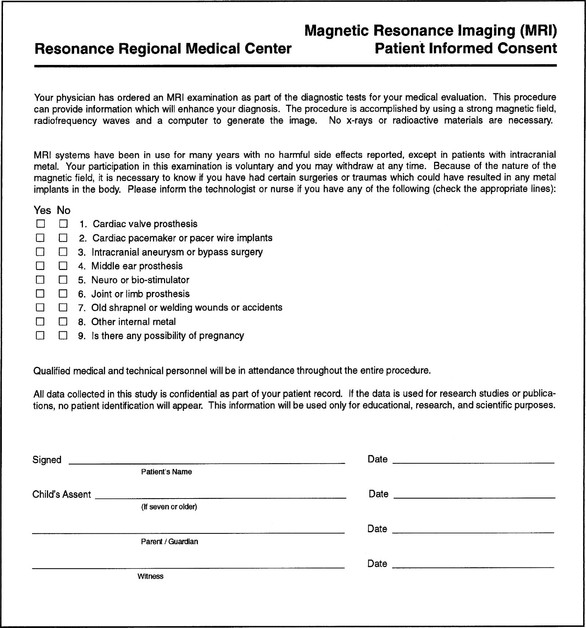
When any hardware or software of the MRI system is not approved by the Food and Drug Administration (FDA), the FDA requires that a consent form be obtained from each patient. Regardless, it is advisable to obtain a consent form from each patient. Figure 30-3 presents such an informed consent form. In addition to providing general information and identification, the form must state that the patient understands the nature of the examination and ensure that all the patient’s questions have been answered.
Of particular importance, the patient should be required to respond to the same questions posed to the clinician regarding clips, pacemakers, prostheses, and other metal devices. A basic explanation of MRI should be provided to the patient. A brief and clearly stated pamphlet would be sufficient. The patient should be made aware that MRI is a benign examination and that there are no adverse effects.
Patient Preparation.
Before the examination, the procedure should be explained and the patient told what the examination time will be and that it is important to remain still and relaxed.
The patient should be assured that the examination does not hurt but that loud thumping noises may be heard. Eating and drinking should be avoided for 2 hours before the examination for patient comfort for a standard MRI. Imaging the gallbladder and pancreatic ducts requires avoiding anything by mouth (n.p.o.) for 6 to 8 hours. The patient should be reminded that this is a diagnostic examination and not a treatment.
Image quality can be substantially improved and image artifacts significantly reduced if patients are properly screened and prepared for the MRI examination. Screening begins with pamphlets to educate the referring physicians, their staff, and patients.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree