(1)
Department of Medical Imaging, Linkou Chang Gung Memorial Hospital, Taoyuan, Taiwan
(2)
Department of Medical Imaging and Radiological Sciences, Institute of Radiological Research Chang Gung University, Taoyuan, Taiwan
1.1 Renal Agenesis
Case 1

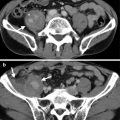
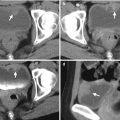
Fig. 1.1
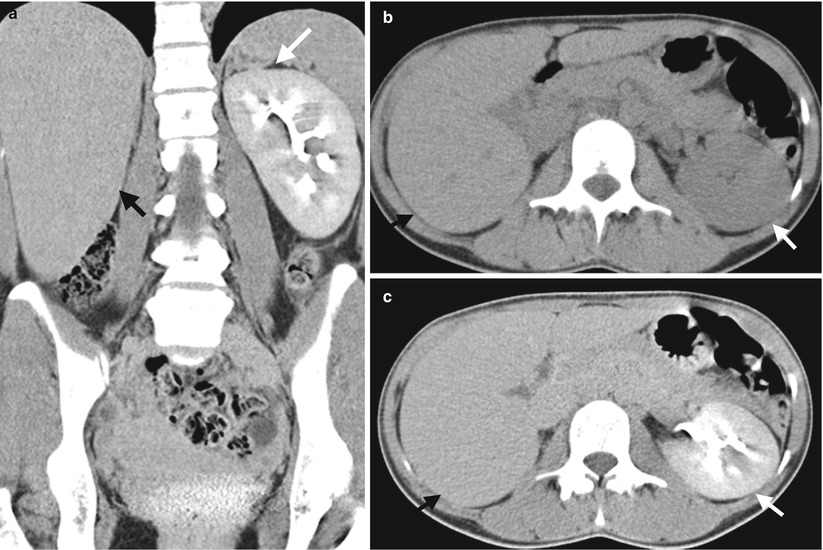
Fig. 1.2
Renal agenesis is shown on excretory urography (EU) and computed tomography (CT). Figure 1.1, EU shows a functioning left kidney excreting contrast medium to the left renal pelvicalyceal system and flowing downward to the left ureter and urinary bladder. Note nonvisualization of the right kidney. Figure 1.2, coronal reformat image of enhanced CT (Fig. 1.2a), axial image of unenhanced CT (Fig. 1.2b), and axial enhanced CT of excretory phase (Fig. 1.2c) show a normal left kidney (white arrows) located in the left renal fossa. In the corresponding anatomical location as the right renal fossa, there is absence of the right kidney. Instead, posterior segment of the right lobe (black arrows) of the liver occupies the presumed right renal fossa anatomical space.
Key Diagnostic Features
Renal agenesis is a congenital anomaly with complete absence of kidney [1]. Renal agenesis usually affects one kidney and rarely both kidneys. Renal agenesis is associated with the ipsilateral absence of the ureter and hemitrigone of the urinary bladder as well as genital or reproductive abnormalities [1]. By definition of renal agenesis, a diagnosis of renal agenesis is established by not only complete absence of a kidney in renal fossa but also in any other parts of the body. If there is any sign of residual or atrophic renal tissue on one side of the body, a diagnosis of renal agenesis should be excluded. In addition, acquired or iatrogenic loss of a kidney is not regarded as renal agenesis by its nature to be a congenital anomaly.
Main Differential Diagnoses
1.
Ectopic kidney
In the absence of a kidney in one side of the renal fossa on renal US, there are two main possible diagnoses: renal absence by renal agenesis or nephrectomy and an ectopic kidney. On EU, an ectopic kidney could be recognized and localized if it is functioning. Similarly, CT or MRI is able to localize an ectopic kidney by its reniform, anatomical structure and function.
2.
Nephrectomy [1]
Complete loss of a kidney is more commonly encountered by nephrectomy than by congenital renal agenesis. A careful search of associated findings of nephrectomy is helpful to differentiate these two conditions. In the presence of surgical clips in renal fossa or right retroperitoneum, incisional scarring at the flank, or a ligated renal arterial stump, renal absence by nephrectomy could be confidently diagnosed. On the other hand, a diagnosis of renal agenesis is more likely in the presence of its associated findings.
1.2 Floating Kidney
Case 2
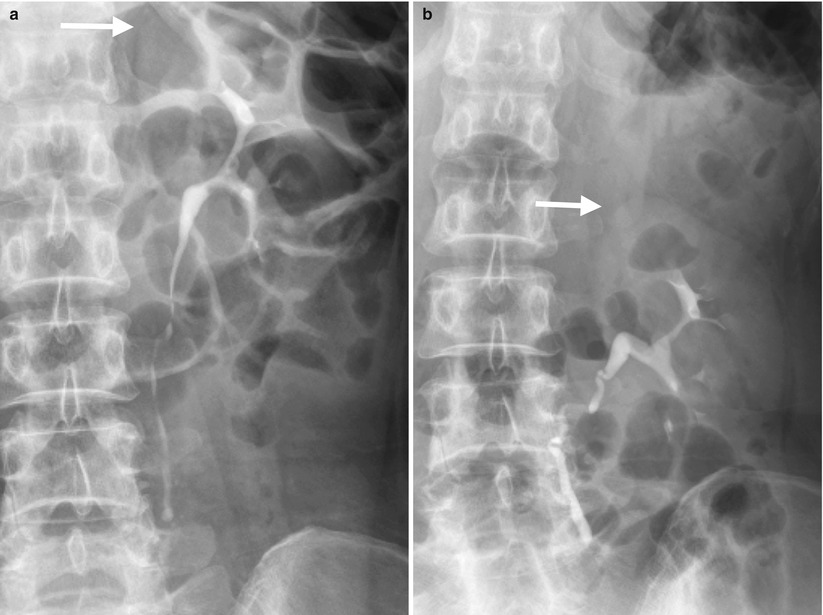
Fig. 1.3
Excretory urography (EU) shows left floating kidney. Figure 1.3, EU of supine image (Fig. 1.3a) and standing image (Fig. 1.3b) shows caudal movement of the left kidney from supine to standing positioning for more than two vertebral heights. The tip of left renal upper pole (arrows) is located at T11–T12 disc level in supine image versus at mid L2 body in standing position. Note that the left proximal ureter becomes tortuous in standing EU image because the left ureter length is fixed despite a caudal movement of the left kidney on standing.
Key Diagnostic Features
Floating kidney is also called nephroptosis and hypermobile kidney, which is diagnosed on images by mobility of one kidney for more than two vertebra heights usually from supine to standing positions [2]. It means that a diagnosis of floating kidney needs renal images of both supine and standing positions, such as excretory urography (EU), antegrade pyelography, retrograde pyelography, or plain radiographs of the kidney, ureter, and bladder (KUB), to show the positional differences between two images. On the other hand, cross-sectional images such as computed tomography or magnetic resonance imaging are usually scanned in either supine or prone positions and not able to scan in a standing position, which are not suitable for diagnosis of floating kidneys.
Main Differential Diagnoses
1.
Renal caudal ectopia
Renal caudal ectopia is characterized by abnormal caudal positioning of the kidney than normal positioning. However, renal caudal ectopic has a consistent and persistent abnormal renal caudal positioning regardless of supine or standing positioning of the patient.
2.
Caudal displacement of the kidney by suprarenal mass lesion
In the presence of suprarenal mass, caudal displacement of the kidney could be depicted if the ipsilateral suprarenal mass has a large size. Nonetheless, the difference of renal caudal displacement by a suprarenal mass between supine and standing positioning is usually limited.
1.3 Renal Ectopia
Case 3

Fig. 1.4
Excretory urography (EU) shows imaging features of left renal ectopic with malrotation of the left renal axis. Figure 1.4a, EU of supine image at 10 min after contrast medium administration shows abnormal caudal positioning of the left kidney (arrow). Malrotation of the left kidney is shown as renal calyces displaying at both medial and lateral sides of the left kidney. Figure 1.4b, EU of anterior-oblique view shows left renal caudal ectopia (arrow) and malrotation of left renal axis (white arrowheads). The left renal pelvis (black arrowhead) is abnormally caudally located as well.
Case 4

Fig. 1.5

Fig. 1.6
Excretory urography (EU) and magnetic resonance imaging (MRI) show a right thoracic kidney. EU of supine image at 30 min after contrast medium administration (Fig. 1.5) shows the right kidney with contrast opacification of the right renal collecting system (arrow) located above the liver shadow and at the right paracardiac area. Unenhanced coronal T1-weighted image (Fig. 1.6a) and axial T2-weighted image (Fig. 1.6b) on MRI show bilateral diaphragmatic eventration. The right kidney (arrows) is located at the subdiaphragmatic area of the right diaphragmatic eventration site. On the other hand, the spleen is located at the subdiaphragmatic area of the left diaphragmatic eventration site.
Case 5
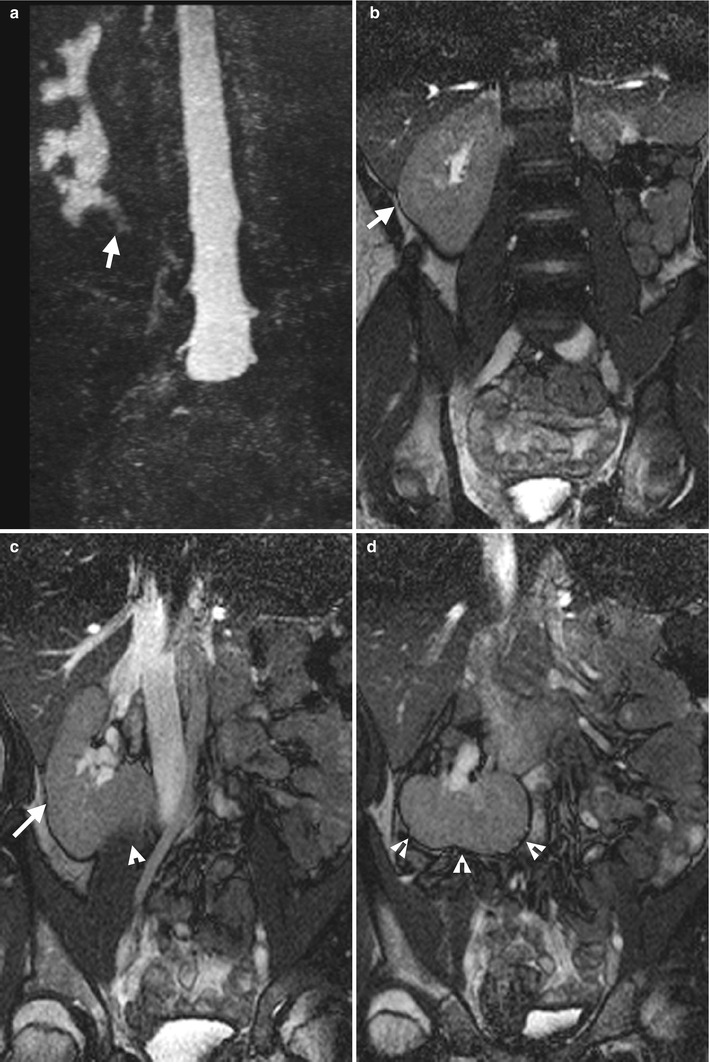
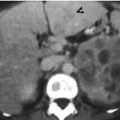
Fig. 1.7
Magnetic resonance imaging (MRI) shows a cross-fused renal ectopia. Magnetic resonance urography (Fig. 1.7a) shows an abnormally large kidney at the right abdomen with elongated appearance of the renal pelvicalyceal system and abnormal ureteropelvic junction location (arrow). Note there is nonvisualization of the renal collecting system at the left abdomen. Serial unenhanced coronal T2-weighted images (Fig. 1.7b–d) show a kidney (arrows, Fig. 1.7b, c) at the right renal fossa with normal size and appearance; however, this right kidney fuses with the left kidney (arrowheads, Fig. 1.7c, d) which crosses midline to the right side with abnormal horizontal axis.
Key Diagnostic Features
Ectopic kidney is diagnosed on images when the kidney is not completely located in the renal fossa but in other locations by a strict definition. Ectopic kidney is nearly always accompanied with anomalous renal vasculature. When an ectopic kidney is found in pelvic cavity, it is also called a pelvic kidney. Renal ectopic to thoracic region and crossing the midline to the contralateral abdominal side with fusion are rare types of renal ectopia [3, 4]. The location of an intrathoracic kidney is not truly in the pleural space [3]. Instead, an intrathoracic kidney protrudes cranially at the diaphragmatic eventration site. Malrotation of the renal axis is a common associated finding of renal ectopia. Many imaging modalities, including ultrasound, excretory urography, computed tomography, and magnetic resonance imaging, are useful for diagnosing ectopic kidneys. Ectopic kidneys are basically recognized on images by demonstrating renal imaging features and contrast excretory function [3, 4].
1.4 Malrotation of the Renal Axis
Case 6
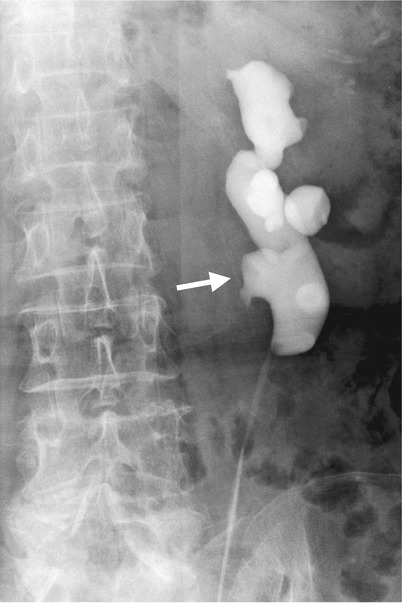
Fig. 1.8

Fig. 1.9

Fig. 1.10
Imaging features of malrotation of left renal axis are illustrated on retrograde pyelography (RP), computed tomography (CT), and magnetic resonance imaging (MRI). Figure 1.8, RP shows a renal calyx (arrow) located medial to the left renal pelvis. Figure 1.9a, computed tomography urography shows the left renal calyx (arrow) projecting medial to the left renal pelvis, similar to that shown on RP. Figure 1.9b, axial enhanced CT image of excretory phase shows the left renal pelvis (arrow) anterior to the left renal calyces, indicating malrotation of the right renal axis. Figure 1.10, an axial T2-weighted MRI image shows similar anterior positioning of the left renal pelvis, as depicted on Fig. 1.9b.
Key Diagnostic Features
Malrotation of the renal axis is considered when the renal pelvis is not located anteromedially to the ipsilateral renal calyces [5]. The most common type of malrotation of the renal axis is shown on RP or excretory urography (EU) as renal calyces locating medial to the renal pelvis. On cross-sectional imaging modalities such as CT and MRI, depicting an anterior location of the renal pelvis could also suggest the diagnosis of malrotation of the renal axis. The location of the ureteropelvic junction (UPJ) and the most proximal part of the ureter of a malrotated kidney is usually deviated more laterally than normal. Other types of malrotation of renal axis are rare, in which the renal pelvis is located either posteriorly or laterally.
Main Differential Diagnosis
1.
Hydronephrosis on EU or RP
Malrotation of the renal pelvis could result in a false-positive diagnosis of hydronephrosis on EU or RP because an anterior located renal pelvis has a prominent size on the scene by its end-on projection. Nonetheless, careful assessment of the relationships between the renal calyces and the renal pelvis as well as the locations of the UPJ and proximal ureter could help their differentiation. Furthermore, hydronephrosis is usually accompanied with hydrocalicosis which is not found in a kidney having the axis malrotation.
1.5 Horseshoe Kidney
Case 7
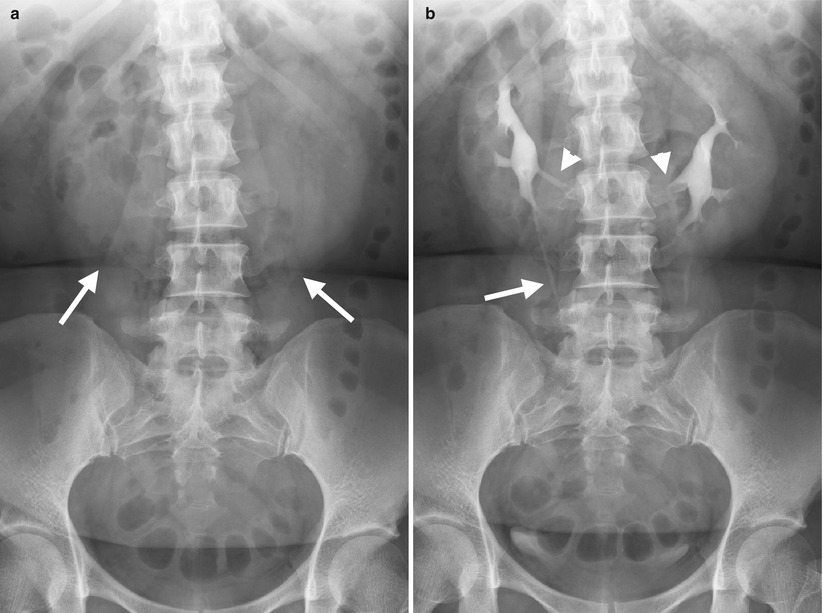
Fig. 1.11
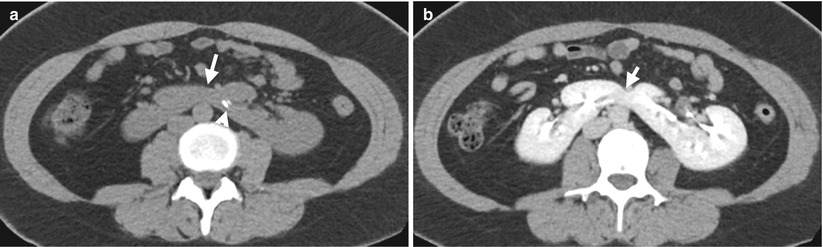
Fig. 1.12

Fig. 1.13
Excretory urography (EU) and computed tomography (CT) illustrate imaging features of horseshoe kidney connected by renal parenchymal isthmus. Figure 1.11a, the baseline plain film of the kidney, ureter, and bladder (KUB) of EU shows both renal lower poles (arrows) projecting medially and overlying bilateral psoas shadows. Figure 1.11b, EU image at 10 min after contrast medium administration shows abnormal axis of both kidneys with some renal calyces (arrowheads) projecting medial to the ipsilateral renal pelvis. Note that both kidneys form a horseshoe shape and abnormal course of the right proximal ureter (arrow). Figure 1.12, axial CT images before (Fig. 1.12a) and after contrast medium administration (Fig. 1.12b) show medial fusion (arrows) by an isthmus of renal parenchyma of both renal lower poles. Note the calculi (arrowhead) of the left renal lower calyx shown in Fig. 1.12a. Figure 1.13, left renal ultrasound shows left renal lower pole fusion to the right renal lower pole by a parenchymal isthmus (arrow).
Case 8

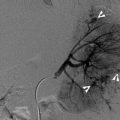
Fig. 1.14
Key Diagnostic Features
Horseshoe kidney is characterized by fusion at an isthmus between both kidneys [5], and both kidneys form a shape simulating a horseshoe. The most common type of horseshoe kidney is medial fusion of lower poles of both kidneys by an isthmus. The fusion isthmus could be formed by either renal parenchyma or a fibrotic band as shown in above illustrated images. As a result of medial fusion of lower poles, both kidneys have an abnormal renal axis, respectively. The imaging features related to abnormal axis in horseshoe kidney include: (1) lower poles which are medial to upper poles of both kidneys and the longitudinal axes of both kidneys which are no longer parallel to bilateral psoas lines, (2) anterior location of the renal pelvis of both kidneys, and (3) medial locations of some renal calyces relative to ipsilateral renal pelvis. Horseshoe kidney is associated with renal calculi and other congenital anomalies, including abnormal renal vessels, ureteropelvic obstruction, and duplex kidneys and ureters [5].
Main Differential Diagnosis
1.
Hydronephrosis on EU or RP
Malrotation of the renal pelvis could result in a false-positive diagnosis of hydronephrosis on EU or RP because an anterior located renal pelvis has a prominent size on the scene by its end-on projection. Nonetheless, careful assessment of the relationships between the renal calyces and the renal pelvis as well as the locations of the UPJ and proximal ureter could help their differentiation. Furthermore, hydronephrosis is usually accompanied with hydrocalicosis which is not found in a kidney having the axis malrotation.
1.6 Column of Bertin
Case 9
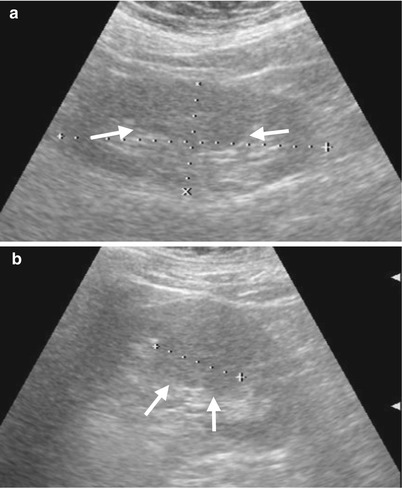
Fig. 1.15
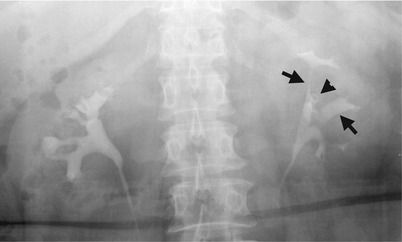
Fig. 1.16
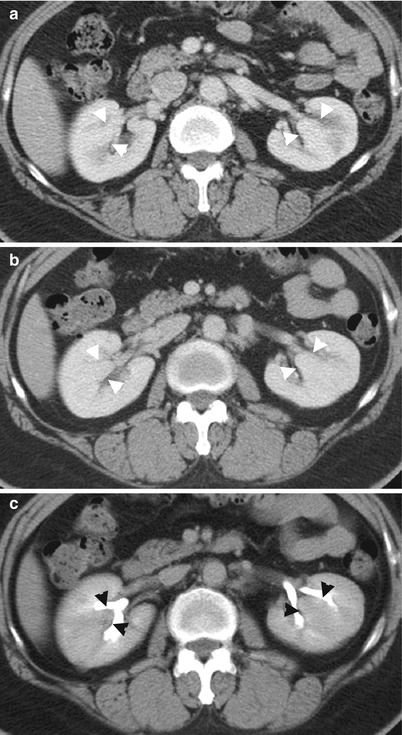
Fig. 1.17
Column of Bertin is shown on renal ultrasound (US), excretory urography (EU), and computed tomography (CT). Figure 1.15a, left renal US of longitudinal scan shows a prominent column of Bertin protruding into the renal sinus, which is isoechoic to other part of renal parenchyma. Figure 1.15b, left renal US from a different angle of Fig. 1.15a shows column of Bertin illustrating as a mass-like appearance with a measured largest diameter of 4.2 cm. Figure 1.16, EU shows wide separation of the upper and middle major infundibula (arrows) of the left kidney, simulating a space-occupying lesion (i.e., a mass lesion occupying an anatomical area or space). A subtending calyx (arrowhead) present at this location suggests the presence of column of Bertin rather than a true space-occupying lesion. Figure 1.17, enhanced CT of corticomedullary phase (Fig. 1.17a), nephrographic phase (Fig. 1.17b), and excretory phase (Fig. 1.17c) shows columns of Bertin (arrowheads) protruding into the renal sinus of both kidneys, which are isodense to other renal parenchyma on all three phases after contrast medium administration. Note the conical appearance of column of Bertin.
Key Diagnostic Features
Column of Bertin is one kind of renal pseudotumor on images if it is large in size. Column of Bertin is a normal variant having a hypertrophic renal parenchyma protruding into the renal sinus, which is most commonly seen in the junction of the upper pole and midportion of the kidney. On EU, a large column of Bertin could make upper and middle infundibula and calyces splaying over it and widely separated from each other, which may arouse a suspicion of existence of a space-occupying lesion. Nonetheless, if a subtending calyx is recognized along with the above findings on EU, column of Bertin could be diagnosed with confidence. The subtending calyx draining the papilla in the column of Bertin is a typical finding implying the correct diagnosis of the column of Bertin. Because the column of Bertin is basically a part of the normal renal parenchyma, the key diagnostic feature is to confirm if it is identical to the normal parenchyma on all situations using different imaging modalities. In other words, the column of Bertin is isoechoic to the normal renal parenchyma on renal US [6] and has identical density to the normal renal parenchyma on unenhanced CT and magnetic resonance imaging (MRI) and all phases of enhanced CT and MRI as well. As the column of Bertin is protruding into the renal sinus, it has a typically conical shape on longitudinal US as well as on CT and MRI.
Main Differential Diagnoses
1.
Renal cysts
Renal cysts could be differentiated from the column of Bertin without difficulty. On US, renal cysts are hypoechoic rather than isoechoic to normal parenchyma. On unenhanced CT, renal cysts are also hypodense to normal renal parenchyma and typically measured as −10 to 20 HU. On unenhanced MRI, renal simple cysts show low signal intensity on T1-weighted image and high signal intensity on T2-weighted imaging, reflecting its water content.
2.
Renal tumors
A renal tumor located in junction of the upper pole and lower pole could have similar appearance as the column of EU. Nonetheless, the presence of subtending calyx favors the diagnosis of column of Bertin and a diagnosis of a renal tumor could thus be excluded. In the absence of subtending calyx, enhanced CT or MRI could be used for differentiating renal tumors from the column of Bertin. Although renal tumors could be isodense to normal renal parenchyma on unenhanced CT, nearly all renal tumors do not have the same degree of contrast enhancement as that of normal renal parenchyma after contrast medium administration.
1.7 Duplex Kidney
Case 10

Fig. 1.18
Excretory urography (EU) of a child shows left duplex kidney. Figure 1.18, EU shows hydrocalicosis of the left renal upper collecting system (arrow), which is completely separated from the left renal lower collecting system (white arrowhead). Note the normal appearance of the left ureter (black arrowheads) draining the left renal lower collecting system. On the other hand, the ureter draining the left renal upper collecting system is not opacified.
Case 11
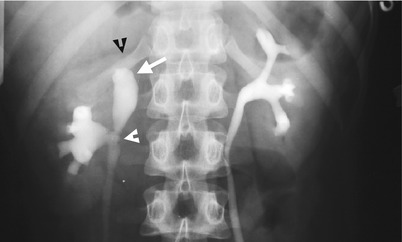
Fig. 1.19

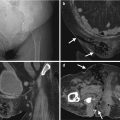
Fig. 1.20
Excretory urography (EU) studies show different appearances of a child with duplex kidney. Figure 1.19, EU shows two separate collecting systems of the right kidney. There is dilatation of the upper collecting system (arrow) with decreased corresponding parenchymal thickness (black arrowhead) of the right kidney. Note the upper and lower collecting systems of the right kidney join at the ureteropelvic junction, as bifid renal pelvis. Figure 1.20, another EU done 1 year later shows non-opacification of the upper collecting system of the right kidney by contrast medium. Note that the opacified lower moiety of the renal collecting system has a fewer number of calyx and longer distance to the right renal upper pole than normal.
Case 12

Fig. 1.21
Excretory urography (EU) of a child shows bilateral duplex kidneys. Figure 1.21, EU shows two right renal collecting systems, including upper moiety (black arrow) and lower moiety (black arrowhead). The left kidney has an opacified collecting system (white arrow) with typical drooping lily appearance. This picture suggests left duplex kidney with non-opacification of upper moiety.
Key Diagnostic Features
Duplex kidney is named for a kidney containing two separate (duplicated) renal collecting systems rather than two kidneys of one side. Therefore, a duplex kidney is diagnosed on images by identification of two separate renal collecting systems in one kidney. Excretory urography (EU), computed tomography (CT), and magnetic resonance imaging (MRI) are usually sufficient to provide imaging clues for diagnosis. A duplex kidney is also associated with the column of Bertin, which is located between upper and lower collecting systems. If renal ultrasound shows two renal collecting systems presenting with central echo complexes, separated by intervening renal parenchyma, a diagnosis of duplex kidney could be made. Nonetheless, absence of the above finding could not exclude the diagnosis of duplex kidney by insensitivity of the above sign of renal ultrasound. In addition, the duplex kidney is associated with duplex ureters, incomplete or complete types. Nonetheless, if the two separate renal collecting systems join at the ureteropelvic junction (it is called bifid renal pelvis), there is absence of duplex ureters in a duplex kidney. In patients with duplex kidney and ureters, hydronephrosis of the upper collecting system may occur. In female patients, a duplex kidney is associated with didelphys of the uterus. In the presence of hydronephrosis of the upper collecting system of a duplex kidney, non-opacification of the corresponding collecting system may occur. On EU, opacified lower moiety of the renal collecting system shows a so-called “drooping lily” sign [7], with abnormal axis not paralleling to the ipsilateral psoas line, fewer number of calyces, and lateral deviation of corresponding opacified ureter. In summary, a duplex kidney is diagnosed by two separate collecting systems in a kidney, regardless of their functioning status, and a further search of coexisting duplex ureters or other congenital anomalies should be done.
1.8 Duplex Ureters
Case 13
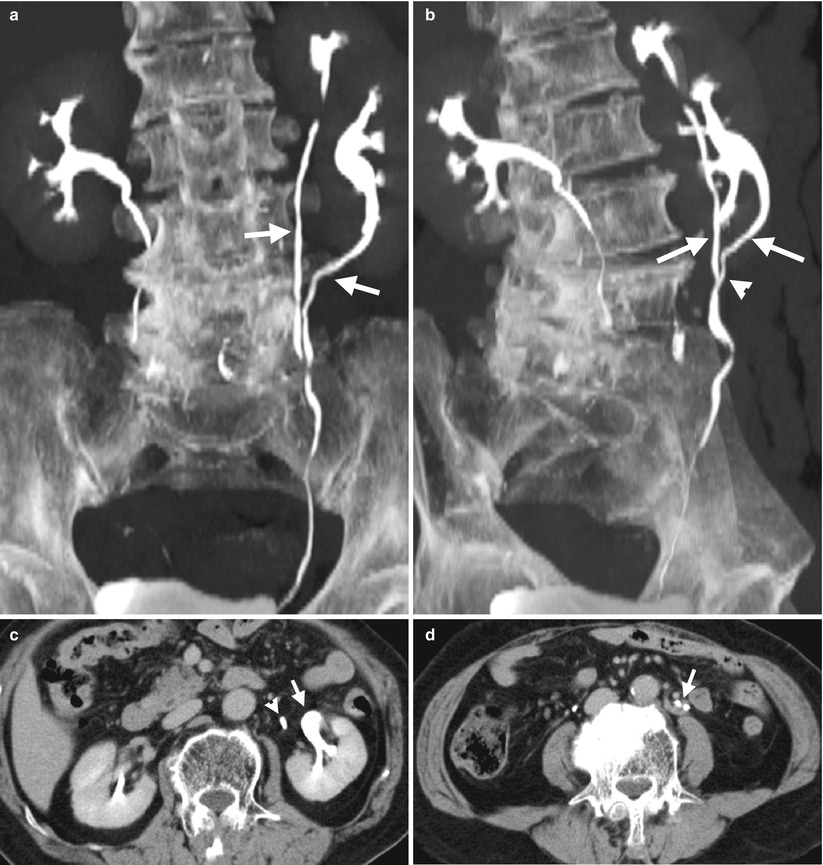
Fig. 1.22
Duplex kidney and duplex ureters are illustrated on computed tomography (CT) of excretory phase. Figure 1.22a, a coronal CT image using maximal intensity projection (MIP) shows two left renal pelvicalyceal systems. Two left ureters (arrows) are from upper and lower moieties of the left kidney, respectively. Figure 1.22b, oblique coronal MIP CT image shows fusion (arrowhead) of the two left renal ureters (arrows). Figure 1.22c, axial CT image shows a renal pelvis (arrow) of the left renal lower moiety and another ureter (arrowhead) of the left renal upper moiety. Figure 1.22d, axial CT image of the lower abdomen level shows two left ureters (arrow) running in parallel.
Key Diagnostic Features
Duplex ureters are accompanied by duplex kidney. Duplex kidney is characterized by separation of the renal pelvicalyceal systems into two parts: the cranial part is named as upper moiety and caudal part as lower moiety. If duplex ureters fuse with each other at any ureter point, it is called incomplete duplication; otherwise, it is called complete duplication. Incomplete duplication of the ureter is more common than complete duplication. In most instances, both upper moiety and lower moiety have a normal excretory function, and the presence of two ureters is thus easily depicted by contrast medium opacification on CT or excretory urography. The ureter from upper moiety is associated with ectopic insertion, ureterocele, and stenosis at the distal end, while the ureter in lower moiety is associated with vesicoureteral reflux.
1.9 Ectopic Ureter Insertion to the Vagina