Type of Arthritis |
Site |
Crucial Abnormalities |
Technique/Projection |
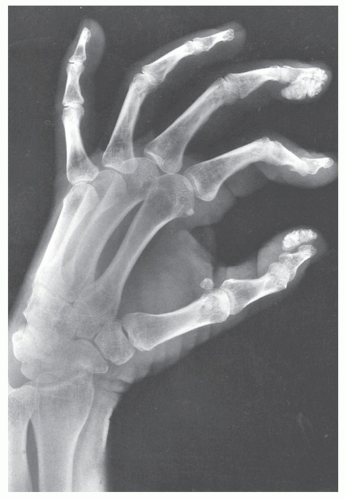
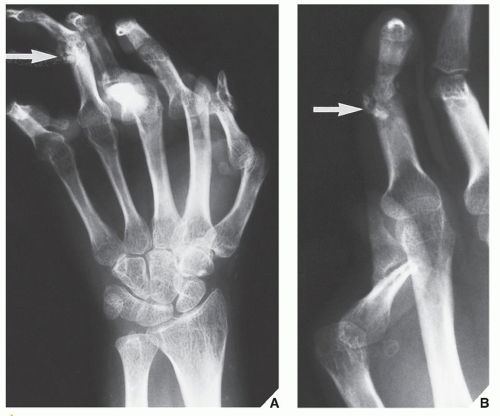
Gout (M > F) |
Great toe
Large joints (knee, elbow)
Hand |
Articular erosion with preservation of part of joint
Overhanging edge of erosion
Lack of osteoporosis
Periarticular swelling |
Standard views of affected joints |
|
|
Tophi |
Dual-energy color-coded CT |
CPPD crystal deposition disease (M = F) |
Variable joints |
Chondrocalcinosis (calcification of articular cartilage and menisci)
Calcifications of tendons, ligaments, and capsule |
Standard views of affected joints |
|
Femoropatellar joint |
Joint space narrowing
Subchondral sclerosis
Osteophytes |
Lateral (knee) and axial (patella) views |
|
Wrists, elbows, shoulders, ankles |
Degenerative changes with chondrocalcinosis |
Standard views of affected joints |
CHA crystal deposition disease (F > M) |
Variable joints, but predilection for shoulder joint (supraspinatus tendon) |
Pericapsular calcifications
Calcifications of tendons |
Standard views of affected joints |
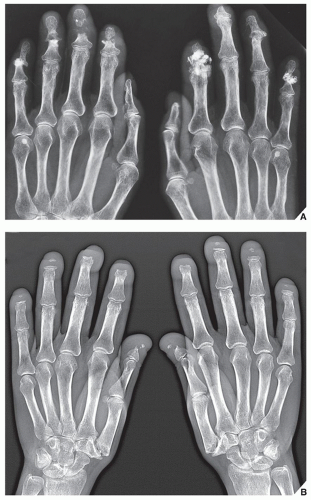
Hemochromatosis (M > F) |
Hands |
Involvement of second and third metacarpophalangeal joints with beak-like osteophytes |
Dorsovolar view |
|
Large joints |
Chondrocalcinosis |
Standard views of affected joints |
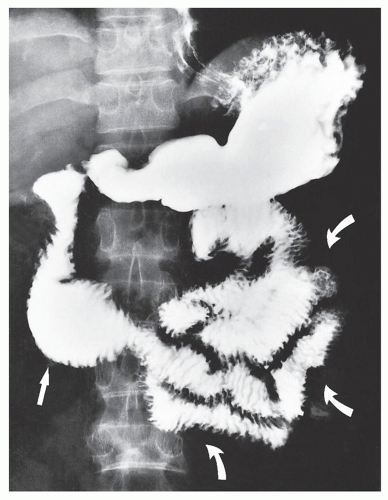
Alkaptonuria (ochronosis) (M = F) |
Intervertebral disks, sacroiliac joints, symphysis pubis, large joints (knees, hips) |
Calcification and ossification of intervertebral disks, narrowing of disks, osteoporosis, joint space narrowing, periarticular sclerosis |
Anteroposterior and lateral views of spine; standard views of affected joints |
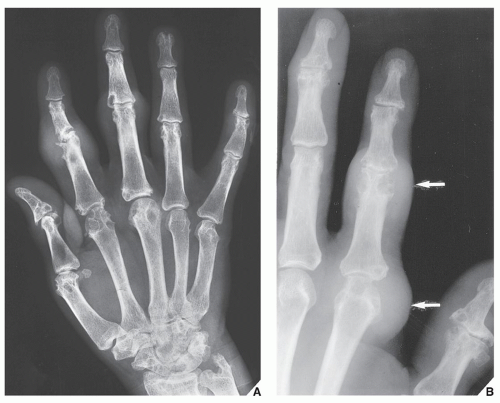
Hyperparathyroidism (F > M) |
Hands |
Destructive changes in interphalangeal joints
Subperiosteal resorption |
Dorsovolar view
Dorsovolar and oblique views |
|
Multiple bones
Skull
Spine |
Bone cysts (brown tumors)
Salt-and-pepper appearance
Rugger-jersey appearance |
Standard views specific for locations
Lateral view
Lateral view |
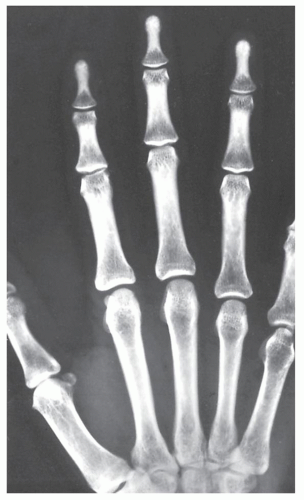
Acromegaly (M > F) |
Hands |
Widened joint spaces
Large sesamoid
Degenerative changes (beak-like osteophytes) |
Dorsovolar view |
|
Skull
Facial bones
Heel
Spine |
Large sinuses
Large mandible (prognathism)
Thick heel pad (>25 mm)
Thoracic kyphosis |
Lateral view
Lateral view
Lateral view
Lateral view (thoracic spine) |
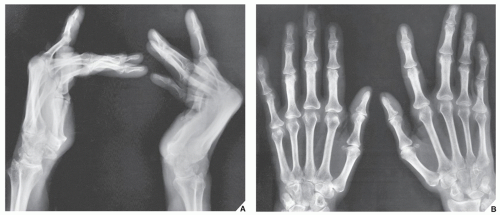
Amyloidosis (M > F) |
Large joints (hips, knees, shoulders, elbows) |
Articular and periarticular erosions, osteoporosis (periarticular), joint subluxations, pathologic fractures |
Standard views of affected joints
Radionuclide bone scan (scintigraphy) |
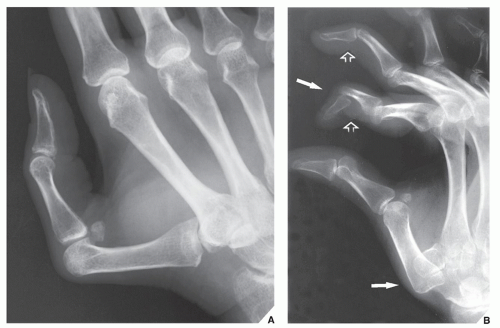
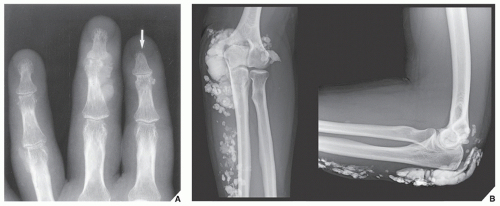
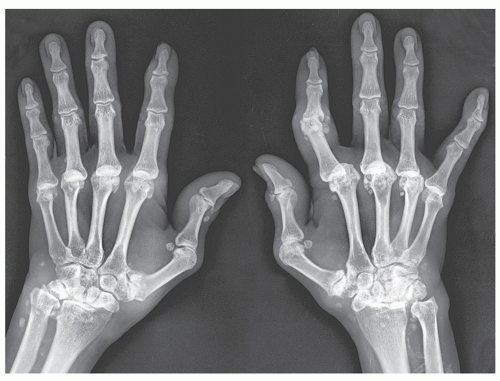
Multicentric reticulohistiocytosis (F > M) |
Hands (distal and proximal interphalangeal joints)
Feet |
Soft-tissue swelling, articular erosions, lack of osteoporosis |
Dorsovolar view
Norgaard (ball-catcher’s) view
Dorsoplantar view
Oblique view |
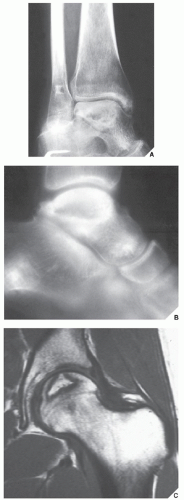
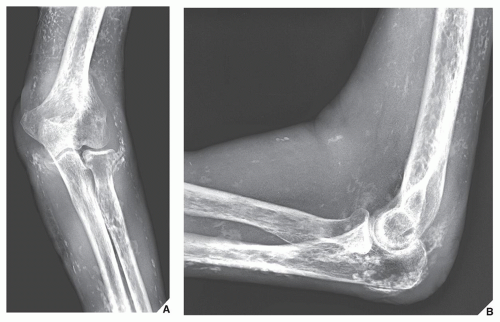
Hemophilia (M > F) |
Large joints (hips, knees, shoulders)
Elbows, ankles |
Joint effusion, osteoporosis, symmetrical and concentric joint space narrowing, articular erosions, widening of intercondylar notch, squaring of patella; very similar to changes of juvenile rheumatoid arthritis |
Standard views of affected joints
MRI |
M, male; F, female; CT, computed tomography; CPPD, calcium pyrophosphate dihydrate; CHA, calcium hydroxyapatite; MRI, magnetic resonance imaging. |