Fig. 24.1
(a, b) Extraskeletal chondroma of the foot in a 37-year-old man: (a) plain radiograph; (b) CT. Soft tissue mass with multiple punctate and ringlike calcifications between the second and third toes (a). Calcifications are better demonstrated on CT (b). Localization in the forefoot and presence of characteristic calcifications are suggestive of extraskeletal chondroma

Fig. 24.2
(a, b) Extraskeletal chondroma below the right patella in a 54-year-old woman: (a) plain radiograph; (b) CT at the level of the proximal tibia; plain radiograph and CT show a pronounced, dense calcification at the periphery of the mass (a, b)
Imaging
On plain radiography and CT, an extraskeletal chondroma presents as a well-demarcated soft tissue mass. Calcifications are observed in 33–77 % of cases [6, 16, 33]. The pattern of calcification is most typically that of curvilinear, ringlike densities, outlining the soft tissue lobules. Less commonly, these calcifications may also be punctate or mixed punctate and curvilinear or rim-like [16, 33] (Figs. 24.1 and 24.2). Ossification is less common [16]. In longstanding cases, the tumor can cause cortical pressure erosion and reactive cortical sclerosis on an adjacent bone [6, 16, 33].
On MRI, soft tissue chondromas appear on T1-weighted images as well-circumscribed masses that are isointense relative to skeletal muscle. On T2-weighted images the hyaline cartilage typically presents with very high signal intensity (Fig. 24.3). Mineralized areas cause foci of signal void on all sequences [16]. Diagnosis of chondromas without foci of calcification is more difficult, and these lesions have to be differentiated from other soft tissue masses, especially those of synovial origin. After intravenous injection of gadolinium the majority of chondromas exhibit marked and mostly peripheral contrast enhancement (Figs. 24.3 and 24.4).



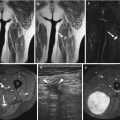
Fig. 24.3
(a–d) Soft tissue chondroma of the finger in a young woman: (a) coronal spin-echo T1-weighted MR image; (b) coronal spin-echo T2-weighted MR image; (c) transverse spin-echo T1-weighted MR image; (d) transverse spin-echo T1-weighted MR image after gadolinium contrast injection (same level as in c). Lobulated soft tissue mass near the radial aspect of the proximal third of the basic phalanx of the fourth finger. On T1-weighted image the mass presents with homogeneous low intensity (a, c). T2-weighted image reveals very high signal intensity of the matrix of the lesion, with internal low-intensity linear structures, corresponding to septations separating the cartilaginous lobules (b). Gadolinium-enhanced T1-weighted images show pronounced ringlike enhancement at the periphery of the lesion (d)

Fig. 24.4
(a–c) Extraskeletal osteochondroma at the popliteal fossa: (a) sagittal spin-echo T1-weighted MR image with fat suppression; (b) sagittal spin-echo T1-weighted MR image with fat suppression after gadolinium contrast injection; (c) axial spin-echo T2-weighted MR image with fat suppression. Rounded soft tissue mass at the popliteal fossa. The central region of signal void corresponds to extensive calcification, as observed in extraskeletal osteochondroma. The periphery of the lesion is slightly hyperintense to muscle and fat on fat-suppressed T1-weighted images (a), markedly hyperintense on fat-suppressed T2-weighted images (c), and shows pronounced enhancement following gadolinium contrast injection (b)
24.2.1.2 Synovial Osteochondromatosis
Definition
Synovial osteochondromatosis (SC) is characterized by the formation of numerous metaplastic cartilaginous or osteocartilaginous nodules of small size, within the joint (Figs. 24.5, 24.6 and 24.7), tendon sheath (Fig. 24.8) [6, 20, 28], or bursa [18]. Although the lesion has an intimate relationship with the synovium, it is currently classified as a neoplastic lesion of bone rather than soft tissue according to the WHO Classification of Tumours of Soft Tissue and Bone [8].





Fig. 24.5
(a–b) Primary (a) and secondary (b) synovial chondromatosis of the hip in two different patients: (a) plain radiograph of the right hip in a 36-year-old woman. Notice the presence of rice grain-like ossified nodules in the right hip joint. In primary synovial chondromatosis, the joint space is normal or can be even enlarged. Furthermore, the nodules are typically small and of uniform size in the primary form, whereas they are often larger and of heterogeneous size in the secondary form. (b) Plain radiograph of the left hip in a 41-year-old woman with a previous history of an acetabular fracture due to a motor vehicle accident. There are multiple ossified nodules in the left hip joint. Note marked protrusion of the acetabulum and central cartilage loss, in keeping with secondary posttraumatic synovial chondromatosis

Fig. 24.6
(a–d) Intra-articular synovial chondromatosis of the right hip joint in a 55-year-old woman: (a) coronal FS T2-WI of the pelvis shows joint effusion within the right hip and multiple hypointense intra-articular nodules. Note erosion at the lateral aspect of the right femoral neck (black arrow), (b–d) oblique coronal, axial, and sagittal MR arthrograms of the right hip confirming multiple intra-articular nodules, and an erosion at the lateral aspect of the right femoral neck (arrows in b and c)

Fig. 24.7
(a, b) Synovial chondromatosis of the elbow in a 21-year-old male: (a) plain radiograph (lateral view) showing two ossified nodules at the ventral aspect of the elbow joint (arrowheads). (b) Longitudinal ultrasound shows joint effusion and intra-articular loose bodies with retro-acoustic shadowing (arrows)

Fig. 24.8
(a, b) Tenosynovial chondromatosis of the finger in a 45-year-old male: (a) Plain radiograph (lateral view) showing calcified nodules at the flexor side of the proximal and middle phalanx of the finger. Note scalloping due to pressure erosion of the palmar cortex of the proximal and middle phalanx (black arrowhead). (b) On sagittal T2-WI, the lesions are of mixed signal. Area of low signal corresponds to calcifications, whereas high signal areas are due to hyaline cartilage. Note also scalloping of the palmar cortex of the proximal and middle phalanx (black arrowheads)
Two forms of SC are described in the literature. Primary SC is defined by subsynovial cartilage metaplasia, synovial hyperplasia, and production of similar-sized round cartilaginous nodules. The secondary form occurs as part of a preexisting joint disease, such as degenerative joint disease, arthritis, or trauma. In the secondary form, formation of nodules in the joint space is caused by the dislodgement of bony or cartilaginous tissue. These loose bodies undergo concentric layering of synovial cells, by which nourishment is provided. These nodules are more irregular and are often larger and of heterogeneous size compared to nodules of primary form [20]. Milgram proposed the following staging system [18]. In the initial stage, there is active synovial disease without loose bodies. The transitional stage is characterized by persistent synovial disease and formation of loose bodies, whereas in the third stage, detached intra-articular nodules varying from 1 mm to 10 mm are present, with burned-out intrasynovial disease. The nodules often detach and form loose bodies in the joint space. Approximately two-thirds of them calcify or ossify.
Rarely, the nodules are extra-articular. Chondrosarcoma arising in synovial chondromatosis has been reported but is uncommon [15].
Incidence and Clinical Behavior
Synovial osteochondromatosis commonly occurs in large joints, such as the hip (Figs. 24.5 and 24.6), knee, shoulder, ankle, or elbow (Fig. 24.7) [20], but small joints such as the metacarpophalangeal, interphalangeal, distal radioulnar, acromioclavicular, proximal tibiofibular joint, apophyseal joints, and temporomandibular joint may be involved as well [10, 20]. The clinical history is often characterized by joint pain of several years’ duration.
Imaging
Ultrasound may show a heterogeneous mass containing foci of hyperechogenicity, in keeping with chondral fragments or fronds of the synovium with underlying cartilage nodule formation. Posterior acoustic shadowing is seen in case of sufficient mineralization or enchondral bone formation (Fig. 24.7). Depending on the site involved, fragments may change in position during dynamic US examination [20]. Power Doppler sonography has been reported to reveal an avascular process [23].
MRI findings are an increased amount of joint fluid and intra-articular nodules (Fig. 24.6). In the early stage, nonspecific synovitis may be seen. Uncalcified osteochondromas are isointense relative to muscle on T1-weighted images and hypointense relative to synovial fluid. Calcified lesions, occurring in up to 77 % of cases, are seen as small, round signal voids. Ossified nodules may demonstrate signal intensities of fatty bone marrow. In joints that have a very tense capsule, such as the hip joint, synovial chondromatosis can cause erosions of the bone [20] (Fig. 24.6).
24.2.2 Malignant Chondro-osseous Soft Tissue Tumors
24.2.2.1 Mesenchymal Chondrosarcoma
Definition
Mesenchymal chondrosarcoma (MCS) is a biphasic, high-grade malignant neoplasm [4, 11] that presents on macroscopy as a multilobulated mass of variable size. On cross section, the tumor shows a mixture of gray-white tissue and foci of the cartilage and bone. On microscopy the tumor exhibits a proliferation of primitive round cells and interspersed small islands of well-differentiated hyaline cartilage [30].
Incidence and Clinical Behavior
Extraskeletal mesenchymal chondrosarcoma occurs less frequently than the myxoid variant. However, 30–50 % or half of all mesenchymal chondrosarcomas are extraskeletal in location, whereas the others are intraosseous [30]. There is a slight female predominance. A bimodal age distribution is noted and related to anatomic location. When occurring in the third decade of life, tumors are located mainly in the head or neck, often in the brain, meninges, and periorbital regions. Tumors arising in the fifth decade of life afflict preferentially the soft tissues (thigh) [30]. The mesenchymal chondrosarcoma has an aggressive behavior and frequently metastasizes to lungs, lymph nodes, and bones. The prognoses are variable, with a 10-year survival rate of nearly 27.3 % [4, 30].
Imaging
Calcifications within the tumor are common and well demonstrated by plain radiography and CT (Figs. 24.9 and 24.10). The degree and type of calcification are variable and range from ring and arcs, flocculent or stippled calcification, to dense mineralization [4]. In rare cases, the tumor involves underlying bone [11].



Fig. 24.9
(a, b) Extraskeletal mesenchymal chondrosarcoma of the right axilla in a 50-year-old man: (a) plain radiograph; (b) CT. Ill-defined mass with coarse intralesional calcifications located in the subscapular region (a, b). Calcifications are commonly seen in the mesenchymal type of extraskeletal chondrosarcoma

Fig. 24.10
(a, b) Extraskeletal mesenchymal chondrosarcoma of the buttock in a 32-year-old man: (a) plain radiograph; (b) CT; large calcified mass superior to the trochanter major (a). CT reveals a soft tissue component medially and the calcified component laterally within the mass (b). Findings on plain radiography and CT are indicative of a lesion of cartilaginous origin
On MRI, extraskeletal mesenchymal chondrosarcoma presents as a lobulated soft tissue mass, but further imaging appearance may be nonspecific. Signal intensity of the tumor equals that of muscle on T1-weighted images and is intermediate to high on T2-weighted images [11]. Following administration of gadolinium contrast, inhomogeneous enhancement is observed, especially at the periphery (Fig. 24.11). Areas of calcifications may be of low signal intensity [11].


Fig. 24.11




(a–d) Extraskeletal chondrosarcoma of the left pectoralis minor in 63-year-old female: (a) axial T2-weighted HASTE MR image; (b) axial FS T1-WI. (c) Axial and (d) sagittal FS T1-WI following administration of gadolinium contrast. T2-WI reveal the lobulated shape of the lesion with the cartilaginous lobules being markedly hyperintense contrasting with intralesional low-intensity septa. The lesion is isointense with muscle on T1-WI (b). Following administration of gadolinium, pronounced peripheral enhancement is observed (c, d)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree