Trial
No. of patients
Follow-up
Mortality (%)
MI (%)
Repeat revascl (%)
BARI
CABG – 914
5.4 year
1.3
4.6
8
PTCA – 915
1.1
2.1
54
EAST
CABG – 194
3 year
6.2
19.6
13
PTCA – 198
7.1
14.6
54
ERACI
CABG – 64
1 year
3.2
3.2
32
PCI – 63
0
1.8
3.2
GABI
CABG – 177
1 year
2.5
8.1
44
PCI – 182
1.1
2.3
6
CABRI
CABG – 531
1 year
2.7
3.5
6.5
PCI – 548
3.9
4.9
33.6
Bare Metal Stenting vs. CABG
As the era of balloon angioplasty gave way to stent placement, several clinical trials of bare metal stenting vs. CABG in MVD were initiated (Table 21.2). The ARTS (Arterial Revascularization Therapies Study) [22] enrolled 1,205 patients with mean age of 61 years, with diabetics comprising 19 % of the Bare Metal Stent (BMS) group and 16 % of the Coronary Artery Bypass Graft (CABG) group. The extent of disease between the two groups was well matched, with approximately 2/3 of patients having double-vessel disease and 1/3 of patients having triple-vessel disease. Left anterior descending artery involvement was present in 90 % of patients. There were no significant differences between the PCI and CABG groups in the 1-year rates of death (2.5 % vs. 2.8 %), stroke (1.7 % vs. 2.1 %), Q-wave MI (5.3 % 4.3 %), or non-Q-wave MI (0.8 % vs. 0.5 %). Among patients who survived without stroke or MI, a higher proportion of the BMS group than the CABG group (16.8 % vs. 3.5 %) needed repeat revascularization. Thus, the survival free of Major Cardiac and Cerebrovascular Events (MACCE) (a composite of death, stroke, myocardial infarction, or repeat revascularization) at 1 year was 73.8 % in the BMS group compared with 87.8 % in the CABG group (p < 0.001). At 5 years, the mortality rate was 8 % in the PCI group as compared to 7.6 % in the CABG group (p = 0.83). The incidence of composite death, stroke, or MI was numerically greater, but not significantly different between the PCI (18.2 %) and CABG (14.9 %) groups (p = 0.14). However, repeat revascularization was significantly more frequent in the stent group compared to CABG (30.3 % vs. 8.8 %, p < 0.001); additionally, there was a small excess of patients reporting persistent angina in the PCI group as compared to the CABG group (21.2 % vs. 15.5 %, p < 0.05).
Table 21.2
CABG vs. BMS
Trial | No. of patient | Follow-up | MACCE (%) | Mortality (%) | MI (%) | Repeat revascl (%) |
|---|---|---|---|---|---|---|
ARTS | CABG – 605 | 5 year | 21.8 | 8 | – | 8.8 |
PCI – 600 | 41.7 | 7.6 | – | 30 | ||
AWESOME | CABG – 232 | 3 year | – | 21 | – | – |
PCI – 222 | – | 20 | – | – | ||
MASS II | CABG – 203 | 10 year | – | 25.1 | 10.3 | 7.4 |
PCI – 205 | – | 24.9 | 13.3 | 41.9 | ||
Med t/t– 203 | – | 31 | 20.7 | 39.4 | ||
SOS | CABG – 500 | 6 year | – | 6.8 | – | 6 (2 year) |
PCI – 488 | – | 10.9 | – | 21 (2 year) | ||
ERAC II | CABG – 225 | 5 year | 24.6 | 11.5 | 6.2 | 7.2 |
PCI – 225 | 34.7 | 7.1 | 2.8 | 28.4 |
The second Argentine Randomized Study: Coronary Angioplasty with Stenting Versus Coronary Bypass Surgery in patients with MVD (ERACI II) compared BMS with CABG in patients with symptomatic MVD. Out of a total of 2,759 patients screened, 450 were randomized to either PCI (n = 225) or CABG (n = 225). Initially (for the first month), the MACCE was lower in the PCI arm as compared to the CABG arm (12.3 % vs. 36 %, p = 0.02), and at 1-year follow-up [23], there was a favorable survival benefit in the PCI arm as compared to CABG arm (freedom from mortality: 96.9 % vs. 92.5 %, p < 0.017). However, at 5-year follow-up [24], freedom from MACE was significantly lower with CABG compared with PCI (76.4 % vs. 65.3 %; p = 0.013), again driven mainly by repeat revascularization [24].
The MASS-II (Medicine, Angioplasty, or Surgery Study II) trial was a single-center study designed to compare the long-term effects of medical therapy, angioplasty, or surgical strategies among 611 patients with chronic angina, multivessel Coronary Artery Disease (CAD), and preserved left ventricular function who were appropriate candidates for all three therapies [4]. MASS II was the first randomized clinical trial with long-term follow-up (10 year) comparing all three treatment strategies for patients with MVD. Overall mortality was similar between the medical therapy, PCI, and CABG arms (2, 4, 4 %, respectively, p = nonsignificant), whereas nonfatal MI occurred in 20.7, 13.2, and 10.3 % of patients, respectively (p = 0.016), and repeat revascularization in 39.4, 41.5, and 7.4 %, respectively (p < 0.001). Patients who underwent CABG (64 %) and PCI (59 %) were more likely to be angina-free at the end of 10 years when compared to medical therapy (43 %). The incidence of stroke was similar in all three groups: 6.9 % with medical therapy, 5.4 % with PCI, and 6.9 % with CABG (p = 0.55). Notably, the occurrence of the composite of cardiac death, MI, and Cerebrovascular Accident (CVA) was similar with both PCI and CABG, but more frequent with medical therapy, refuting the contention that these early trials enrolled patients that would have done just as well with medical therapy alone.
Two other trials comparing CABG vs. BMS for MVD were the AWESOME (Angina with Extremely Serious Operative Mortality Evaluation) and SOS trials. AWESOME [25] screened high-risk patients from 16 VA centers and then randomized them to CABG (n = 232) or PCI (n = 222). The 30-day survival for CABG and PCI were 95 and 97 %, respectively. Survival rates for CABG vs. PCI were 90 % vs. 94 % at 6 months, 79 % vs. 80 % at 36 months (p = 0.46), and 73 % vs. 78 % at 5 years (p = 0.46). Similarly, 5-year survival free of unstable angina was comparable in both groups. The Stent or Surgery (SOS) trial involved 988 patients (n = 488 PCI, n = 500 CABG) randomized at 53 centers during the period from 1996 to 1999 [26]. At the end of 2 years, patients randomized to PCI had a higher rate of repeat revascularization than patients randomized to CABG (20.7 % vs. 6.0 %; p < 0.001). While the incidence of death or nonfatal Q-wave myocardial infarction was similar in both groups, death occurred in 4.5 % of the PCI group compared with 1.6 % of the CABG group (p = 0.01). At a median follow-up of 6 years, 53 patients (10.9 %) died in the PCI group compared with 34 (6.8 %) in the CABG group (hazard ratio 1.66, 95 % confidence interval 1.08–2.55, p = 0.022) driven by an excess of noncardiac deaths (25 patients in PTCA arm and 11 patients in the CABG arm), the majority being cancer related. Among diabetic patients, 17.6 % of patients died in the PCI group compared with 5.4 % in the CABG group; among nondiabetic patients, 9.8 % of patients died in the PCI group compared with 7.0 % in the CABG group.
Meta-analyses of PCI and CABG (Pre-DES (Drug Eluting Stents))
Several attempts have been made to synthesize the existing prior studies of PCI vs. CABG for MVD. A meta-analysis by Bravata et al. [27] evaluated 23 randomized trials comparing 5,019 patients treated with PCI and 4,944 with CABG. Overall, the difference in survival between the two groups was less than 1 % at 10-year follow-up. Of the six trials, which reported data on the diabetic subpopulation, there was no significant survival benefit noted with the overall rate of survival with CABG being higher by just 0.2 %. Procedure-related stroke was more common after CABG than after PCI (1.2 % vs. 0.6 %, p = 0.002). When segregating the PCI arm and comparing balloon angioplasty vs. CABG and stenting vs. CABG, there were no significant differences in the 5-year survival in either group. However, 90.2 % of CABG patients were free of repeat revascularization at 5 years compared to 53.9 % with balloon angioplasty and 59.9 % with stent placement (p < 0.001).
A pooled analysis of 3,051 patients in four randomized stent trials – ARTS, ERACI-II, MASS-II, and SOS trials – was performed by Daemen et al. [28] to evaluate the relative safety and efficacy of PCI with stenting vs. CABG at 5 years for treatment of MVD. At the end of 5 years, the cumulative incidence of death, MI, and stroke was similar between the two groups (16.7 % PCI vs. 16.9 % CABG, p = 0.69). However, the rate of repeat vascularization was significantly higher in the stent arm (29 % vs. 8 %, p < 0.0001). As a result, overall MACCE was significantly higher in the stent arm (39 % vs. 23 %, p < 0.0001). Among diabetics, there were no statistically significant differences noted in the rate of death (12.4 % vs. 7.9 %, p = 0.09) or the composite end point of death, MI, or stroke (21.4 % PCI vs. 20.9 % CABG, p = 0.9).
Hlatky performed a meta-analysis [29] of ten randomized trials of both PTCA and PCI with BMS compared to CABG for MVD. This patient-level analysis included at a total of 7,812 patients and the PCI arm included six angioplasty trials and four bare metal stent trials. After a mean follow of 5.9 years, overall death was similar in both arms (15 % CABG vs. 16 % PCI, p = 0.12). The composite end point of death or MI was also nonsignificantly different (15.4 % CABG vs. 16.7 % PCI, p = 0.47), while the rate of death or repeat revascularization was significantly lower for CABG (9.9 % vs. 24.5 %, p < 0.0001). In patients with diabetes (CABG n = 615, PCI n = 618), mortality was substantially lower in patients treated with CABG when compared to PCI (23 % vs. 29 %, p = 0.014).
Overall, these three meta-analyses of early PCI (prior to the introduction of drug-eluting stents) vs. CABG for MVD highlight the fact that when comparing “hard” clinical end points, PCI performs similarly to CABG. The main driver of differences between the two therapies is the rate of repeat revascularization, which is expectedly higher among PCI-treated patients.
Drug-Eluting Stenting vs. CABG
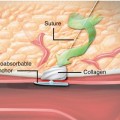
The use of drug-eluting stents has dramatically reduced the rate of restenosis and repeat revascularization procedures and revolutionized the field of interventional cardiology, making PCI possible for an expanding range of patient and lesion subsets [14, 30]. By slowly releasing a drug which can be either immunosuppressive/antiproliferative (sirolimus/everolimus/zotarolimus) or antiproliferative (paclitaxel), drug-eluting stents reduce the amount of neointimal hyperplasia within implanted stents, thereby reducing rates of restenosis and rates of repeat revascularization by 20–70 % when compared to BMS [30] (Table 21.3). Given that the primary observed disadvantage of BMS over CABG for MVD related to the rate of repeat revascularization procedures, soon after their introduction, DES were tested in the setting of MVD in several clinical trials in the hope of narrowing that difference.
Table 21.3
CABG vs. DES
Trial | No. of patients | Follow-up | MACCE (%) | Mortality (%) | MI (%) | Repeat revascl |
|---|---|---|---|---|---|---|
SYNTAX | CABG – 897 | 4 year | 23.6 | 8.8 | 3.8 | 11.9 |
PCI – 903 | 33.5 | 11.7 | 8.3 | 23 | ||
ARTS II | CABG – 605 | 5 year | 20.8 | 7.1 | 4.0 | 7.0 |
DES – 607 | 27.2 | 5.4 | 4.4 | 14.5 | ||
BMS – 600 | 41.2 | 7.8 | 6.8 | 23.3 | ||
ERAC III | CABG – 225 | 3 year | 22.7 | 9.8 | 6.2 | 5.8 |
PCI – 225 | 22.7 | 5.7 | 6.2 | 14.2 | ||
CARDia | CABG – 254 | 1 year | 11.3 | 3.2 | 5.7 | 2.0 |
PCI – 256 | 19.3 | 3.2 | 9.8 | 11.8 |
ARTS II Trial
ARTS II was a multicenter, nonrandomized, open-label trial designed to compare the safety and efficacy of the sirolimus-eluting stent (SES) in patients with de novo multivessel coronary artery disease using the surgical group of ARTS I as a historical control. ARTS II enrolled 607 patients with the same inclusion and exclusion criteria, end points, and protocol definitions as ARTS I. Despite enrolling a higher-risk population than ARTS I trial, the 5-year MACCE (a composite of death, MI, stroke, and repeat revascularization) rate with SES in ARTS II (27.5 %), while significantly higher than ARTS I CABG (21.1 %, p = 0.02), was significantly lower than among BMS-treated patients in ARTS (41.5 %, p < 0.001). At 5 years, the death/stroke/myocardial infarction event-free survival rate was 87.1 % in ARTS II SES vs. 86.0 % (p = 0.1) and 81.9 % (p = 0.007) in the ARTS I CABG and BMS cohorts, respectively. Interestingly, approximately one-third of the adverse events seen with SES in ARTS II could be attributed to early, late, and very late stent thrombosis with SES.
Using an angiographic scoring system derived from the subsequently conducted SYNTAX trial (the SYNTAX score, see below), the ARTS II investigators sought to further stratify the patients enrolled in ARTS II to assess the risk/benefit of PCI vs. CABG [31, 32]. Patients with lowest-tercile SYNTAX scores had MACCE-free survival rates greater than that of patients in the middle or highest terciles, and the SYNTAX score was an independent predictor of 5-year stent thrombosis and MACCE. Among patients with lowest-tercile SYNTAX scores, the MACCE rate was similar between SES-treated patients in ARTS II and the entire surgical cohort from ARTS I, suggesting that patients with MVD and a low SYNTAX score may be adequately treated with PCI.
ERACI-III Trial
This was a multicenter, prospective, nonrandomized, open-labeled registry that compared the various treatment options in patients with MVD; ERAC III [33] was aimed at comparing patients who received DES (n = 225) with the patients who received BMS (n = 225) and CABG (n = 225) in the ERACI-II trial after meeting similar clinical and angiographic inclusion criteria. However, when comparing the baseline characteristics between the three groups, patients in DES group were older, more often smokers, and higher risk (by EuroSCORE); had more type C lesions; and received more stents but had less frequent angina. Nevertheless, at the end of 3 years, the occurrence of the primary end point (MACCE) was similar in both DES and CABG groups (22.7 % for each, p = 1.0) and lower when compared to BMS group (29.8 %, p = 0.015) mainly due to reduced repeat revascularization in the DES group (14.2 % DES vs. 24.4 % BMS, p = 0.009). The DES group had nonsignificantly higher rates of death or MI when compared to BMS (10.2 % vs. 6.2 %, p = 0.08) but nonsignificantly lower rates than CABG (15.1 %, p = 0.07 %). Among diabetics, there was no significant difference in MACCE between the three groups (DES, 36.2 %; BMS, 43.6 %; CABG, 30.8 %; p = 0.49); however, the rate of repeat vascularization was significantly different between the three groups with lowest rates observed among patients treated with CABG (DES, 21.3 %; BMS, 38.5 %; CABG, 15.4 %; p = 0.048).
CARDia (Coronary Artery Revascularization in Diabetes) Trial
This study [34] was designed as non-inferiority trial to assess the safety and efficacy of PCI against CABG for patients with diabetes and MVD. 510 diabetic patients with MVD were randomized to PCI with stenting and routine use of abciximab (n = 256) or CABG (n = 254). Initially BMS were used for PCI (in 31 % of the overall cohort) but with the advent of DES, SES stents were ultimately used in 69 % of patients. At the end of 1 year, the rate of the composite primary end point of death, stroke, or MI was 10.5 % with CABG vs. 13 % with PCI (p = 0.39). There were no differences in rates of all-cause mortality (3.2 % vs. 3.2 %), but repeat vascularization rates were lower with CABG vs. PCI (2.0 % vs. 11.8 %, p < 0.0001). The trial did not meet non-inferiority criteria due to early termination and thus reduced sample size; however, CARDia did demonstrate that PCI was a viable option in diabetic patients with follow-up to 1 year. The upcoming results of the FREEDOM trial will hopefully add some further clarity to this issue.
The SYNTAX Trial
The Synergy Between Percutaneous Coronary Intervention with TAXUS and Cardiac Surgery (SYNTAX) trial, conducted from 2005 to 2007, has shaped much of the current thinking regarding the treatment of MVD in the era of drug-eluting stents [35]. Prior to this trial, as stated in the 2005 ACC/AHA/SCAI guideline update for PCI, CABG remained the treatment of choice for patients with severe coronary artery disease, including those with left main coronary artery disease and three-vessel disease. Due to the lack of data from adequately powered randomized trials of DES-PCI in such patients, the SYNTAX trial sought to assess the optimal revascularization strategy for patients with MVD and/or left main coronary artery disease and to define the populations of patients for whom only one or the other revascularization method would be most effective. SYNTAX was a prospective, randomized clinical trial conducted at 62 European and 23 US sites. Inclusion criteria included treatment of de novo lesions with ≥50 % target vessel stenosis in symptomatic patients (or with the evidence of myocardial ischemia in asymptomatic patients). Patients were screened for both CABG and PCI suitability by an interventional cardiologist and a cardiac surgeon at each site (a concept termed the “heart team”) and if suitable for both were randomized. Patients considered eligible for only one form of treatment were assigned to the equivalent registry. The primary analysis was non-inferiority comparison of MACCE between the two groups with the hypothesis that PCI with DES would be non-inferior to CABG at 1 year. A total of 1,800 patients were randomized to undergo CABG (n = 897) or PCI with the TAXUS Express paclitaxel-eluting stent (PES) (n = 903). Of the patients included LM disease was prevalent in 38.8 % of CABG patients and 39.5 % of PCI patients. At the end of 12 months, the primary outcome of MACCE was significantly higher with PCI (17.6 % vs. 12.3 %, p = 0.002) mainly driven by increased rates of revascularization (13.5 % vs. 5.9 %, p < 0.001); as such, the primary non-inferiority hypothesis was rejected. Interestingly, the incidence of composite death, MI, or stroke was similar in both arms at the end of 12 months (7.6 % PCI vs. 7.7 % CABG, p = 0.98), and the rate of stroke was significantly higher with CABG (2.2 % vs. 0.6 %, p = 0.003). The 12-month rate of symptomatic graft occlusion in CABG group and stent thrombosis in the PCI group was similar among both arms of the trial (3.4 % vs. 3.3 %: p = 0.89).
Several exploratory sub-analyses of the SYNTAX data have been performed in order to attempt to further define the suitability of specific subgroups of the trial for PCI vs. CABG. When comparing the two groups based on SYNTAX score terciles, MACCE at 12 months was similar in the lowest (13.6 % PCI vs. 14.7 % CABG, p = 0.71) and intermediate terciles (16.7 % PCI vs. 12.0 % CABG, p = 0.1). However, there was a statistically significant difference in highest tercile in favor of CABG (23.4 % PCI vs. 10.9 % CABG, p < 0.001). In the left main subset, there was no significant difference in MACCE at 12 months (15.8 % PCI vs. 13.7 % CABG, p = 0.44). In the 3-vessel disease subset, when comparing PCI and CABG, all-cause death (4.4 % vs. 2.9 %, p = 0.18), CVA (0.8 % vs. 1.9 %, p = 0.09), and symptomatic graft occlusion or stent thrombosis (3.7 % vs. 3.3 %, p = 0.73) were non-statistically different among the study arms. However, the rates of MI (2.6 % vs. 5.2 %, p = 0.04) and repeat revascularization (5.4 % vs. 14.7 %, p < 0.001) favored CABG.
SYNTAX at 4 Years
The 4-year results of SYNATX trial [36] have been reported on 819 patients in the CABG arm (91.3 %) and 879 in the PCI arm (97.3 %) with 78 CABG patients and 24 PCI patients lost to follow-up. The benefit of CABG continued over to the fourth year, with the MACCE rate being significantly lower when compared to PCI (23.6 % vs. 33.5 %, p < 0.001). There remain no significant differences in the rate of death, stroke, or MI between the two groups, although the rate is numerically lower with CABG (14.6 vs. 18 % with PCI, p = 0.07). At 4 years, patients treated with CABG had a significantly lower rate of all-cause mortality when compared to PCI (8.8 % vs. 11.7 %, p = 0.048), with a similar significant difference observed for cardiac death (4.3 % vs. 7.6 %; p = 0.004), MI (3.8 % vs. 8.3 %; p < 0.001), and also the rate of repeat revascularization (11.9 % vs. 23 %; p < 0.001). When comparing the stroke rates at 4-year follow-up, there was no significant difference noted (3.7 % CABG vs. 2.3 % PCI).
Due to the difference in ascertainment of follow-up between the two study arms, a sensitivity analysis was conducted assuming that all non-evaluable patients had died. In this analysis, there was still a significant difference favoring CABG for MACCE (p = 0.04), but no difference in death/stroke/MI. When analyzing the data according to the three terciles of SYNTAX scores, at the end of 4 years, there was no significant difference in MACCE between CABG and PCI in those with a SYNTAX score of 0–22 (lowest tercile) (26.1 % vs. 28.6 %; p




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree