, Gustav Andreisek2 and Erika J. Ulbrich2
(1)
Phoenix Diagnostic Clinic, Cluj-Napoca, Romania
(2)
Institute of Diagnostic and Interventional Radiology, University Hospital Zürich, Zürich, Switzerland
5.1 Anatomy and Normal MRI Appearance
The menisci and their insertions into bone represent a fibrocartilaginous functional unit [1]. Their function is to distribute loads and to protect the cartilage and the subchondral bone. They measure approximately 35 mm in diameter and are divided into anterior horn, posterior horn, and body of meniscus. Both menisci are hypovascular and contain mainly water and a dense elaborate type I collagen network with a predominantly circumferential alignment [1]. The vascular supply is provided by branches of lateral, medial, and middle genicular arteries. A perimeniscal capillary plexus originating in the capsular and synovial tissues of the joint supplies the peripheral 10–33 % of the menisci [2, 3]. Both menisci are interconnected and are separately attached to the capsule and anchored to the adjacent bone structures. The tibial attachment of the menisci are known as the meniscal root ligaments. On MR images menisci are seen as homogeneous low-signal intensity structures on all sequences (Fig. 5.1).
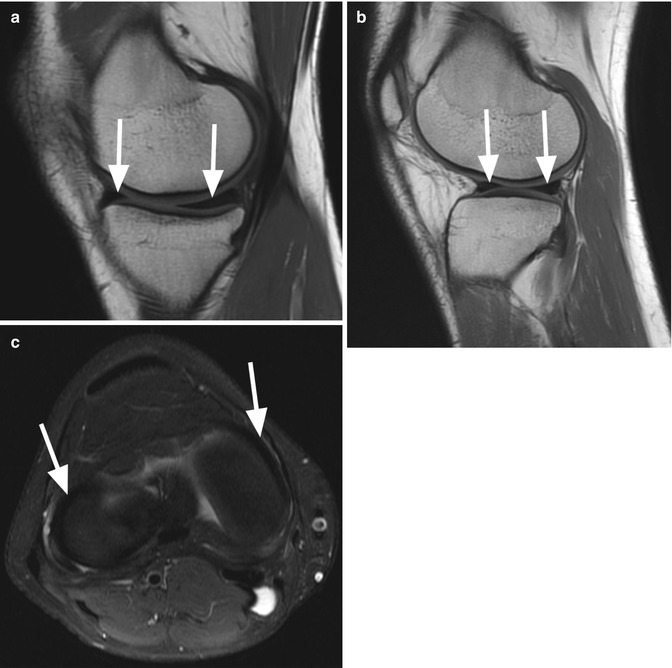
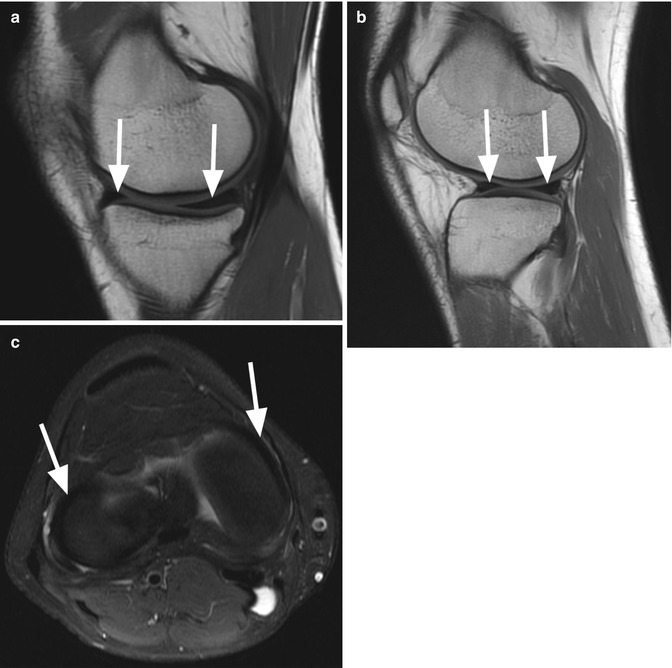
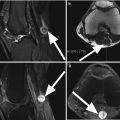
Fig. 5.1
Normal menisci in a 19 year old female. Sagittal proton-density (PD) FSE image through the medial compartment (a) shows the medial meniscus which is wider posteriorly than anteriorly (arrows). Sagittal proton-density (PD) FSE image through the lateral compartment (b) shows the normal homogeneous hypointense anterior and posterior horn of the lateral meniscus (arrows). A complete evaluation of the meniscus should include axial images as shown in the axial proton-density (PD) FSE fat-suppressed image (arrows in c)
5.1.1 Medial Meniscus
The medial meniscus has a more open C-shaped structure than the lateral meniscus, covers approximately 60 % of the corresponding tibial plateau and is wider posteriorly than anteriorly (Fig. 5.1) [1]. In a loaded, in vitro situation, 50% of the axial load in the medial compartment is absorbed by the medial meniscus [4].
Capsular Attachments
The medial meniscus is intimately attached to the knee capsule along its entire circumference. The meniscofemoral, the meniscotibial, and the meniscopatellar ligaments are the structures that defines the deep layer (layer 3) of the medial collateral ligament. The meniscofemoral ligament is seen on MR images as a thin band that originates from the superior margin of the body of the medial meniscus and inserts on the femoral condyle 1–2 cm above the joint line (Fig. 5.2) [5]. The meniscotibial ligament is shorter and connects the inferior margin of the medial meniscus to tibial cortex inferior to the joint line (Fig. 5.2) [5]. The meniscotibial ligament extends along the entire circumference of the posteromedial edge of the meniscus and further form the deepest layer of the capsule and is also called the coronary ligament or the meniscocapsular ligament. The patellomeniscal ligament is seen on MR images anteriorly from the medial meniscus to the patellar margin (Fig. 5.3) [6]. A small bursa, known as medial posterior femoral recess or medial gastrocnemius bursa separates the posterior horn of the medial meniscus from the joint capsule [7].
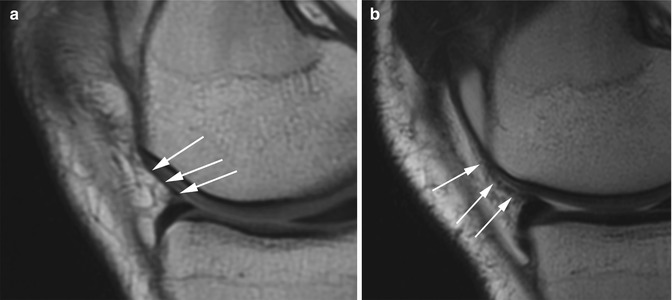
Fig. 5.2
Meniscofemoral and meniscotibial ligaments in a 22 year old male. Coronal proton-density (PD) FSE image shows the meniscofemoral ligament inserting on the femoral condyle and the superior margin of the body of the medial meniscus (large arrow) and the shorter meniscotibial ligament (small arrow) which connects the inferior margin of the medial meniscus to tibia. Both ligaments are structures of the deep layer of medial collateral ligament (curved arrow)
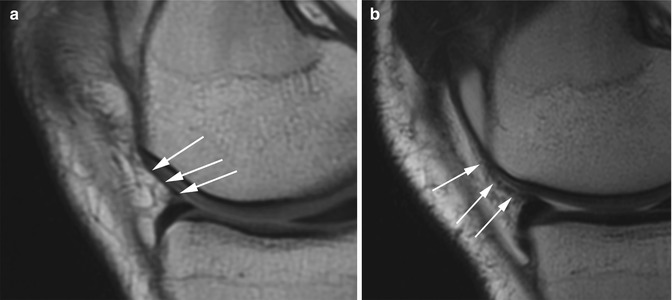
Fig. 5.3
Patellomeniscal ligament. Sagittal proton-density (PD) FSE images in a 22 year old male (a) and 19 year old female (b) show the patellomeniscal ligament (arrows) anteriorly, connecting the medial meniscus to the patellar margin. The ligament is hard to see on one image. Usually, dynamic view over multiple images is needed
Bone Attachments
The anterior and posterior horns are firmly attached to bone through the insertional ligaments known as the meniscal root ligaments. The tibial attachment of the anterior horn of the medial meniscus or the anterior medial root ligament is situated at the intercondylar fossa, 6–7 mm anteriorly to the anterior cruciate ligament (ACL) attachment (Fig. 5.4) [8]. The posterior medial root ligament attaches the posterior horn of the medial meniscus with the posterior intercondylar tibial fossa (Fig. 5.4). The attachment site is situated between the insertion of the posterior lateral root ligament and the insertion of posterior cruciate ligament (PCL) (Fig. 5.4) [1]. Both, the anterior and posterior ligaments, are larger that those of the lateral meniscus. The meniscal roots are defined on MR imaging as the last few millimeters of meniscal tissue angling down to the tibial plateau attachment in the intercondylar notch and are visible on axial, sagittal, and coronal planes (Figs. 5.4 and 5.5) [9].
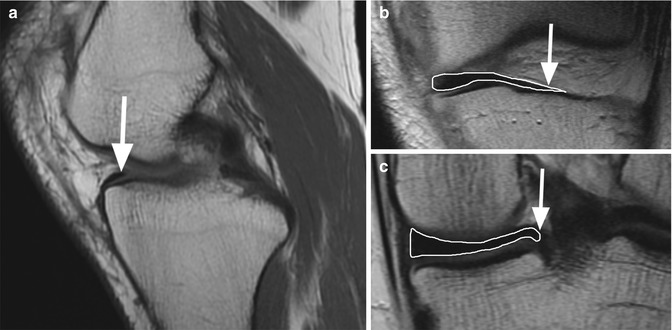
Fig. 5.4
Axial (PD) FSE image shows the anterior medial root ligament anteriorly to the anterior cruciate ligament. The posterior root of the medial meniscus is situated between the insertion of anterior cruciate ligament and the insertion of posterior cruciate ligament
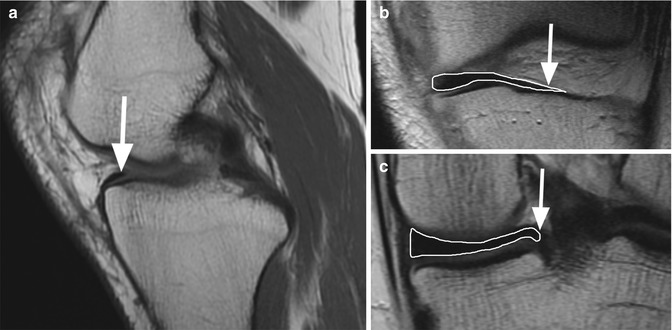
Fig. 5.5
The anterior and posterior medial roots ligaments. Sagittal proton-density (PD) FSE image (a) shows the anterior root ligament of the medial meniscus (arrow). Coronal proton-density (PD) FSE image (b) shows the most anterior segment of the anterior horn of the medial meniscus and enables the evaluation of its anterior root ligament (arrow). Coronal proton-density (PD) FSE image through the posterior knee joint (c) shows the posterior horn of the medial meniscus and its posterior root ligament (arrow)
Inconsistently, a medial anterior meniscofemoral ligament may be present connecting the anterior horn of the medial meniscus to the lateral wall of the intercondylar fossa of the femur [10].
Intermeniscal Connections
The anterior transverse ligament, also known as the geniculate ligament, connects the anterior horns of the medial and lateral meniscus. Medially the transverse ligament blends with the posterior attachment of the anterior medial root ligament. There is an association between the presence of a transvers ligament’s attachment and the presence of tears in the medial meniscus [11]. The ligament is inconsistently present and is best seen on sagittal and coronal MR images (Fig. 5.6) [12]. The posterior transverse ligament is much more rarely present than the anterior transverse ligament. It connects the posterior horns of the medial and lateral meniscus and is seen on MR images, when present, on coronal plane in front of the posterior cruciate ligament. Inconsistently, two oblique meniscomeniscal ligaments may be recognized on MR images [13]. The oblique ligaments extends from the anterior horn of the medial meniscus to the posterior horn of the lateral meniscus (medial oblique ligament) and from the anterior horn of the lateral meniscus to the posterior horn of the medial meniscus (lateral oblique ligament) (Fig. 5.7) [13].
Fig. 5.6
The anterior transverse ligament or the geniculate ligament. Sagittal proton-density (PD) FSE image (a), coronal proton-density (PD) FSE image (b), and axial (PD) FSE fat-suppressed image (c) show the ligament which connects the anterior horns of the medial and lateral meniscus (arrows)
Fig. 5.7
Axial (PD) FSE image shows the lateral oblique ligament (arrows) which connects the posterior horn of the medial meniscus (curved arrow) with the anterior horn of the lateral meniscus
5.1.2 Lateral Meniscus
The lateral meniscus is more circular O-shaped than the medial meniscus and covers 80 % of the corresponding tibial plateau [1]. Its width is constant from anterior to posterior. In a loaded, in vitro situation, 70% of the axial load in the lateral compartment is absorbed by the lateral meniscus [4]. The lateral meniscus is more mobile than the medial meniscus and, compared to the medial meniscus, has a loose attachment to the knee capsule and no attachment to the lateral collateral ligament.
Popliteomeniscal Fascicles (PMF)
The lateral meniscus is strongly attached to the popliteus tendon (PT) through the two popliteomeniscal fascicles (PMF) that are part of the posterolateral corner of the knee. On MR images the PMF are inconsistently seen as hypointense structures on sagital planes (Fig. 5.8) [14]. The posterosuperior PMF extends from the posterolateral aspect of the lateral meniscus to the PT (Fig. 5.8) and the anteroinferior PMF extends from the middle third of the lateral meniscus to the PT (Fig. 5.8). The anteroinferior PMF is stronger and shorter than the posterosuperior PMF [15, 16]. The PMF are situated around the popliteus bursa which is a synovial space adjacent to the posterior horn of the lateral meniscus [17, 18].
Fig. 5.8
The popliteomeniscal fascicles (PMF). Sagittal (PD) FSE image shows both ligaments. The posterosuperior PMF extends from the posterolateral aspect of the lateral meniscus to the popliteus tendon (large arrow). The anteroinferior PMF extends from the middle third of the lateral meniscus to the popliteus tendon (small arrow)
Bone and Capsular Attachments
The lateral meniscotibial ligament also known as the coronary ligament or the meniscocapsular ligament connects the lateral meniscus to the tibia along the entire circumference of the lateral meniscus.
The posterior horn of the lateral meniscus attaches to the medial femoral condyle through the meniscofemoral ligaments. The posterior meniscofemoral ligament (Wrisberg ligament) extends from the posterior horn of the meniscus to the medial femoral condyle proximal to the posterior cruciate (PCL) insertion (Fig. 5.9). The anterior meniscofemoral ligament (Humphrey ligament) attaches on the medial femoral condyle, inferior to the PCL insertion (Fig. 5.10). Many variations of these ligaments have been reported and the incidence of the presence of one or the other ligament is 70–100 % [19].
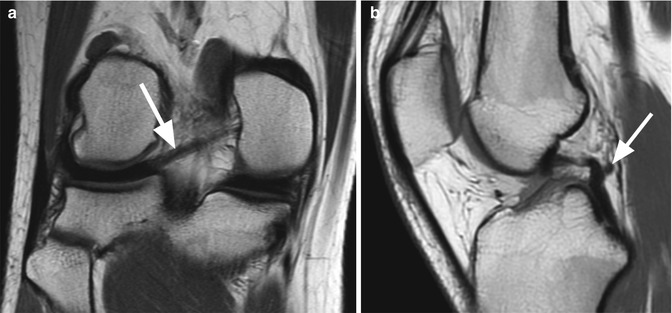

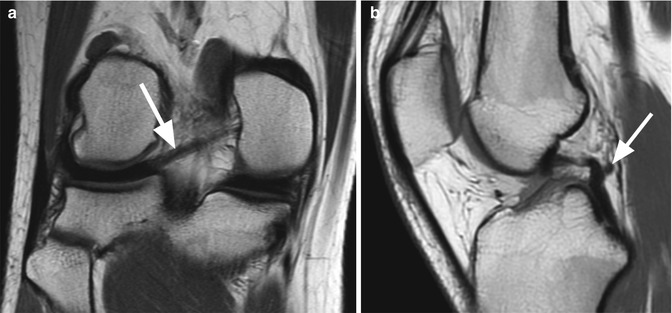
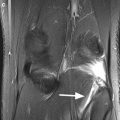
Fig. 5.9
Posterior meniscofemoral ligament (Wrisberg ligament). Coronal proton-density (PD) FSE image (a) and sagittal proton-density (PD) FSE image (b) show the posterior meniscofemoral ligament (arrow). On the coronal image (a) the entire length of the ligament is visualised

Fig. 5.10
Anterior meniscofemoral ligament (Humphrey ligament). Coronal proton-density (PD) FSE image (a) and sagittal proton-density (PD) FSE image (b) show the anterior meniscofemoral ligament (arrow)
The lateral meniscus is attached to the tibia by the lateral root ligaments. The anterior lateral meniscal root ligament attaches the anterior horn of the lateral meniscus to the lateral intercondylar tibial eminence just behind the anterior cruciate ligament (ACL) insertion (Figs. 5.11 and 5.12) [1]. The posterior root ligament of the lateral meniscus attaches posterior to the lateral intercondylar tibial eminence anterior to the posterior root ligament of the posterior horn of the medial meniscus (Figs. 5.11 and 5.12).
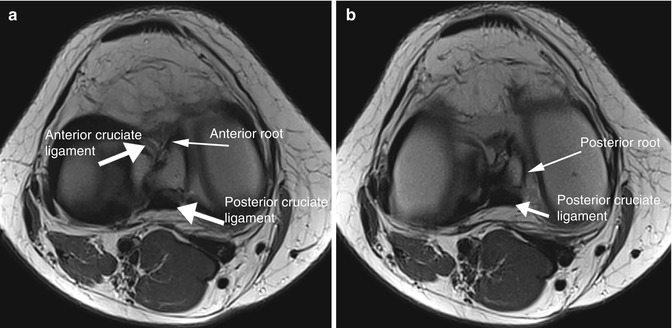
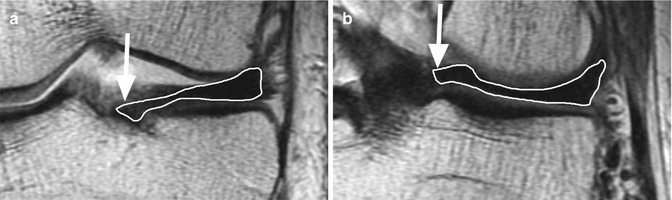
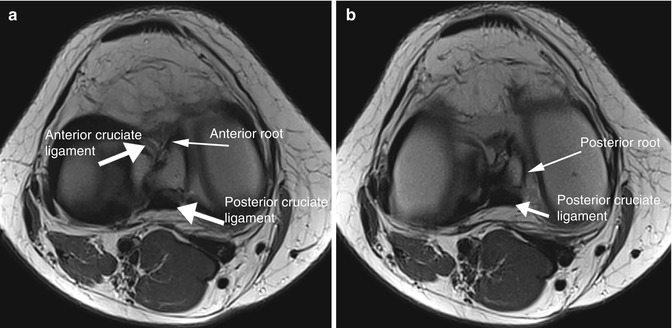
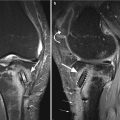
Fig. 5.11
Two consecutive axial (PD) FSE images show the anterior lateral root ligament which inserts posteriorly to the anterior cruciate ligament (a) and the posterior root of the lateral meniscus which inserts near the posterior cruciate ligament (b)
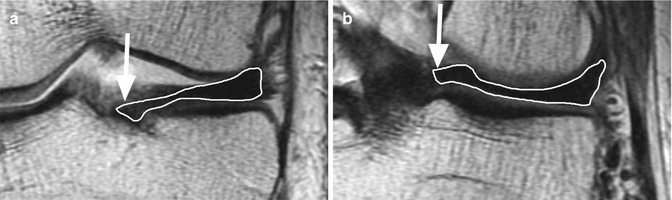
Fig. 5.12
The anterior and posterior lateral roots ligaments. Coronal proton-density (PD) FSE image (a) shows the most anterior segment of the anterior horn of the lateral meniscus and enables the evaluation of its anterior root ligament (arrow). Coronal proton-density (PD) FSE image through the posterior knee joint (b) shows the posterior horn of the lateral meniscus and its posterior root ligament (arrow)
A meniscofibular ligament was described connecting the lateral meniscus to the proximal fibula [20]. This ligament is located anterior to the popliteus tendon and is intra-capsular.
5.1.3 Normal Variants – Meniscal Flounce
The medial meniscal flounce is a normal positional variant characterized by a single symmetric fold along the free edge of the meniscus [21, 22]. The flounce is less commonly seen on MRI compared to arthroscopy and is considered it to be the result of traction of the medial meniscus during tibial rotation [22]. In these cases, the flounce is a transient finding and it may disappear during maximal knee extension or flexion [22]. On MR images the body of the medial meniscus shows a wavy, irregular S-shaped along the free margin of the meniscus on sagittal planes (Fig. 5.13). A similar appearance may be seen in patients with knee instability or joint effusion when the flounce can be also seen in the lateral meniscus. Although, the meniscal flounce is a rare anatomic variant, its presence should be recognised since a meniscal tear or a discoid meniscus may resemble same appearance (Fig. 5.14). However, meniscal flounce and meniscal tears may coexist.
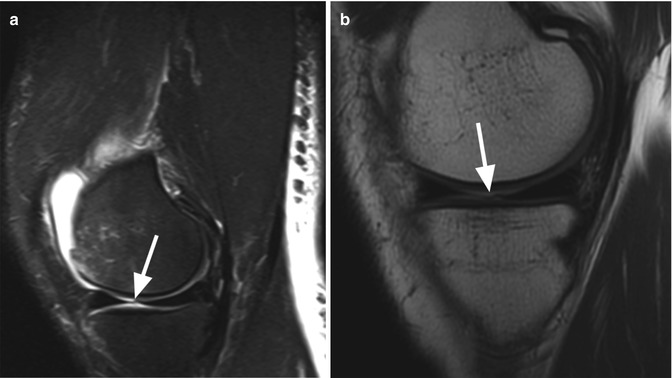
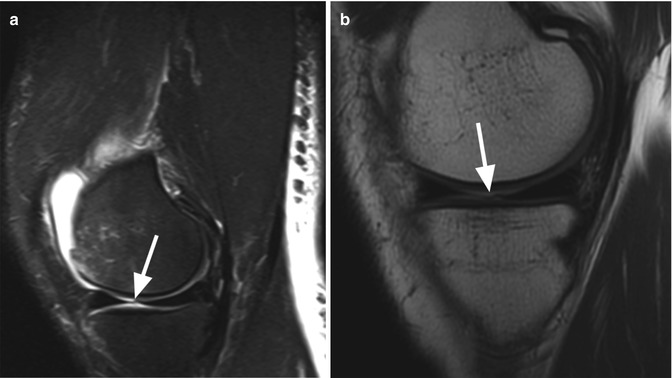
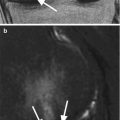
Fig. 5.13
Two different patients with internal meniscal flounce. Sagittal proton-density (PD) FSE fat-suppressed image (a) in a 23 year old patient and sagittal proton-density (PD) FSE image (b) in a 22 year old patient show in both cases a wavy, irregular meniscal contour of the meniscus (arrows)
Fig. 5.14
Differential diagnosis between meniscal flounce and meniscal tear. In the cases of irregular margins of the meniscus on sagittal images a meniscal tear can be easily mistaken for meniscal flounce. Therefore the coronal images should be carefully evaluated. Coronal proton-density (PD) FSE fat-suppressed image in a 18 year old male shows a bucket-handle tear of the medial meniscus (arrow) which presents with a wavy contour of the meniscus
5.2 MRI Pathological Findings
5.2.1 Discoid Meniscus
A discoid meniscus is a congenitally tall and elongated meniscus that can be symmetrically or asymmetrically increased in size [23]. The lateral discoid meniscus is more common (incidence of 0.4–16.6 %) than the medial discoid meniscus (incidence of 0.3 %) [24]. There are three types of discoid meniscus: complete, incomplete, and the Wrisberg type [25]. The complete and incomplete variants describe the shape of the meniscus with the incomplete type having a more semilunar shape. Both types, complete and incomplete discoid meniscus, are stable due to a normal posterior capsular and tibial attachment. The Wrisberg discoid meniscus is unstable and the only posterior attachment is the posterior meniscofemoral ligament of Wrisberg with a deficient posterior root meniscotibial ligament [26]. Clinically, patients can be asymptomatic or may complain of pain, swelling, clicking, and snapping especially in Wrisberg type due to the hypermobility of the meniscus. The MR imaging diagnosis of discoid meniscus is mainly based on the meniscus width and not on the meniscus height since it has been demonstrated that the accuracy of the meniscus height of the discoid meniscus is low [24]. Taking into consideration that the normal meniscus width is 14 mm measured on central slices, the diagnosis of discoid meniscus is suggestive when on sagittal images a continuity between the anterior and posterior horn is seen on four or more continuous slices (3 mm slice thickness) (Fig. 5.15) [27, 28]. The coronal images through the middle joint are more accurate and show an abnormally wide meniscus (>15 mm) (Fig. 5.16) [28]. The discoid meniscus may extend into the intercondylar notch in the complete type (Fig. 5.17) or may be seen in a normal position in the incomplete discoid type [29]. In the Wrisberg type, in the absence of the meniscotibial and posterior capsular attachment, an increased T2 signal intensity may be present between the capsule and the meniscus, simulating a peripheral tear [26]. Regardless the type, a discoid meniscus is prone to degeneration and tears (Figs. 5.18 and 5.19).
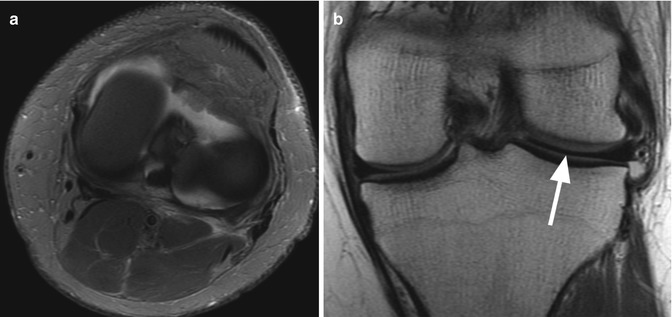


Fig. 5.15
Lateral discoid meniscus in a 39 year old female. Five consecutive sagittal proton-density (PD) FSE image (a–e) using 3 mm slice thickness show a continuity between the anterior and posterior horn (arrow)
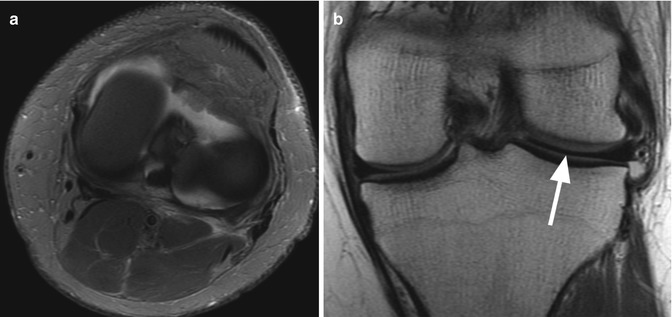
Fig. 5.16
Discoid meniscus – stable type. Axial (PD) FSE fat-suppressed image (a) shows an enlarged meniscus that can be identified entirely on axial plane (circles). Coronal proton-density (PD) FSE image (b) through the meniscus (line in a) shows an abnormally wide meniscus (>15 mm) at this level (arrow in b)

Fig. 5.17
Discoid meniscus in the intercondylar notch in a 39 year old female. Coronal proton-density (PD) FSE fat-suppressed image (a) and sagittal proton-density (PD) FSE image (b) show an enlarged meniscus extending into the intercondylar notch (arrow)
Fig. 5.18
Degenerative changes of lateral discoid meniscus in a 41 year old female. Sagittal proton-density (PD) FSE image show intrameniscal diffuse degenerative changes of the anterior and posterior horn (arrows)

Fig. 5.19
Multiple tears of lateral discoid meniscus in a 31 year old female. Two consecutive sagittal proton-density (PD) FSE images (a, b) show vertical longitudinal tear (arrow in a) as well as horizontal tear (arrow in b)
5.2.2 Meniscal Avulsion
Meniscal avulsion or the “floating” meniscus is defined as the detachment of the meniscus from the tibial plateau without separating completely from the capsule [30]. Typically, the lesion is limited to the meniscotibial ligaments (coronary ligaments) while the meniscofemoral ligaments remain intact [31]. In the setting of acute trauma the meniscotibial ligaments may become disrupted and the meniscus is avulsed from the tibial plateau without evidence of tear within the substance of the meniscus [31]. The medial meniscus is more frequently involved than the lateral meniscus [30]. On MRI, the meniscal avulsion is best evaluated on sagittal and coronal T2-weighted images and on MR arthrography. The presence of high-intensity fluid of greater than 3 mm thickness in the long axis between the meniscus and the tibial plateau is suggestive for meniscal avulsion (Fig. 5.20) [31].
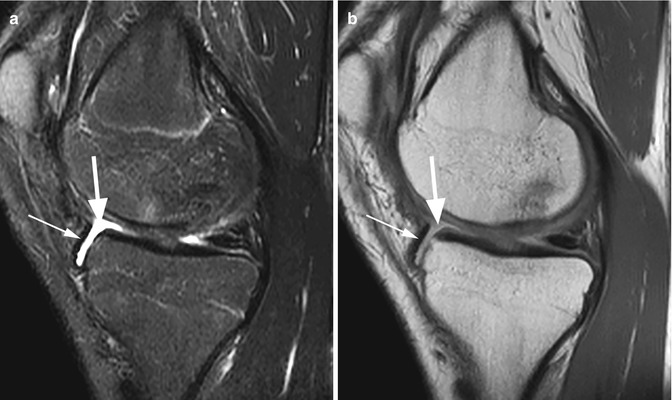
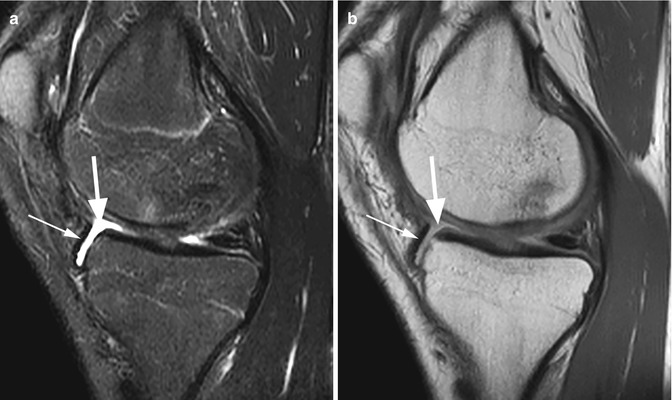
Fig. 5.20
Meniscal avulsion in a 19 year old male with acute trauma. Sagittal T2-weighted fat-suppressed image (a) and sagittal proton-density (PD) FSE image (b) show the presence of an abnormal volume of fluid anteriorly between tibia and femur (large arrows) with the anterior horn of the meniscus displaced anteriorly (small arrows)
5.2.3 Meniscal Extrusion
Meniscal extrusion is considered when the meniscus is displaced beyond the tibial margin [32]. Meniscal radial and oblique tears, meniscal roots tears, meniscal degeneration, cartilage defects and the absence of the meniscofemoral ligaments are the most common causes of the radial expansion of the meniscus from the joint space. The meniscal tears as well as the meniscal roots tears alter the circumferential margin of the meniscus that resists radial displacement and permit the meniscal extrusion from the joint space [33]. The meniscal roots tears are strongly associated with meniscal extrusion especially in the medial compartment. There is also a significant association between all grades of meniscal degeneration and cartilage damage of the medial compartment and the medial meniscal extrusion (Fig. 5.21) [34]. A rare cause of meniscal extrusion may be the knee effusion when the extrusion is seen in the medial compartment as a result of the distention of the capsule that is firmly attached to the medial meniscus [35]. Recognising the meniscal extrusion is of clinical importance since it may lead to development of osteoarthritis. On coronal MR images the extrusion is assessed between the tibial margins (excluding osteophytes) and the outer margin of the lateral or medial meniscus (Fig. 5.21) [34]. A distance of more than 3 mm for the medial meniscus and more than 1 mm for the lateral meniscus is considered abnormal [9].
Fig. 5.21
Medial meniscal extrusion in a 56 year old female with osteoarthritis. Coronal proton-density (PD) FSE image shows that the meniscal margin is beyond the tibial plateau (arrow). Note the intrameniscal degenerative changes
5.2.4 Meniscocapsular Separation
Meniscocapsular separation is the result of the disruption of the capsular attachment of meniscus. The lesion can occur at the meniscocapsular junction or within the peripheral zone of the meniscus. Because of the strong fixation of the medial meniscus, tears of the meniscotibial or the coronary ligaments, especially of the posterior horn, are more frequently compared to the lateral meniscus. Coronal and sagittal T2-weighted MR images are particularly useful in demonstrating the lesion (Figs. 5.22 and 5.23). The presence of fluid with an increased distance between medial collateral ligament and medial meniscus, the displacement of meniscus from tibia, tear within the peripheral zone of meniscus, and irregular meniscal margins are the best predictors of medial meniscocapsular separation (Fig. 5.22) [36]. Laterally, a displaced meniscus and the disruption of the popliteomeniscal fascicles with high-signal intensity edema in the posterolateral corner of the knee are suggestive for lateral meniscocapsular separation [37]. Perimeniscal fluid may be also present in medial or lateral meniscocapsular separation (Fig. 5.23).
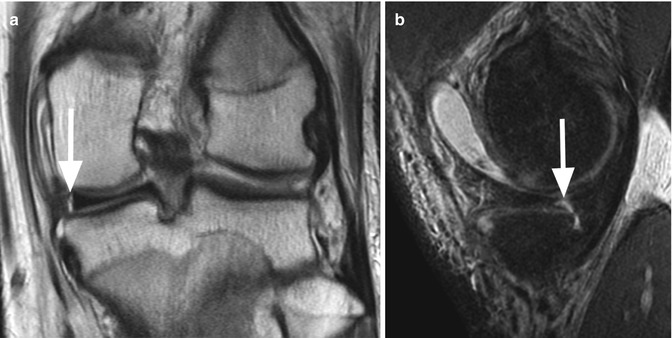
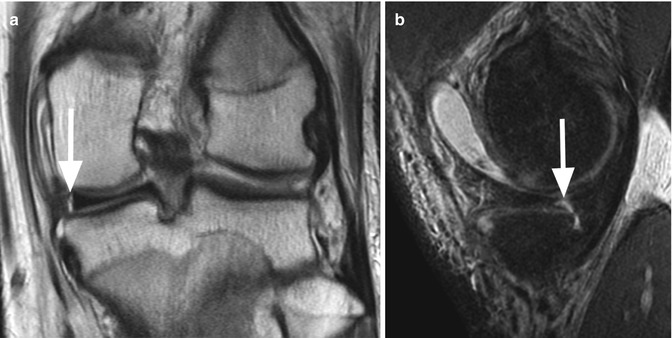
Fig. 5.22
Medial meniscocapsular separation in an 18 year old male. Coronal proton-density (PD) FSE image (a) and sagittal proton-density (PD) FSE fat-suppressed (b) images show a linear high-signal intensity separation between the peripheral zone of meniscus and the medial collateral ligament (arrow in a). The lesion is also visible on the sagittal image as a peripheral vertical tear of the posterior medial meniscus (arrow in b)
Fig. 5.23
Lateral meniscocapsular separation in a 51 year old male. Coronal proton-density (PD) FSE fat-suppressed image shows perimeniscal hematoma (arrow) between the lateral meniscus and the lateral collateral ligament suggestive for meniscocapsular separation
5.2.5 Degenerative Changes
The degenerative meniscal changes are the result of the internal derangement of the normal meniscal architecture followed by intrasubstance mucoid degeneration. It is frequently seen in elderly but it can appear at younger ages in response to high mechanical loading. The degenerative changes involve more frequently the posterior horn of the medial meniscus and are usually asymptomatic. On MR images the lesion appears as diffuse or focal increased signal intensity changes surrounded by normal low-signal intensity of the normal meniscal substance (Fig. 5.24). The degenerative lesions do not extend to the articular surfaces of the meniscus [29]. However, in some cases the free margin may display irregularities and the mucoid changes may progress to horizontal tears. When the linear changes do not convincingly extend to the articular surface, it is better to be descriptive rather than overdiagnose an equivocal finding [29].
Fig. 5.24
Degenerative intrasubstance mucoid degeneration of the posterior horn of the lateral meniscus in a 54 year old male. Sagittal proton-density (PD) FSE image shows a focal signal-intensity change within the meniscus (arrow). The lesion does not extend to the articular surfaces of the meniscus
5.2.6 Meniscal Contusion
Meniscal contusion appears in the setting of acute trauma and it usually involves the meniscal surface [38]. Bone injury adjacent to the meniscal contusions have been described in these patients suggesting that the mechanism of these lesions may be a compressive injury [38]. Meniscal contusion is seen on MR images as a diffuse, amorphous area of abnormal signal intensity that extends to the articular surface (Fig. 5.25). The signal does not meet the definite linear pattern of a meniscal tear neither the well-defined intrameniscal signal of the mucoid degeneration. At arthroscopy these lesions do not have the appearance of typical meniscal tears [38]. On MR imaging follow-up the meniscal contusion may resolve or improve suggesting the transient character of the contusion [38].
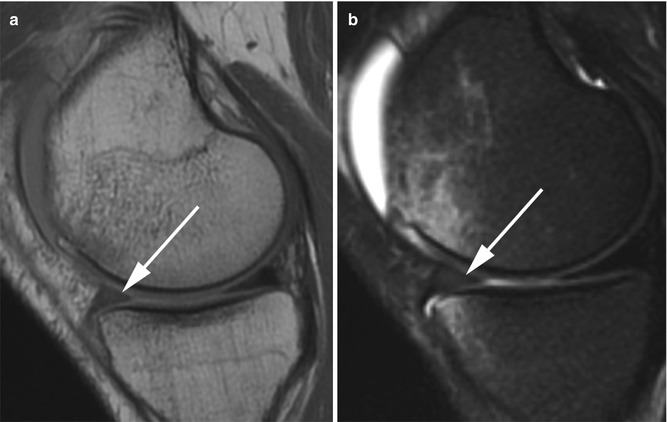
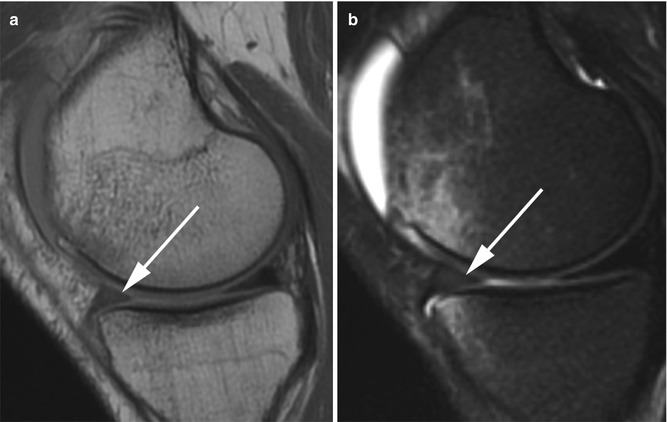
Fig. 5.25
Meniscal contusion in a 32 year old male with knee injury. Sagittal proton-density (PD) FSE image (a) and sagittal proton-density (PD) FSE fat-suppressed image (b) show diffuse signal intensity changes in the anterior horn of the medial meniscus that extends to the articular surface (arrows). Note the bone marrow contusion of the medial femoral condyle
5.2.7 Meniscal Tears
The meniscal tear is described as a linear increased signal intensity within the meniscus. The MR report should not only identify the presence of a linear meniscal tear but also should accurately describe the orientation, location, length and stability, because these criteria are important and may influence the choice of operative or nonoperative treatment. The classifications of meniscal tears is based on different criteria (Table 5.1). According to the orientation, a meniscal tear can be vertical, horizontal, or complex. Vertical tears are further subdivided into radial (perpendicular to the long axis of the meniscus), which includes the tears of the meniscal root and longitudinal (parallel to the long axis of the meniscus) [29]. The complex tears refer either to a combination of more orientations (vertical and horizontal) including the parrot beak tear and tears with displaced fragments (bucket-handle tear, flap meniscus tear, or free meniscus fragment). Meniscal grading (grade I–III) that has been widely used in the past is now considered obsolete in the clinical routine imaging [41].
Meniscal tear | Vertical | Longitudinal | Incomplete | Stable | Low clinical relevance, not always correlated with symptoms = “leave alone” lesion |
Complete | Unstable when meniscocapsular separation is present or in extensive lesion | High clinical relevance | |||
Radial | Without meniscal root involvement | Usually unstable | High clinical relevance | ||
Radial meniscal root tear | |||||
Horizontal or oblique-horizontal | Incomplete | Stable | Low clinical relevance, not always correlated with symptoms = “leave alone” lesion | ||
Complete | Unstable/stable | Different clinical relevance depending on associated lesions | |||
Complex
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

| |||||