Fig. 16.1
Ground-glass opacity. Axial fat-suppressed fast spin-echo T2-WI (a) and axial free-breathing post-contrast fat-suppressed 3D GRE T1-WI (radial VIBE) (b). In the left lower lobe, a hazy opacity is depicted with high signal intensity on both sequences and without obscuring the bronchovascular markings
Consolidation due to infectious pneumonia (Fig. 16.2) is defined as a region of a normally compressible lung tissue that has been filled with liquid. On MR, consolidation is seen as areas of signal intensity that obscures the margins of vessels and airway walls and appears with high signal intensity on T2-weighted images (T2-WI) (Fig. 16.3), due to the high fluid content. Air bronchogram may be present. Air bronchogram appears as low signal areas following the course of the bronchi within the consolidation (Fig. 16.4). MRI may enable the differentiation of consolidation associated with fibrotic tissue due to the relatively short T2 component of fibrosis [17].
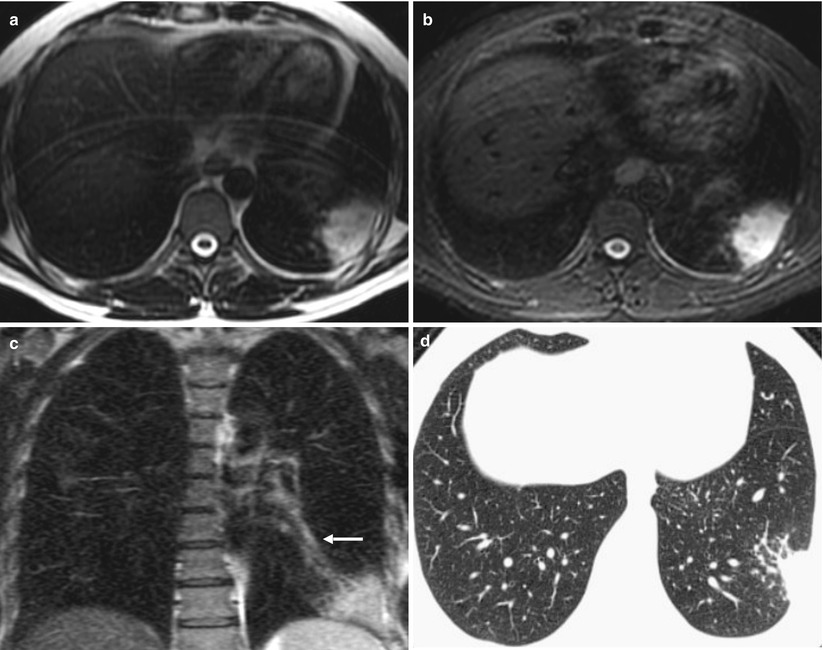
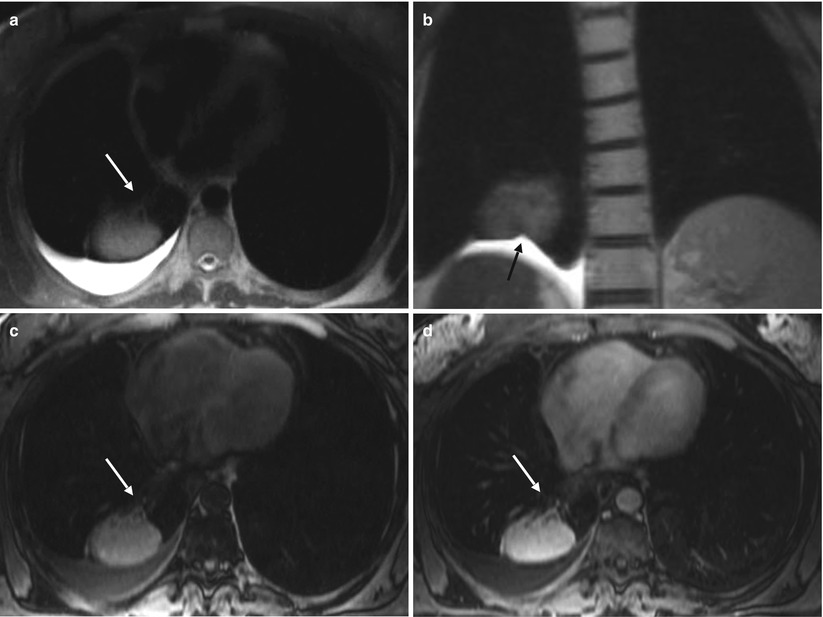
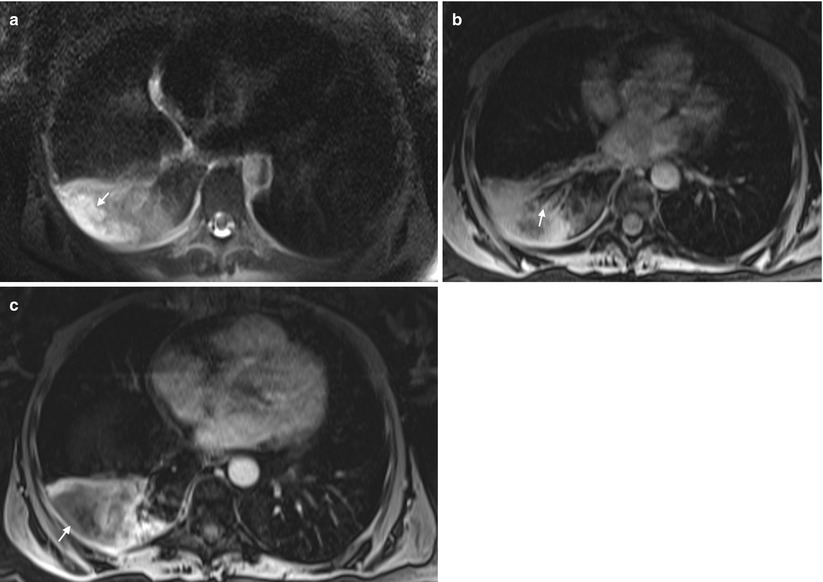
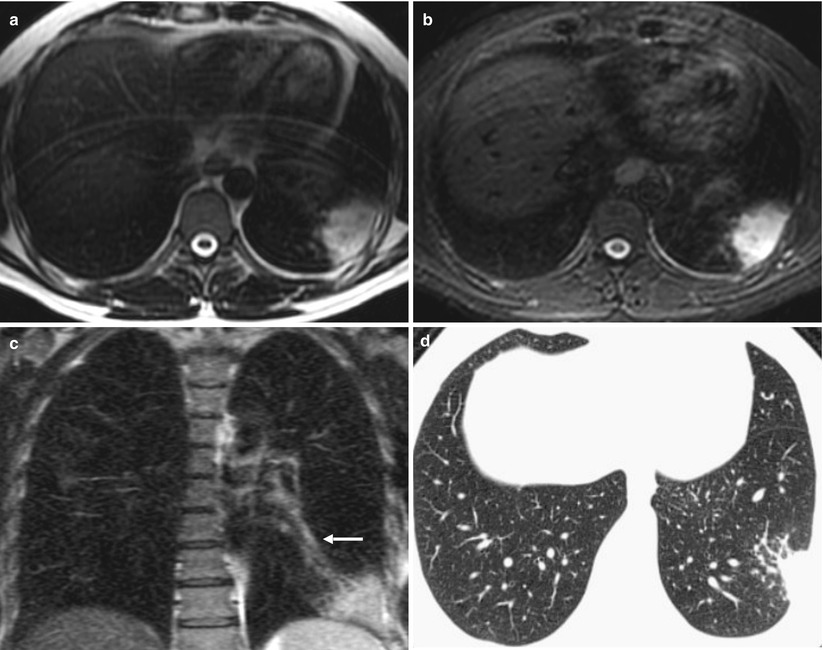
Fig. 16.2
Pneumonia. Chest MRI and follow-up CT performed in a patient with suspected pneumonia. Axial fast spin-echo T2-WI (a), axial fast spin-echo fat-suppressed T2-WI (b), coronal fast spin-echo T2-WI (c), and axial CT image (d). There is a wedge-shaped consolidation in the lower left lobe, with high signal intensity on T2-WI images (a–c), which suggests active inflammation. Note that there is a linear structure converging toward the consolidation (arrow, c), which also shows high signal intensity on T2-WI images, representing thickened wall bronchi with fluid content. A follow-up posttreatment chest CT (d) performed 2 weeks later shows that the consolidation has decreased in size
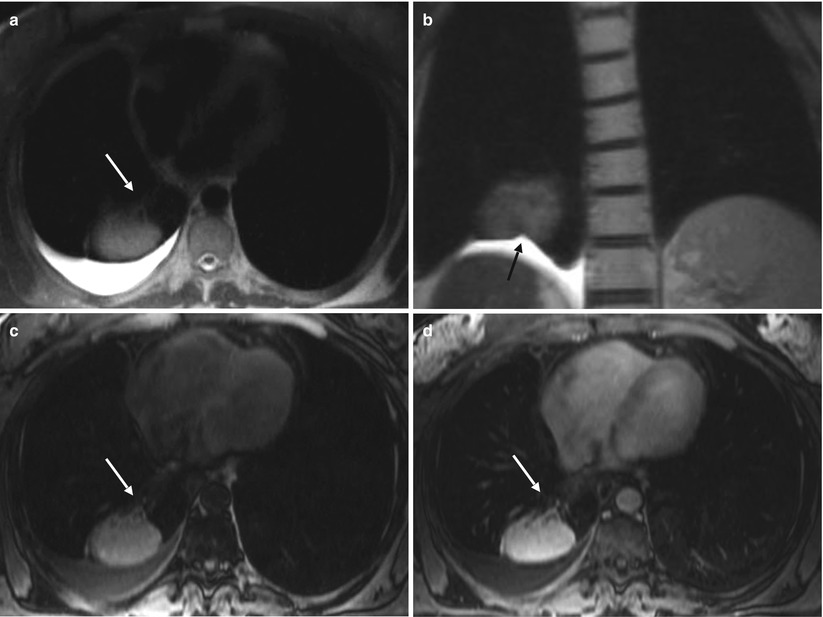
Fig. 16.3
Pulmonary consolidation (rounded atelectasis). Chest MRI performed to evaluate a lung mass detected on a follow-up x-ray of a patient with pleural effusion. Axial fast spin-echo fat-suppressed T2-WI (a), coronal fast spin-echo T2-WI (b), and axial pre- (c) and post-contrast (d) fat-suppressed 3D GRE T1-WI. Areas of signal intensity that obscures the margins of vessels and airway wall are depicted and are compatible with a consolidation. The typical morphology of a rounded atelectasis in association with pleural effusion is seen. Folding of the visceral pleura (black arrow, b) along with converging of vessels and bronchi into the atelectasis (white arrows, a, c, d) is well shown on MRI images
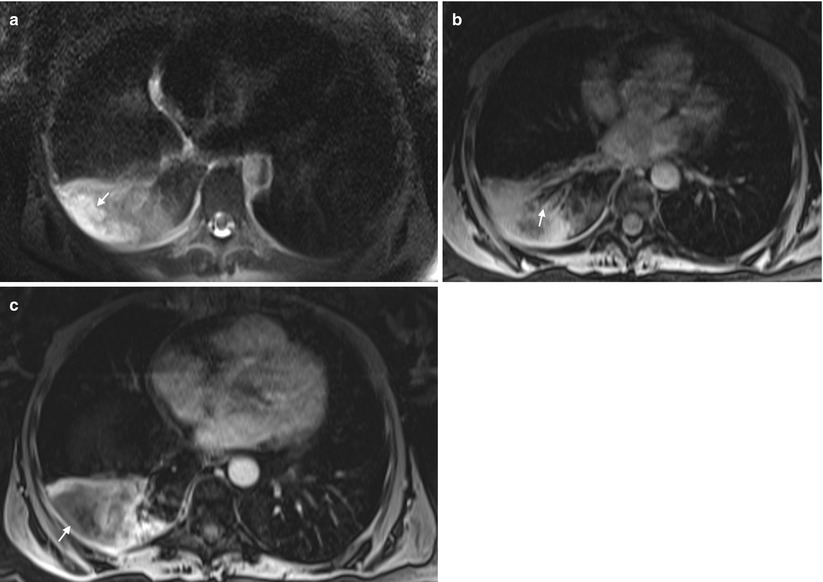
Fig. 16.4
Necrotizing pneumonia. Axial fat-suppressed fast spin-echo T2-WI (a) and axial post-contrast (b, c) fat-suppressed 3D GRE T1-WI. A pulmonary consolidation (arrow) is seen in the right lower lobe with high signal intensity on T2-WI (a) obscuring the bronchovascular margins. Air bronchogram is also depicted (arrow, b). A region of higher T2 signal intensity is seen inside the consolidation, with no enhancement, most consistent with an area of necrosis
The differential diagnoses of consolidation include various substances that may fill the air space, including fluid, blood, pus, and cells. CT attenuation is nonspecific; however, given the MRI ability to characterize different aspects of tissue on the basis of signal intensity, it may be useful for the evaluation of the consolidated parenchyma [17]. For example, focal consolidation in pulmonary infarction due to intra-alveolar blood, or pulmonary hemorrhage that might be related to several diseases such as Goodpasture’s syndrome or invasive aspergillosis, often exhibits high signal intensity on T1-WI due to methemoglobin formation in subacute hemorrhage.
Pleural effusions are a common finding in patients with pneumonia. More than 40 % of patients with bacterial pneumonia and 60 % of patients with pneumococcal pneumonia develop parapneumonic effusions.
Parapneumonic pleural effusions might appear as free-flowing pleural fluid producing sickle-shaped opacity (in most cases posteriorly) with high signal intensity on T2-WI and low signal intensity on T1-WI.
Loculated fluid collections might appear as lenticular opacities in a fixed position and usually develop when frank pus accumulates in the pleural space in the setting of empyema. Significant pleural enhancement is seen after contrast administration. MRI is useful for evaluating the thickening of the pleural membrane when the administration of contrast material is contraindicated, such as in pregnant patients.
16.3.1.2 Tuberculosis
In 2013, 3.3 million cases of tuberculosis were estimated to occur in women worldwide. During pregnancy, tuberculosis is associated with poor outcomes, including increased mortality in both the neonate and the pregnant woman [29].
It has been suggested that MRI might be useful for the diagnostic evaluation of the lung but also to replace CT in assessing lung tuberculosis in women during pregnancy.
Based on a correlation between MRI and CT, the findings in both techniques regarding consolidations, nodules, and cavities correlate well and show comparable results when identifying these characteristics. Consolidations may demonstrate high T2 signal intensity when it is associated with liquefactive necrosis and low signal intensity on T2-weighted and STIR sequences when it is associated with caseating necrosis, probably due to the presence of paramagnetic free radicals in macrophages, which produce T2 shortening or magnetic susceptibility effects on T2-weighted sequences [30].
MRI may depict nodules and micronodules in the pulmonary parenchyma greater than 5 mm in diameter [31]. Three-dimensional GRE and T2-weighted SS-FSE are the most widely used sequences for the detection of pulmonary nodules; however, the three anatomic distributions of the nodules (centrilobular, lymphatic, or random) are not well characterized by MRI. A cavitation is a gas-filled space, within a pulmonary consolidation, mass, or nodule [32]. MRI allows the evaluation of cavity wall thickness and air fluid levels and the identification of intracavitary filling defects [17]. Leutner et al. [33] described the ability of MRI to show various features of opportunistic pneumonia, including cavitation, which are well-known CT findings. MRI and CT have demonstrated a high level of agreement in the detection of lung cavities in tuberculosis. “Tree in bud” and ground-glass opacities are more difficult to detect on MRI [34].
Due to its excellent contrast resolution, MRI seems to be more accurate than unenhanced CT revealing lymph node involvement, pleural abnormalities, and parenchymal caseation.
16.3.1.3 Pulmonary Edema Related to Preeclampsia and Tocolytic Therapy
Preeclampsia is a multisystemic condition, affecting 2–5 % of pregnancies in the United States and with a worldwide prevalence ranging between 3 and 8 %. When severe, various serious complications can increase the mortality in pregnant women. One of them although rare is pulmonary edema, which has an associated mortality rate close to 10 % [35, 36].
Beta (β)-adrenergic agents such as ritodrine and terbutaline are commonly used to inhibit preterm labor and, in this setting, can also cause acute respiratory failure due to pulmonary edema. The etiology of this complication is unclear [22].
There are no specific studies regarding MR evaluation of pulmonary edema; however, the classic CT findings of pulmonary edema, such as septal thickening and areas of consolidation (later stages), may also be seen on MRI. Septal thickening is smooth in contour and appears as interlobular interstitium linear pattern with high signal on T2-WI. Consolidation will appear as described for pneumonias above.
16.3.2 Chronic Diseases
16.3.2.1 Asthma
Asthma affects between 3 and 12 % of pregnant women worldwide, and the prevalence among pregnant women is rising. For unknown reasons, asthma severity appears to be greater in women between the ages of 20–50 years, carrying poorer prognosis than in men [22, 37].
The effect of pregnancy in asthma is incompletely understood and is a matter of debate. However, exacerbations occur in approximately 20 % of all asthmatic pregnant women and are greatly increased in women with severe asthma [37]. Moreover, the effect of pregnancy on asthma symptoms is likely to be consistent during successive pregnancies in an individual patient [22]. Asthma exacerbations require appropriate treatment in order to protect the fetus as far as possible from adverse outcomes. In particular, the fetus is at risk of being born of low birth weight, which may predispose to diseases in later life [37].
Currently, pulmonary function tests (PFT) are considered the most important assessment method and are the most widely used method for diagnosis and management of asthmatics.
Smooth muscle hyperresponsiveness and hypertrophy, increased mucous production, and subepithelial fibrosis are the frequent abnormalities present in asthma. Many of these findings are not evident on standard MRI sequences. New investigational techniques using positive contrast inhaled hyperpolarized noble gases imaging, such as 3He and 129Xe or O2-enhanced MRI (OE-MRI), have shown to be promising in the evaluation of patients with asthma [25, 38]. This technique can assess regional changes caused by airflow obstruction. In a patient with obstruction of medium and small airways caused by asthma, the airspaces distal to the obstruction do not fill with the positive contrast inhaled gas. Therefore, the lungs of healthy patients demonstrate a uniform high signal, whereas the lungs of patients with asthma show wedge-shaped regions of low signal intensity on T1-WI [25]. In patients with asthma, these defects have been shown to increase with provocation by exercise or administration of a bronchoconstrictor (methacholine) and decrease with albuterol. OE-MRI is a nonionizing source of contrast that may have a role in the assessment asthma during pregnancy [25], although further work is required to validate and to extend these findings for pregnant patients.
16.3.2.2 Cystic Fibrosis
Cystic fibrosis is an autosomal recessive disorder that is characterized by exocrine gland dysfunction, with the lungs and pancreas being primarily affected. The pulmonary disease consists of chronic, recurrent infections, bronchiectasis, and airway obstruction. With improved treatment, patients are surviving well into their childbearing years. The advisability of pregnancy should be based on disease stability. As a rule, patients with a significant decline in pulmonary function over a short time period and those with frequent infectious exacerbations are best advised against pregnancy [22].
Chest imaging is essential in the assessment of respiratory disease in cystic fibrosis [39]. Being a chronic disease and affecting young patients, the exposure to ionizing radiation is an important concern. This is especially valid for pregnant women.
MRI and CT are comparable for the depiction of larger morphological changes in cystic fibrosis lung disease such as bronchiectasis, bronchial wall thickening, mucus plugging, and air fluid levels, as well as segment consolidation and architectural destruction (Fig. 16.5). Mucus plugging is well visualized by MRI, even in small airways, due to the high signal intensity of fluid content on T2-WI. This modality has been used successfully to score and follow patients with cystic fibrosis [17, 21, 39, 40].
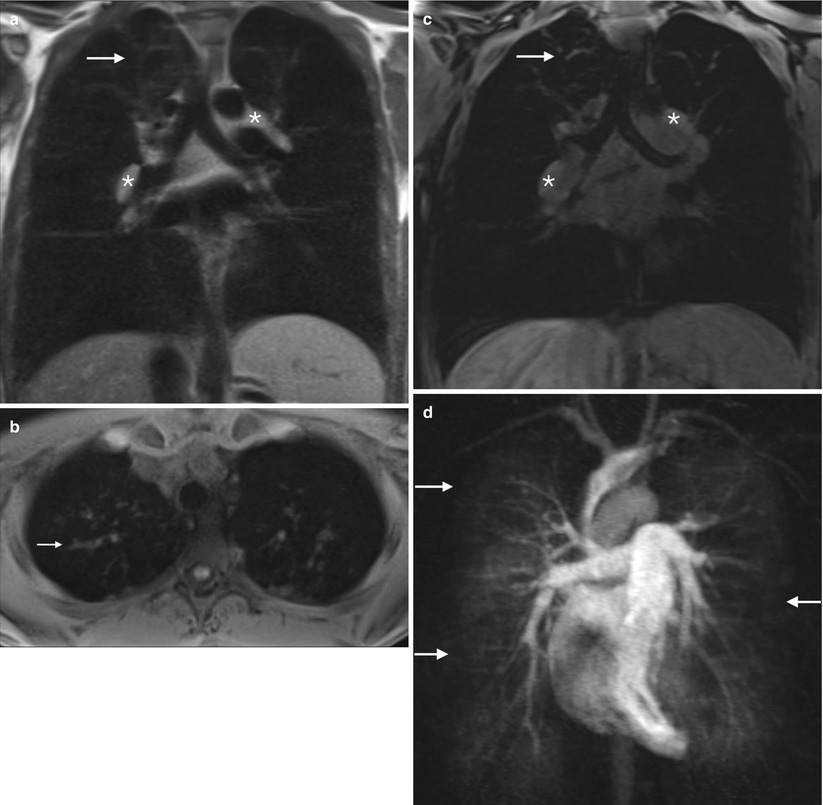
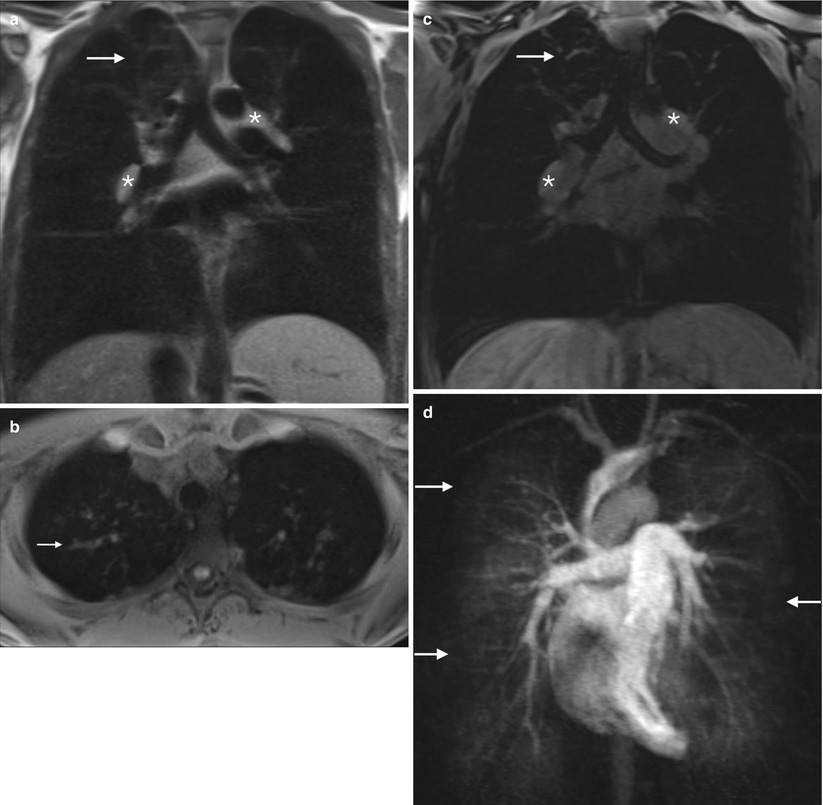
Fig. 16.5
Cystic fibrosis. Chest MRI of a 20-year-old female with cystic fibrosis, admitted with symptoms of pulmonary exacerbation. Coronal spin-echo T1-WI (a), axial (b) and coronal (c) unenhanced 3D GRE T1-WI, and MIP (maximum intension projection) reconstructions of enhanced time-resolved MRA perfusion study image (d). Apical bronchiectasis and mucus plug (arrows, a–c) are depicted. Note the hilar prominent lymphadenopathies (asterisks, a, c). The perfusion study shows areas of decreased perfusion (arrows in d), corresponding to the hypoventilated areas of small airway mucus plugging (arrows, c)
16.3.2.3 Sarcoidosis
Sarcoidosis is a disease of unknown etiology characterized by granulomatous inflammation of body tissues, most commonly the lungs, liver, lymph nodes, eyes, and skin. Patients are often asymptomatic, and the disease would be discovered incidentally on a chest radiograph performed for unrelated reasons [22].
Sarcoidosis in pregnancy is a rare disease associated with an increased risk of adverse obstetrical outcomes. Women with sarcoidosis can carry out successful pregnancies; however, should be made aware of the higher risk of adverse events.
CT is the gold standard imaging method of the lung parenchyma in pulmonary sarcoidosis. However, MRI may be a viable alternative to CT as MRI has been shown to correlate well with CT in this setting [19].
Patterns of sarcoidosis can be described in MRI as parenchymal opacification including ground-glass opacity, consolidation, parenchymal band or scarring (defined as thin linear or discoid regions of signal abnormality), nodules, atelectasis, and focal areas of nodular architectural distortion [19] (Fig. 16.6).
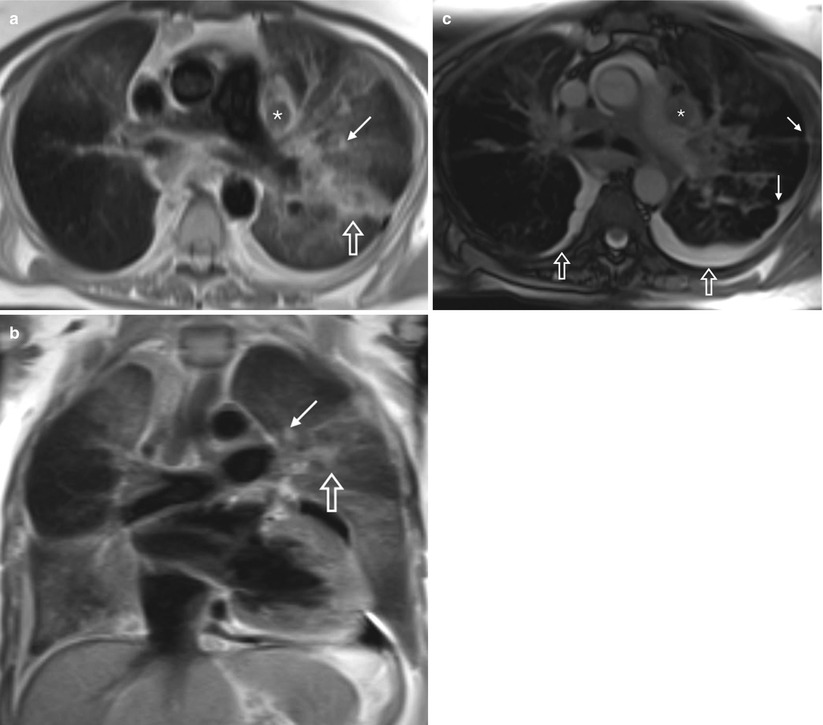
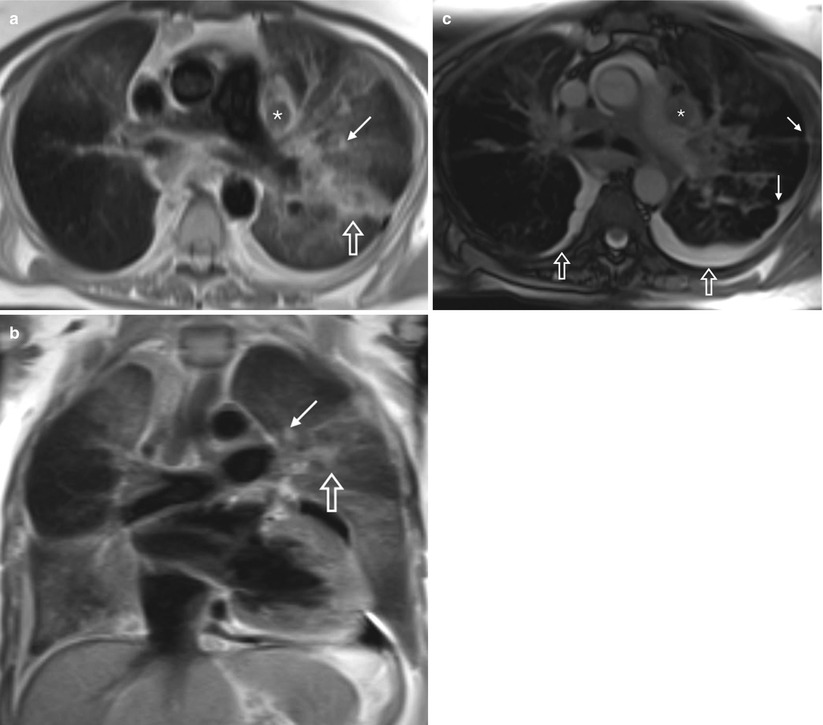
Fig. 16.6
Sarcoidosis. Chest MRI performed in a female patient to follow up for sarcoidosis. Axial (a) and coronal (b) fast spin-echo T2-WI and axial bSSFP (c) images. Areas of ground-glass opacities, more severe at the left side where it tends to consolidate (opened arrows, a, b) and some nodules (arrows, a–c) are depicted, showing the pulmonary sarcoidosis. Lymphadenopathies are well illustrated on both axial images (asterisks, a, c). Pleural retraction (arrows, c) and effusion (opened arrows, c) are also noted
Chung et al. [19] found that in regard to subset scoring, MRI and CT scores seemed to have the strongest correlation for parenchymal opacification and reticulation rather in the setting of lung nodules, where CT performed better. However, they did not include MRI short tau inversion recovery (STIR) images which have been reported to be the most sensitive sequence in the detection of subcentimeter pulmonary nodules [41, 42].
16.3.3 Other Parenchymal Lung Diseases
Other less frequent parenchymal lung diseases may also affect childbearing women, such as lymphangioleiomyomatosis or interstitial lung diseases (Fig. 16.7).
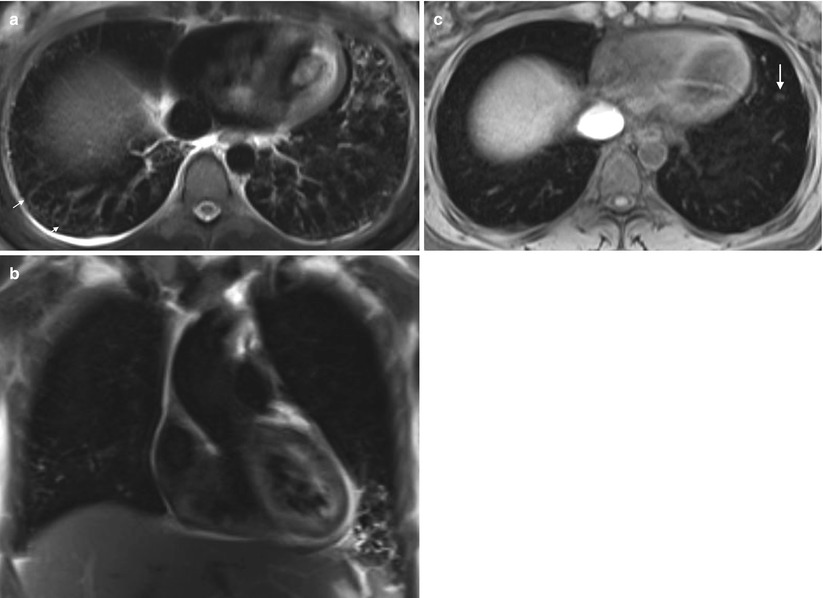
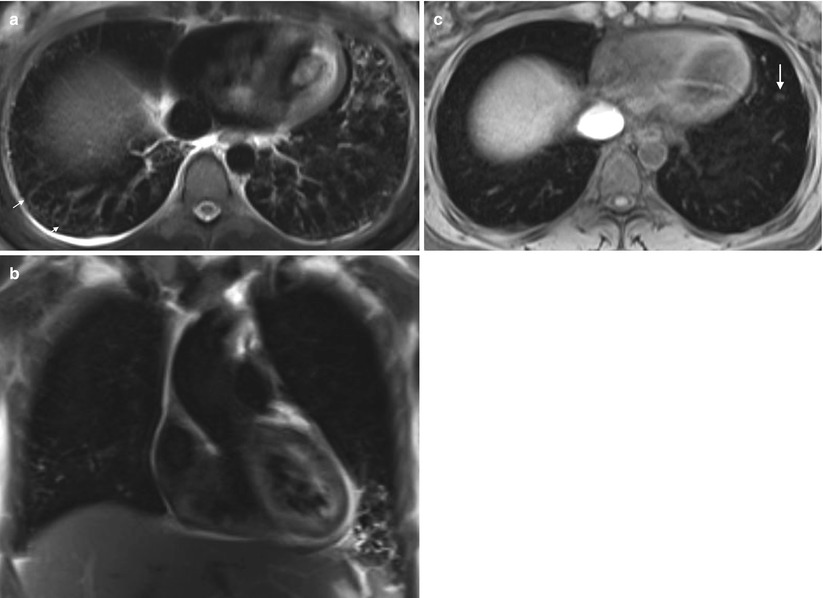
Fig. 16.7
Interstitial pneumonia. Chest MRI performed on a 32-year-old pregnant woman with respiratory symptoms after abnormal findings of the chest x-ray. Axial fast spin-echo fat-suppressed T2-WI (a), coronal fast spin-echo T2-WI (b), and non-enhanced axial fat-suppressed 3D GRE T1-WI (c). A mild-to-moderate interlobular septal thickening is depicted (arrows), with high signal intensity on T2-WI. The septal thickening is less evident on T1-WI. Note the small centrilobular nodules (short arrows, c). Note the minimal right-sided pleural effusion
The relatively limited number of MRI studies that have been clinically performed in these patients is due to the novelty of MRI in this field. Nonetheless, published data suggest at least three possible applications for lung MRI in these settings: (1) visualization and recognition of morphological changes and their patterns, (2) assessment of the inflammatory activity of the disease, and (3) effects of lung morphologic changes on functional parameters such as contrast enhancement and perfusion [24].
16.3.4 Solitary Pulmonary Nodules
Occasionally, a chest x-ray in a pregnant woman, who may not have a previous x-rays for comparison, will show a small lung nodule. The likelihood of malignancy is low for patients under 35 years of age (approximately 5 %), even in cigarette smokers. Additionally, there is little evidence that delaying treatment for some months will result in a reduction of cure rate [43]. Instead, facing these situations may modify attitudes relative to pregnancy.
It has been shown that MRI is useful for detecting and characterizing lung nodules (Fig. 16.8). In fact, MRI has been widely accepted as an ideal screening modality for its nonionizing radiation characteristics [44]. The sensitivity of MRI for nodules greater than 5 mm in diameter is approximately 95 % [45] (Fig. 16.9). The most reliable sequences for detecting lung nodules are STIR, T2-weighted FSE or SS-FSE, and T1-weighted 3D GRE sequences [41, 42, 46].
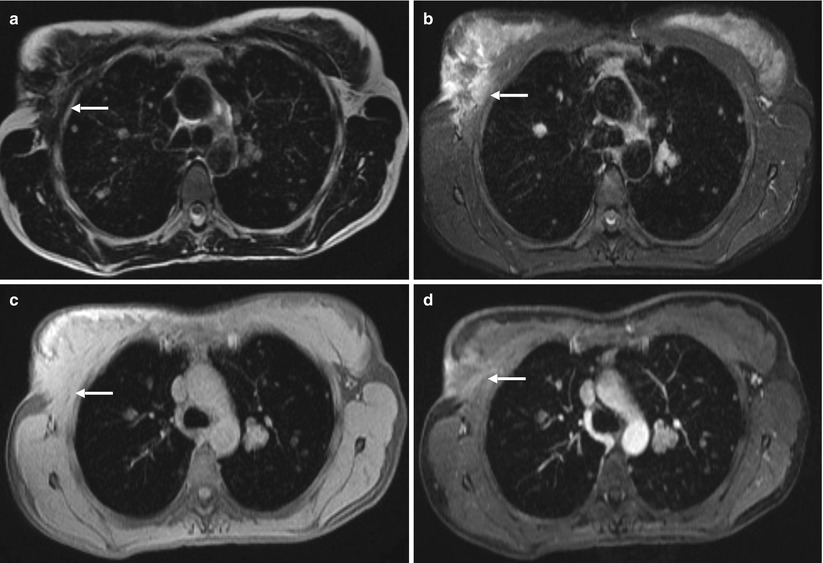
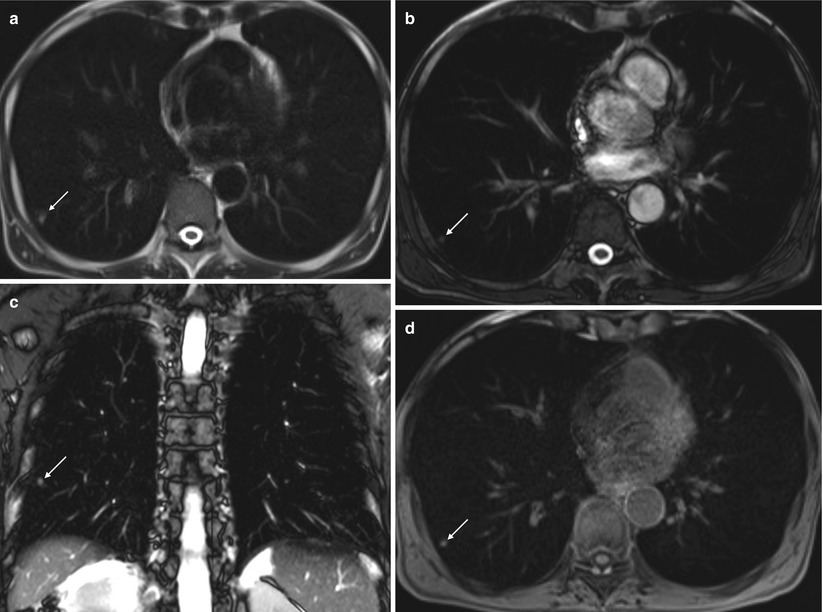
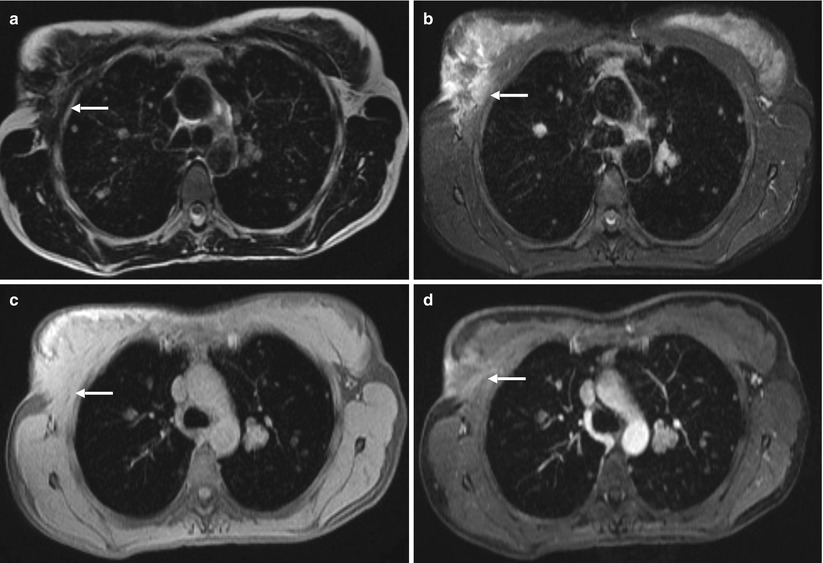
Fig. 16.8
Breast neoplasm with lung metastases. Chest MRI performed for breast neoplasm staging. Axial fast spin-echo T2-WI (a), axial fast spin-echo fat-suppressed T2-WI (b), and axial pre- (c) and post-contrast (d) fat-suppressed 3D GRE T1-WI. There is an ill-defined speculated mass in the lateral right breast (arrows, a–d) extending from the skin to the underlying pectoralis muscle, better shown on T2-weighted fat-suppressed (b) and T1-weighted post-contrast (d) images. Multiple round-shaped nodules are diffusely spread throughout the lungs, consistent with metastases. These findings show the capability of MRI to detect small nodules
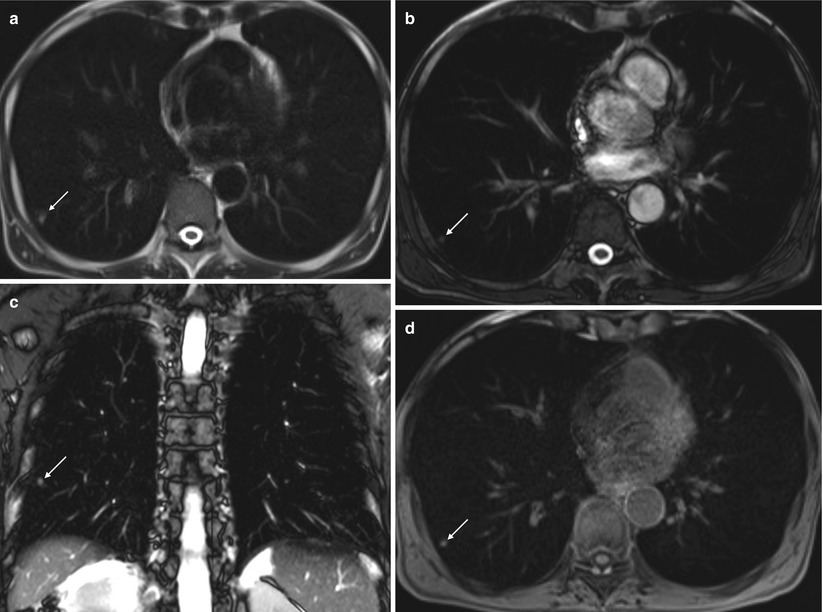
Fig. 16.9
Small metastasis from renal cell carcinoma. Unenhanced chest MRI performed in a patient with history of renal cell carcinoma. Axial fast spin-echo T2-WI (a), axial (b) and coronal bSSFP image (c), and axial fat-suppressed 3D GRE T1-WI (d). A small (5 mm) parenchymal nodule is depicted on all sequences (arrows, a–d), showing the ability of MRI to detect small lung nodules
Many pulmonary nodules, including those of lung cancers, pulmonary metastases, and low-grade malignancies such as carcinoids and lymphomas, appear of low to intermediate signal intensity on T1-WI and of slightly high signal intensity on T2-WI.
DWI allows for differentiation of malignant from benign solitary pulmonary nodules with sensitivity and specificity of 70.0–88.9 % and 61.1–97.0 %, respectively [47–49]. In comparison, the specificity seems to be comparable with that of FDG-PET/CT [47]. Therefore, non-enhanced MR techniques can help in differentiating differentiate malignant from benign SPNs and can be considered as effective as FDG-PET or PET/CT.
Some lung nodules may display specific features, such as pulmonary hamartomas. Pulmonary hamartomas are the third most frequent cause of solitary pulmonary nodule. The presence of fat is the key feature for the diagnosis of this benign lesion. Fat is well depicted on fat suppression and in-phase and out-of-phase imaging (Fig. 16.10).
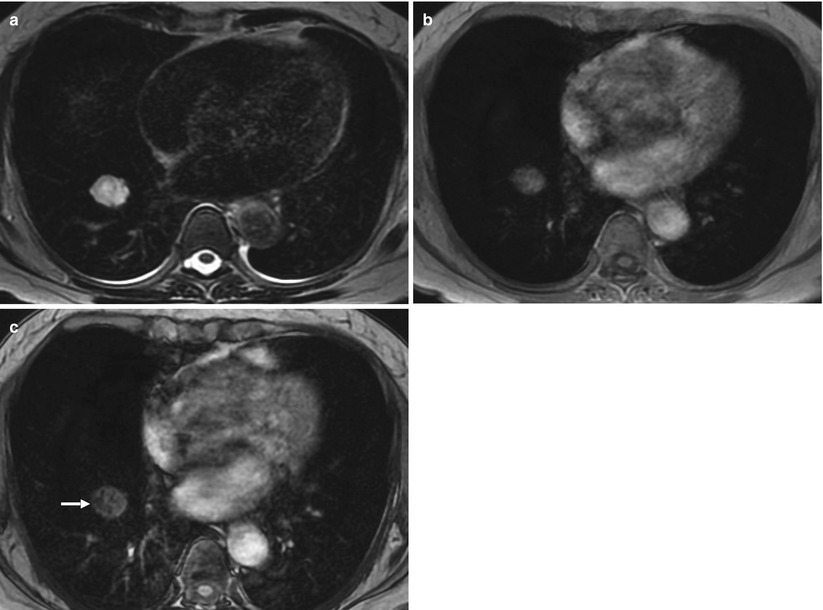
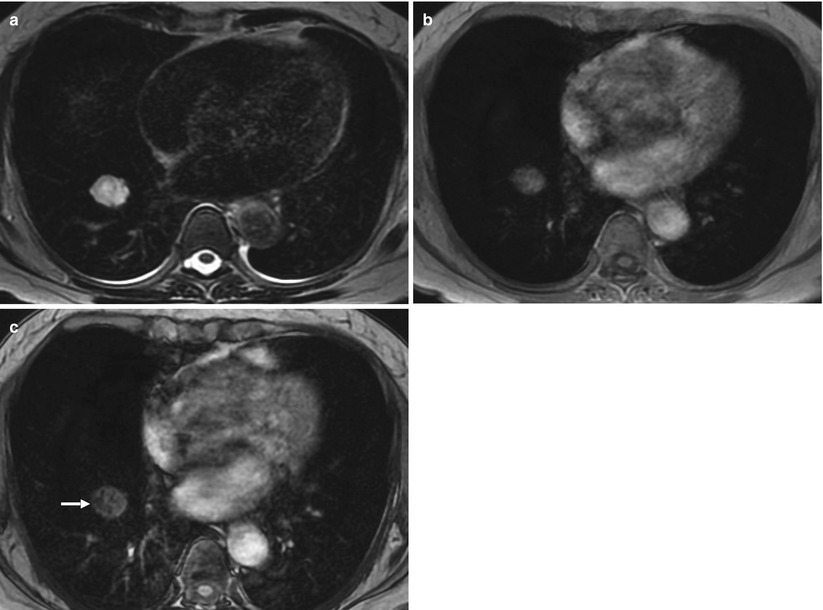
Fig. 16.10
Hamartoma. MRI performed in a patient for evaluation of a right lung nodule depicted as an incidental finding on x-ray. Axial fast spin-echo T2-WI (a) and T1-WI in-phase (b) and out-of-phase (c) images. The nodule shows heterogeneous high signal intensity on T2-WI (a) and T1-WI in-phase (b) images. Areas of signal loss on T1-WI out-of-phase images (arrows, c) are evident within the nodule, consistent with fatty component
16.3.5 Primary Lung Cancer
Cancer in general during pregnancy is rare and occurs in 1 to every 1000 gestations. The most common types of cancer diagnosed during pregnancy are breast and cervical cancer, lymphoma, melanoma, and leukemia [50].
Primary lung cancer in patients during pregnancy is an extremely rare coincidence.
Lung cancer staging is feasible using MRI. For this purpose, MRI can provide a comprehensive morphologic TNM evaluation. The extent of mediastinal, hilar, and supraclavicular lymph node enlargement can be assessed with excellent soft tissue contrast [24]. Unenhanced MRI is comparable to CT in differentiating between T1–T2 and T3–T4 tumors. MRI seems to be better in evaluating pericardial (T3) and heart (T4) involvement. Contrast-enhanced magnetic resonance angiography (CE-MRA) is also a good imaging method for the evaluation of hilar invasion, with some studies showing higher sensitivity and specificity than CT [51]. MRI might also be superior in the characterization of central masses causing atelectasis [52] (Fig. 16.11).
Fig. 16.11
Central lung cancer. The chest unenhanced MRI performed in a patient to clarify a central left-sided mass. Axial fat-suppressed fast spin-echo T2-WI (a) and axial (b, e, and g) and coronal (c, d, f, and h) and pre- (b–d) and post-contrast (e–h) fat-suppressed 3D GRE T1-WI. A central left-sided primary lung neoplasm is depicted (asterisks, a–c, e, f), with hilar infiltration and left upper lobar atelectasis. On unenhanced T1-WI, note the hilar infiltration (c) and the lower signal of the tumor when compared to the atelectasis (black arrow in c and f), showing the value of unenhanced chest MRI on central lung neoplasms assessment. These findings can be confirmed on enhanced sequences (f). The left-sided mediastinal shift as the rising of the left hemidiaphragm due to left lung volume loss can be also seen. It is also depicted as bilateral pleural effusion (arrows, a) and bilateral lung metastases (opened arrows, d, g, and h), showing that MRI can contribute on lung cancer staging on selected patients
A recently published work by Liu et al. [53] suggested that the DWI-driven ADC measurement of lung cancer is a helpful method to evaluate the pathological grade and tumor cellular density. Therefore, the quantitative analysis of ADC in conjunction with conventional MRI findings could provide more valuable information for the assessment of pulmonary tumor.
MRI assessment of lymph nodes is possible not only referring to morphologic features as CT but also functional evaluation with DWI. Unenhanced STIR sequences combined with DWI can be an accurate noninvasive method of staging lymph nodes [51, 52, 54].
Percutaneous transthoracic needle biopsy has been proven as a minimally invasive, sensitive mean to the tissue diagnosis of lung lesions. Recently, Liu et al. demonstrated that MRI-guided percutaneous transthoracic needle biopsy is safe, feasible, and a highly accurate diagnostic technique for the pathologic diagnosis of pulmonary nodules.
16.4 Mediastinum
Mediastinal tumors in pregnancy can be found incidentally during chest workup for unrelated reasons or, less frequently, found as a result of a symptomatic clinical manifestation. In adults, most mediastinal tumors are primary thymic neoplasms, thyroid masses, or lymphomas [55].
While conventional radiology can assess mediastinal disease, cross-imaging methods made its diagnosis more accurate. Usually, the first-line imaging method is chest CT, ideally with IV iodinated contrast. Besides being a radiation-free method, MRI has a higher soft tissue contrast resolution and is able to characterize most mediastinal masses without the use of GBCAs. To achieve that MRI uses not only the multiparametric morphologic evaluation (T1- and T2-weighted sequences, with and without fat suppression plus or minus GBCAs), but also functional evaluation using DWI.
Recently, Seki et al. [56] showed that DWI alone is equal to CT for differentiating tumors not needing further intervention or treatment from those needing further intervention and treatment. Other studies showed that using unenhanced MRI can be better than CT, particularly in cystic diseases [57, 58]. Therefore, MRI is a good alternative to CT as a first-line modality in evaluating mediastinal masses, especially on pregnant women.
For the sake of simplicity and in order to attempt better differential diagnosis, the authors will follow classic anatomic division of mediastinum (i.e., anterior, middle, and posterior compartments) in this chapter [59].
16.4.1 Anterior Mediastinum
The anterior mediastinum is bounded superiorly by the thoracic inlet; inferiorly by the diaphragm; posteriorly by the pericardium, aorta, and brachiocephalic vessels; and anteriorly by the sternum. Disease of any of the contents of the anterior mediastinum may result in a mass; thus, knowledge of the normal contents of the anterior mediastinum aids in developing a differential diagnosis once a mass has been identified.
The thyroid gland (if it extends into the mediastinum) is traditionally considered an anterior mediastinal compartment structure. The other contents include the adipose tissue, internal mammary vessels, nerves, lymph nodes, and thymus gland [59, 60].
Masses of the anterior compartment account for 50 % of all mediastinal masses [61]. Although more than two thirds of mediastinum tumors are benign, most of anterior compartment masses are malignant [62]. The authors will address the most frequent masses of anterior mediastinum in adults, namely, thymus masses, thoracic goiter, teratoma, and lymphoma.
16.4.1.1 Thymus
Thymus topography makes its imaging using MRI challenging. The recent developments in the MRI field have tackled the constant pulsation of the great vessels, beating of the heart, and movement of the lungs as image degrading factors.
In adulthood, the thymus is atrophic and mainly replaced by fat, being hyperintense in T1- and T2-weighted sequences. When the tissue has almost completely involuted, reticulonodular strands of thymic tissue and occasionally small rounded islands of residual thymus (measuring 7 mm or less) can remain and are considered normal [63].
Hyperplastic thymus can be difficult to distinguish from normal thymus. Some guidelines for making this differentiation are available and include the absence of rounded soft tissue masses >7 mm, absence of a convex contour of the thymus after 19 years of age, absence of soft tissue lobulation, absence of excessive thymic thickness (normal is ≤1.3 cm after 20 years of age), no history of diseases associated with thymic enlargement or hyperplasia, and absence of interval enlargement of thymic tissue during adulthood.
In a prospective study by Inaoka et al. [64], normal or hyperplastic thymus could be differentiated using a non-enhanced on chemical shift imaging (in-phase and out-of-phase T1-weighted sequences) due to the interspersed microscopic fat within the nonneoplastic thymic tissue (Fig. 16.12). These results are particularly interesting in the subset of pregnant patients, since neither ionizing radiation nor IV contrast is applied.
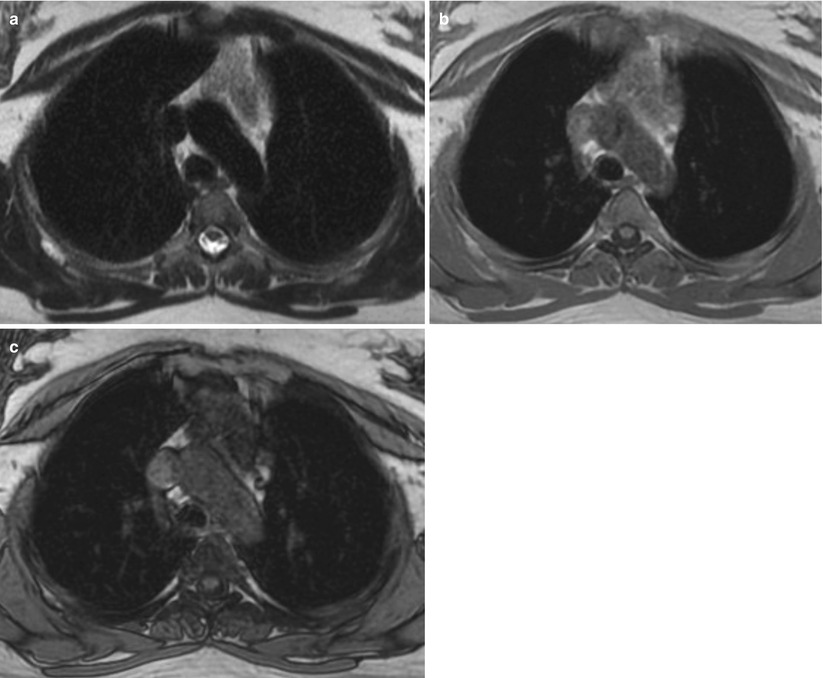
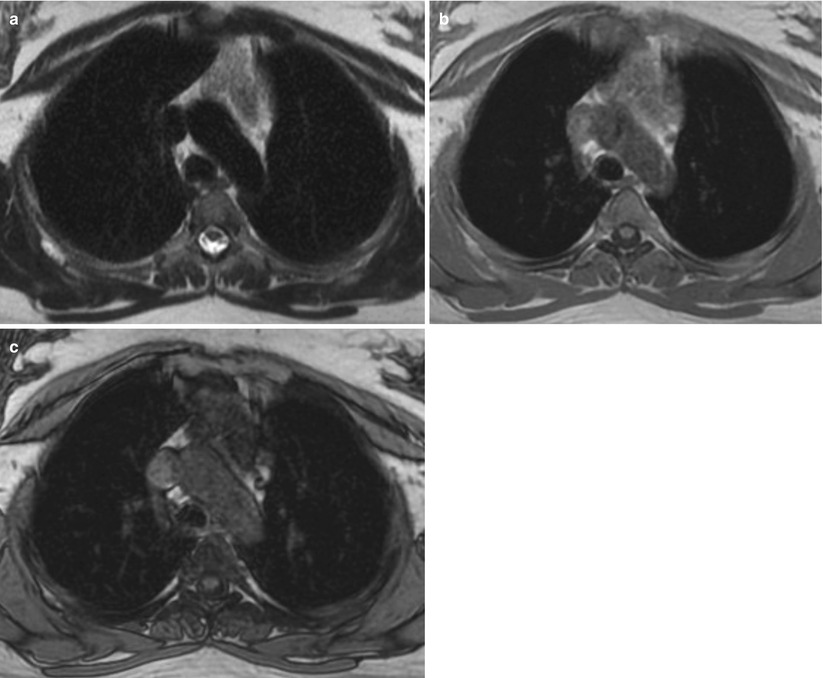
Fig. 16.12
Thymus hyperplasia. Chest MRI performed to evaluate an anterior mediastinal mass in a woman undergoing chemotherapy for breast cancer. Axial fast spin-echo T2-WI (a) and axial GRE in-phase (b) and out-of-phase (c) T1-WI. The mass shows intermediate signal intensity on T2-WI (a) and in-phase T1-WI (b), demonstrating homogeneous signal suppression on out-of-phase T1-WI (c). These features are consistent with hyperplasia due to the presence of microscopic fat within the thymic tissue, virtually excluding thymic tumor
Unenhanced MRI differentiates thymic cysts from solid lesions more readily and consistently than CT. Hyperdense thymic cysts are often misinterpreted as solid lesions on CT [63]. T1 signal of thymic cysts can vary depending on their contents (hemorrhage, lipid, and protein increase in internal T1 intensity), but generally, they are hypointense on T1-WI. Virtually, all thymic cysts are hyperintense on T2-WI, albeit not always as hyperintense as spinal CSF [63] (Fig. 16.13). Congenital cysts tend to be unilocular and have thin walls, whereas acquired cysts are multiloculated and thick walled. The latter usually are inflammatory in nature. When evaluating a thymic cystic lesion, one should be aware that cystic regions might occur in thymic neoplasms such as thymoma and lymphoma.
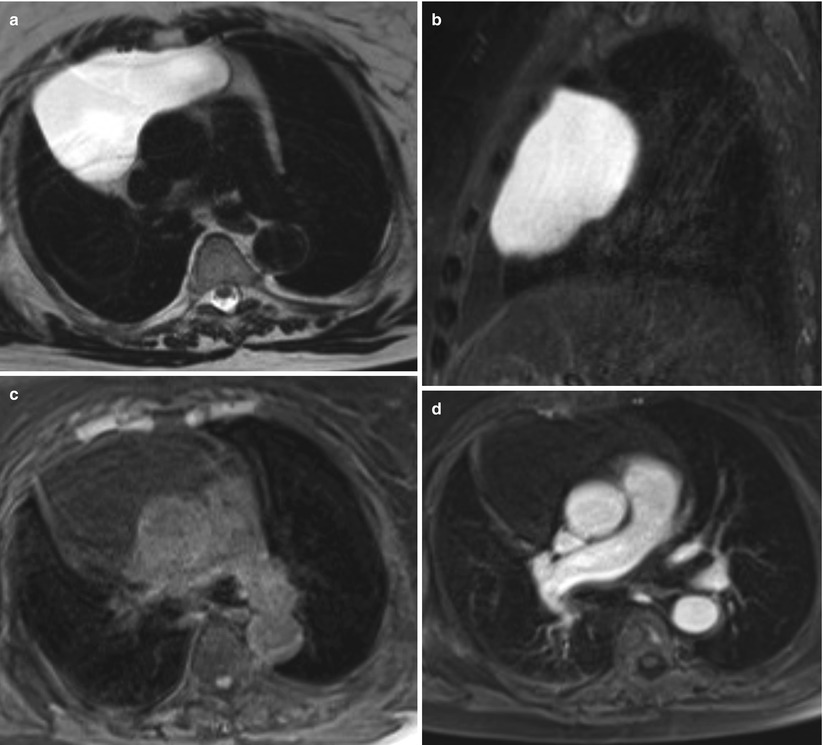
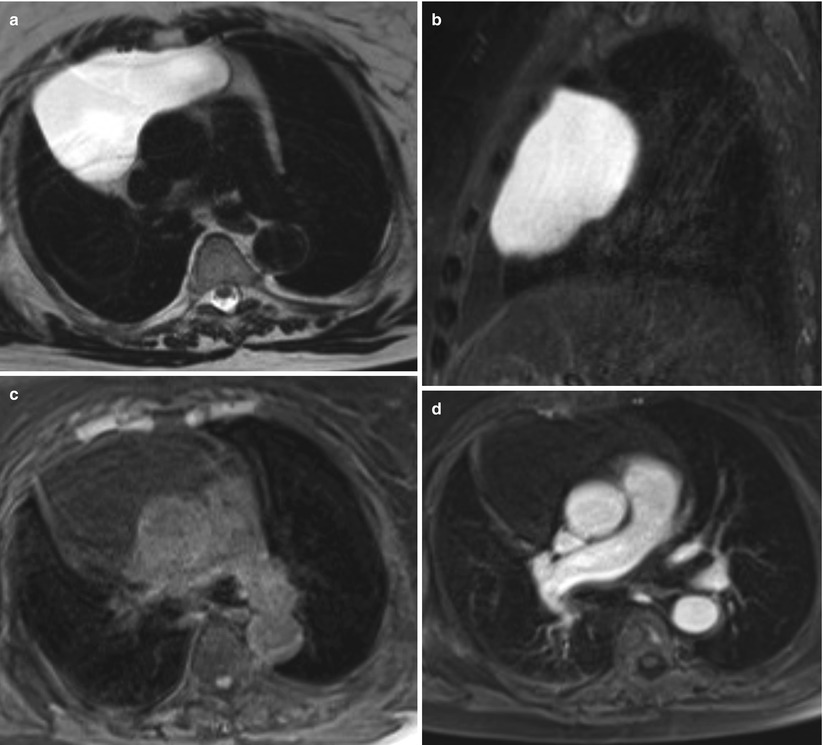
Fig. 16.13
Thymic cyst. Chest MRI performed to evaluate mediastinum enlargement depicted as an incidental finding on an x-ray. Axial fast spin-echo T2-WI (a), sagittal fast spin-echo fat-suppressed T2-WI (b), and axial pre- (c) and post-contrast (d) fat-suppressed 3D GRE T1-WI. There is a large lesion located in the anterior mediastinum, showing high signal intensity on T2-WI (a, b), low signal intensity on T1-WI (c), and absence of enhancement on post-contrast sequence (d), consistent with a cystic lesion, most probably originating from the thymus
Thymomas are histologically classified as less aggressive (types A, AB, and B1 5-year survival rates >94 %) and more aggressive and of poor prognosis types (B2, B3, and thymic carcinoma) [65].
In pregnant women, the possibility of separating these different subtypes with non-enhanced MRI (morphology and functional imaging) is desirable. Based on the clinical settings, lesions with better prognostic outcome could wait till delivery for a treatment decision (e.g., surgery).
Thymoma shows low to intermediate signal intensity on T1-WI and high signal intensity on T2-WI (Fig. 16.14). Signal intensity is heterogeneous in tumors with necrosis, hemorrhage, or cystic change.
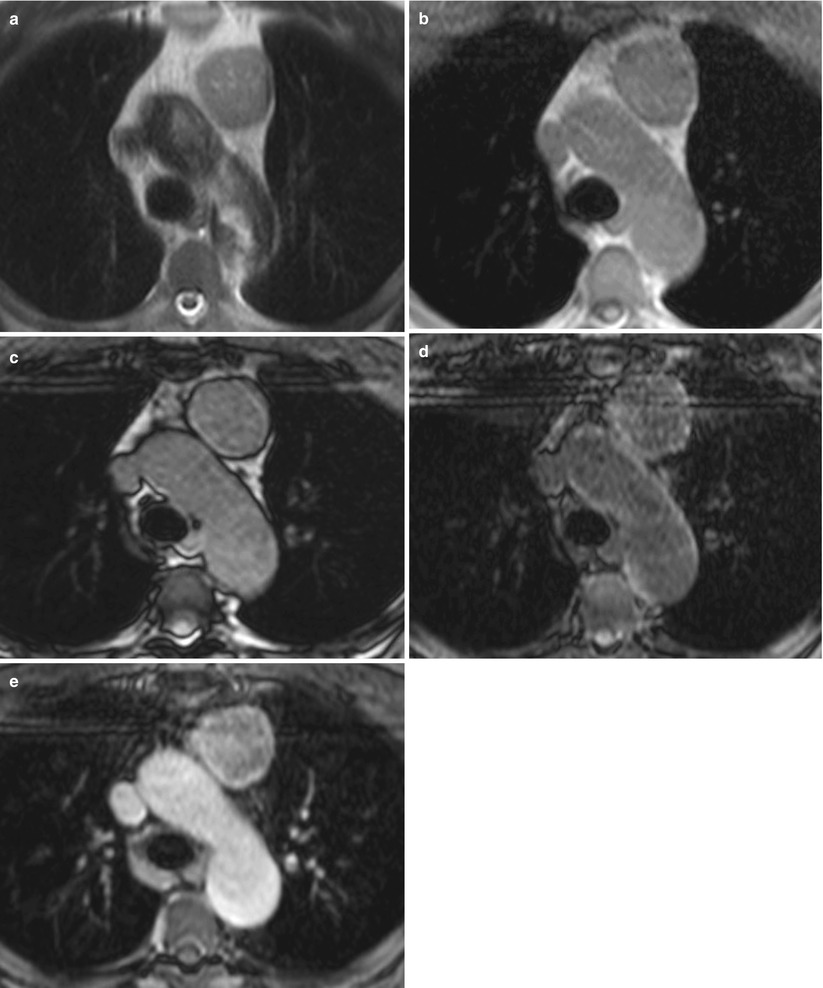
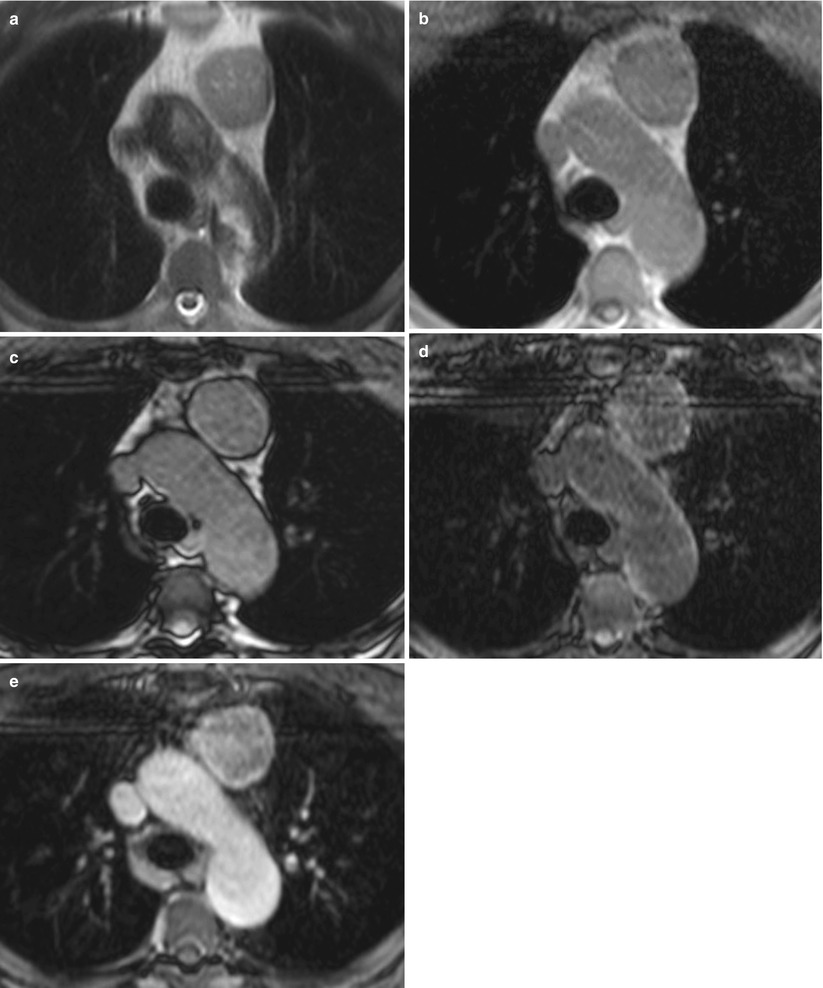
Fig. 16.14
Thymoma. Chest MRI performed in a patient with signs and symptoms of myasthenia gravis. Axial fast spin-echo T2-WI (a), axial in-phase (b) and out-of-phase (c) GRE T1-WI, and axial pre- (d) and post-contrast (e) fat-suppressed 3D GRE T1-WI. The mass has mild high signal intensity on T2-WI (a) and intermediate signal on T1-WI (b–d), showing homogeneous enhancement on post-contrast images (e). Note that there is no signal suppression on the out-of-phase T1-WI (c) comparing to the in-phase T1-WI (b), which is compatible of neoplastic tissue instead of hyperplasia
It has been suggested that morphologic MR sequences can differentiate some thymoma subtypes. Round, smoothly marginated encapsulated tumors are typically type A thymomas; and the presence foci within the mass with low signal on T2-weighted sequences (whether due to hemorrhage, flow voids, or calcification) in conjunction with mediastinal lymphadenopathy favors thymic carcinoma [63]. Recently, Seki et al. [56] showed that DWI alone is equal to CT for differentiating tumors not needing further intervention or treatment from those needing further intervention and treatment. Furthermore, comparisons of DWI-driven ADCs for groups A and B and between thymic malignancies and thymomas in group B showed significant differences.
Often discovered incidentally, thymolipoma is a rare benign encapsulated tumor that is usually found in young adults and has no sex predilection. Histologically, it is composed of mature adipose and thymic tissue in variable proportion. In pregnant women, unenhanced MRI is preferred, since it accurately shows a well-defined encapsulated mass that has extensive fat content (high signal intensity on both T1- and T2-weighted sequences and shows obvious drop of signal intensity on fat-suppressed imaging) [55, 60].
16.4.1.2 Thyroid
Intrathoracic, retrosternal goiter accounts for 3–6 % of mediastinal masses, with a majority located in the anterior compartment. The most common type is secondary to goiter with direct downward extension from the neck [60] (Fig. 16.15). An intrathoracic thyroid mass developing from heterotopic thyroid tissue without any connection to the thyroid in the neck is extremely rare [55].
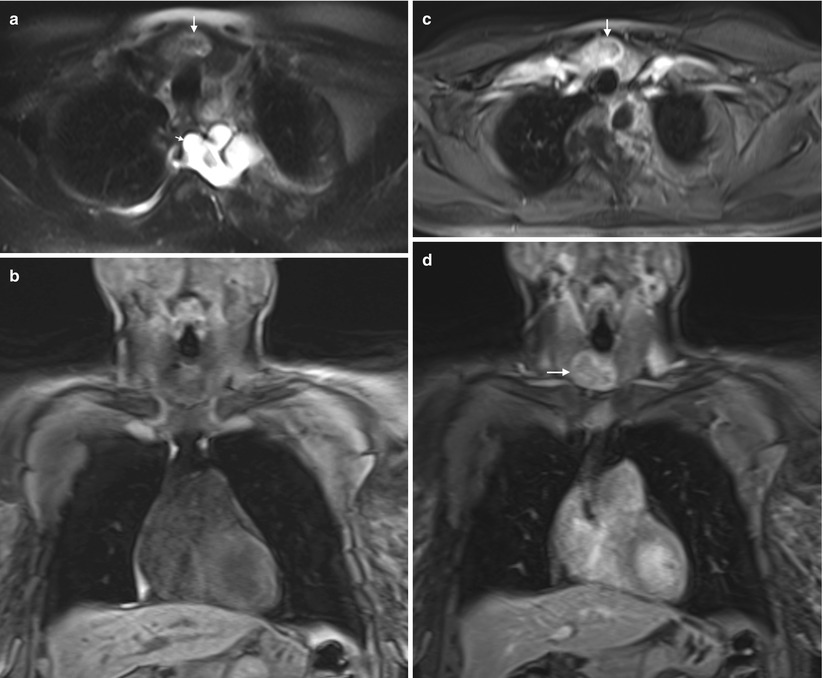
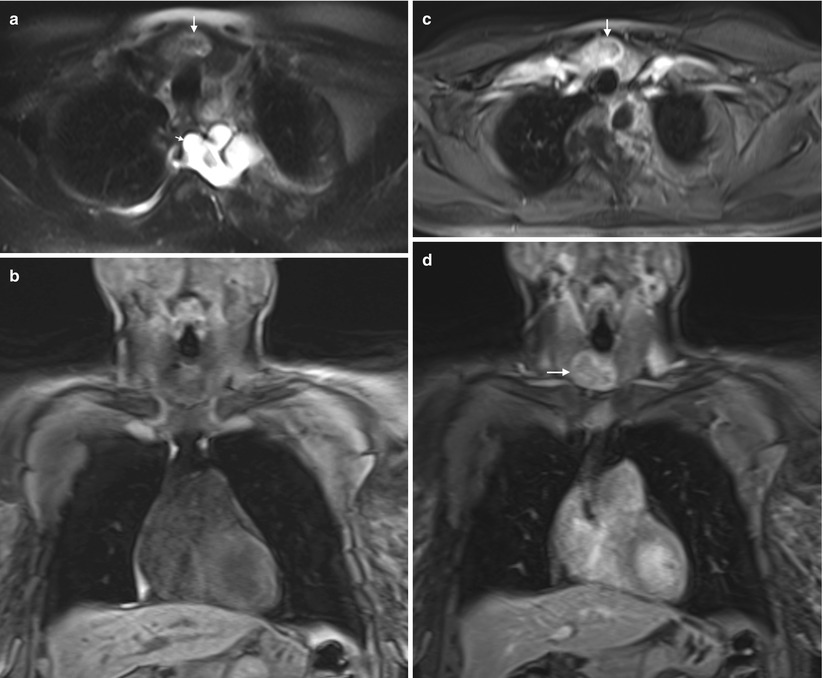
Fig. 16.15
Goiter. Chest MRI performed to evaluate an incidental finding of an anterior mediastinal mass on an x-ray. Axial fast spin-echo fat-suppressed T2-WI (a), coronal pre-contrast fat- suppressed 3D GRE T1-WI (b), axial post-contrast fat-suppressed 3D GRE T1-WI (c), and coronal post-contrast fat-suppressed 3D GRE T1-WI (d). An enlarged thyroid gland reaching the thoracic outlet, with mild high signal intensity on T2-WI (a) and intermediate signal on T1-WI (b). A moderately high signal intensity on T2-WI thyroid nodule is depicted (arrow, a), with strong enhancement after contrast (arrow, c, d). Multiple well-circumscribed lesions abutting the neural foramina at the upper thoracic spine are depicted, with high intensity on T2-WI and no enhancement (short arrows, a). In this patient with history of neurofibromatosis, these findings are most consistent with neurofibromas
Most goiters are euthyroid and are incidentally found, although they can produce life-threatening symptoms because of airway or neurovascular obstruction. No increase in malignancy of thoracic goiter was reported compared to the simple goiter. Malignancy is found in approximately 5 % of thyroid nodules.
A heterogeneous mass extending directly from the thyroid tissue in the neck is the best clue to the diagnosis. Thyroid evaluation is usually performed using head and neck imaging protocols. MRI is able to determine the thyroid origin of the mass and is often preferred to CT due to the improved characterization of heterogeneous nodule structures without the need for IV contrast medium, as iodinated contrast medium interferes with following scintigraphy and radioactive iodine therapy for a period of 1–2 months [66]. In case of thyroid malignancy, MRI can also evaluate cervical lymphadenopathy. Recent studies have shown the possible role of MRI to differentiate malignant from benign nodules. Wu et al. [67] showed that there are significant differences of ADC values between malignant and benign thyroid nodules larger than 1 cm. With multiparametric MRI, including dynamically enhanced MRI sequences and DWI, Sasaki et al. [66] were able to differentiate malignant from benign nodules with sensitivity and specificity of 100 % and 71 %, respectively, and accuracy of 91 %. These results, although promising, require further validation.
16.4.1.3 Teratoma
Germ cell tumors are a heterogeneous group of lesions containing tissues originating from primitive germ cell layers: ectoderm, mesoderm, and endoderm. In adults, germ cell tumors represent 15 % of anterior mediastinum masses. Malignancy is more common in men. Teratoma is the most common germ cell tumor (70 %), contains tissues from all three layers, and occurs in young adults. They are classified into three subtypes: mature, immature, and those with additional malignant components. The vast majority of cases are mature teratomas containing well-differentiated tissue. They most often contain fat and are almost always benign but still have a low malignant potential. On the other hand, although often benign, immature teratomas have their malignant potential proportional to the degree of immature components of neuroectoderm and mesenchymal tissue. Teratomas with additional malignant components are rare lesions in which the teratoma is accompanied by foci of carcinoma, sarcoma, or component of other germ cell tumors [60, 62].
MRI can easily and accurately depict fat-containing teratoma, with high signal intensity on T1- and T2-weighted sequences and drop of signal intensity on fat-suppressed imaging.
As for the other germ cell tumors, a substantial number of teratomas in women are benign, whereas a high proportion of these tumors in men are malignant. Therefore, in our opinion, until proven otherwise, a teratoma in a pregnant woman should be regarded as benign lesion with malignant potential, while surgery might be delayed until delivery.
16.4.1.4 Primary Mediastinal Lymphoma
Enlarged lymph nodes in the mediastinum are usually seen with neoplastic or inflammatory diseases. The former can be primary (mediastinum lymphoma), secondary spreading of other location lymphoma, or secondary to other nonlymphomatous malignancy.
Twenty percent of mediastinal tumors in adults are primary lymphoma, usually occurring in the anterior mediastinum. Approximately 50–70 % of mediastinal lymphomas are due to Hodgkin’s disease, which has no sex predilection and presents with a bimodal age distribution in young adults, as childbearing age women and in patients older than 50 years. Non-Hodgkin’s disease in young and middle-aged adults is classified as large B-cell lymphoma.
Frequently, Hodgkin’s lymphoma appears as a homogeneous soft tissue mass in the anterior mediastinum with surface lobulation and mild-to-moderate contrast enhancement. Occasionally, there may be cystic changes and necrosis [62].
MRI is a valid modality in determining the presence and size of nodes. Morphologic MRI sequences rely only on the size, shape, contours, and homogeneity for characterization. In order to surpass the limited value of morphologic analysis, the standard of reference for lymphoma staging remains FDG-PET/CT. It is known that FDG crosses the human placenta and accumulates in the fetus, locally adding radiation to the ionizing radiation from the CT component of the examination [67].
Whole-body DWI has been successfully used for detecting and staging lymphoma, when compared to FDG-PET/CT. Recently published literature suggests that whole-body DWI should be preferred in patients particularly susceptible to radiation such as pregnant women.
16.4.2 Middle Mediastinum
The middle mediastinum is bounded superiorly by the thoracic inlet, inferiorly by the diaphragm, posteriorly by the posterior portion of the pericardium and posterior tracheal wall, and anteriorly by the anterior portion pericardium. Its contents include the heart pericardium, ascending and transverse aorta, superior and inferior vena cava, brachiocephalic vessels, pulmonary vessels, trachea and main bronchi, lymph nodes, and the phrenic, vagus, and left recurrent laryngeal nerves [59]. Differential diagnoses are based on the contents of this compartment: cardiovascular origin (e.g., ascending aorta aneurysms, pericardial cysts), cysts (bronchogenic, foregut, neurenteric), tracheal lesions, or lymphadenopathies.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree