Fig. 9.1
A 16-year-old boy with Crohn’s disease. The maximum-intensity-projection 18F-FDG-PET image shows a diffuse and intense radiopharmaceutical uptake in the large bowel
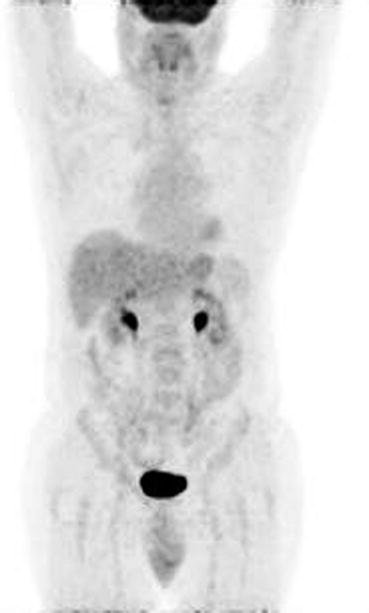
Fig. 9.2
The same patient in Fig. 9.1; 1 year later, posttreatment maximum-intensity-projection 18F-FDG-PET image shows a complete disappearance of any radiopharmaceutical uptake in the large bowel
9.3 Appendicitis
Acute appendicitis is a surgical disease, particularly difficult to diagnosis in children. Delay in diagnosis is associated with morbidity from perforation, abscess, and peritonitis. It is therefore incumbent for the management of the pediatric patients with abdominal pain to correctly diagnose in order to treat patients appropriately.
In particular, in patients with abdominal pain and atypical or equivocal signs, symptoms, or laboratory tests, adjunctive imaging studies often are used to increase early diagnostic accuracy. Other than abdominal x-rays, ultrasound probably is the most commonly used adjunctive test for the patient with an atypical presentation. However, it has an accuracy of only 30 % in patients with early appendicitis because the appendix may not display the changes required for visualization [40].
99mTc-HMPAO-labeled leukocyte imaging is highly sensitive for detecting even small inflammatory processes in the abdomen because of high target-to-background ratio and early rapid uptake at sites of inflammation [41]. In fact, 99mTc-HMPAO is an agent that complexes avidly with polymorphonuclear leukocytes, and it has a rapid uptake into areas of acute inflammation [42, 43].
An anterior image of the pelvis has to be acquired at 30–60 min postinjection, and it needs to be repeated at approximately 60 min intervals until either the scan showed abnormal uptake, indicating a positive scan, or remained negative until 3 h, at which time scanning was terminated.
There are a variety of abdominopelvic inflammatory processes that may be detected with 99mTc-WBC imaging, for example, inflammatory bowel disease, abscess, and even bowel ischemia, and often differentiating between these conditions and appendicitis is not easy to obtain, and this results in a specificity of 85 % [16]. However, this issue can be obviated if the positive scans are interpreted in light of the overall clinical picture in order to consider 99mTc-HMPAO WBC imaging as an accurate, noninvasive test to exclude appendicitis in children with clinical suspicion of the disease but with anomalous presentation.
It is noted that inflammatory lesions show an avid uptake of 18F-FDG. The high resolution of PET, especially associated to CT or MR, together with the high concentration of 18F-FDG in inflammatory tissues, makes PET a potential useful tool for an earlier diagnosis of appendicitis and other abdominal inflammatory diseases. However, the use of 18F-FDG-PET in the detection of appendicitis is rare. More often, it is an incidental finding of high 18F-FDG uptake in the right iliac fossa due to appendicitis during exams performed for malignancies. Familiarity with the normal pattern and physiologic variations of 18F-FDG distribution and with clinical data relevant to the patient can direct to a correct diagnosis, reducing a misleading differential diagnosis with tumors [44, 45].
9.4 Gastroesophageal Reflux and Esophageal Transit
Radionuclide studies for evaluating gastrointestinal transit in adults have been adapted for use in infants and children for assessing esophageal transit, gastroesophageal reflux, and gastric emptying.
9.4.1 Gastroesophageal Reflux
Gastroesophageal reflux, which is a condition characterized by the reflux of gastric and duodenal contents across the gastroesophageal junction into the esophagus, can occur in infants typically from 2 months of age. Typically, children can have symptom resolution by 18 months of age, and 30 % of them may have symptoms until the age of 4 years. The presence of gastroesophageal reflux may be related to severe complications, as strictures and pneumonia [46].
To provide information about esophageal and gastroesophageal function, nuclear medicine technique may be relevant with esophageal and gastroesophageal scintigraphy.
99mTc-sulfur colloid is often used for the assessment of gastroesophageal reflux in children, and the tracer should be added to two thirds of the feeding volume typical for the patient, with a dose of 0.1–1 mCi (3.7–37.0 MBq), in order to leave one third unlabeled to clear any remaining activity from the oropharynx and esophagus [47–49].
Gastroesophageal scintigraphy is best performed at the time of a usual feeding. Then, short-lasting 5 s anterior dynamic images are acquired for 60 min, and at the end, anterior and posterior static images of the thorax can be acquired to look for evidence of aspiration.
The dynamic images should be reviewed to recognize any episodes of reflux and regions of interest may be placed on the entire esophagus and on the upper esophagus to aid in the analysis of data and in order to demonstrate the number of episodes of reflux and level reached within the esophagus, and the clearance rate of reflux episodes may then be determined.
9.4.2 Esophageal Transit
Radionuclide-esophageal transit studies have been performed in infants, usually as part of the evaluation for reflux or in the evaluation of patients with esophageal motility disorders such as achalasia, diffuse esophageal spasm, nutcracker esophagus, tracheoesophageal fistula, Down syndrome, esophagitis, systemic sclerosis, and diabetes mellitus.
Other diagnostic methods, as esophageal manometry, contrast radiography, and endoscopy, may be used to assess esophageal peristalsis, anatomical lesions, and mucosal lesions, but the advantages of esophageal scintigraphy include its noninvasive nature, quantifiability, and low radiation burden. Its clinical application has been suggested to be useful when the other procedures are unavailable or not tolerated by the patient or when the results are equivocal [49–55].
A 10 mL bolus of water or milk labeled with 150 μCi (5.55 MBq) of 99mTc-sulfur colloid is administered to the patient in the supine position. Posterior images at 0.4 s intervals for 150 frames are acquired, including the mouth and stomach, in the camera field of view. A radioactive bolus is placed in the mouth and swallowed on command followed by a dry swallow 30 s later. Abnormal studies may be repeated in the upright position to determine the effect of gravity.
Image analysis is performed by the evaluation of time activity curves derived from regions of interest placed on the upper, middle, and lower thirds of the esophagus and on the stomach. This procedure may demonstrate abnormal esophageal transit in pathologic states and may also visualize esophageal transit condensing dynamic images.
Usually, the normal transit time through the esophagus is typically less than 10 s. Esophageal transit ranges from 3.4 ± 1 s for infants to 4.6 ± 1.9 s for patients 8–16 years of age. Gastroesophageal reflux and esophagitis are associated with prolonged transit times [56].
9.4.3 Gastric Emptying
Patients with abnormal gastric emptying may present nausea, vomiting, abdominal discomfort, early satiety, diarrhea, and “dumping.”
The correct assessment of gastric emptying helps to guide treatment decisions, particularly in the neurologically impaired children that frequently demonstrate symptomatic delayed gastrointestinal motility.
Furthermore, delayed gastric emptying may be secondary to several pathological conditions, as pyloric or duodenal stenosis, acidosis, hypothyroidism, autonomic neuropathy associated with diabetes mellitus, central nervous system disease, systemic lupus erythematosus, dermatomyositis/polymyositis, infection, and many others.
The rate of gastric emptying assessed scintigraphically has been shown to depend on the type of meal used: liquids typically empty faster than solids.
In infants, a milk or formula feeding is usually administered and the type of milk and volume fed should be standardized according to patient size. However, many of the patients studied have feeding difficulties and in these cases is difficult to standardize the volume fed.
The dose of 99mTc-sulfur colloid added to the milk depends on whether gastric emptying is performed in conjunction with the reflux study.
If only the rate of emptying is of interest, this dose can be decreased to 100 μCi (3.7 MBq).
In older children, solid gastric emptying may be performed by having the patient eat an egg sandwich containing 99mTc-sulfur colloid (250–300 μCi). The meal should be scaled according to patient size (where adults are given 4 eggs and 50 mL of water). Thirty second anterior images are acquired every 10 min. Between images, the patient should sit upright. Images are acquired until 120 min.
A region of interest is drawn around the stomach. Activity from the bowel should not be included in the region of interest.
The range for normal gastric emptying has been difficult to establish in children for ethical reasons. Furthermore, the test meals have not been standardized. In general, laboratories have to decide on the values to be used based on their own experience. A study performed several years ago in children thought to be normal retrospectively shown, for milk, a residual of 36–68 % at 60 min and 42–56 % in a small number of older children [57].
In another report using dextrose as the test meal, the 60 min residual was 27–81 % in children under 2 years of age and 11–47 % in older children. This age-related difference in emptying rate has been observed by others, although the composition of the meal may also play a role [58].
9.5 Hepatobiliary Scintigraphy
Hepatobiliary scintigraphy is useful in the assessment of patients with right upper quadrant pain, in particular if there is the suspicion of acute cholecystitis. Cholecystitis is less common in children than in adults, but its incidence in pediatric patients has probably been underestimated [59, 60].
It is possible to recognize two types of cholecystitis: acute calculous cholecystitis, which occurs when the cystic duct becomes obstructed by gallstones leading to gallbladder distension and edema, and acalculous cholecystitis, which can occur in prolonged illness, sepsis, or trauma.
Both of these conditions may be associated with inflammation and edema and consequently with blood flow impairment and bacterial infection advancement.
Typically, the most common symptoms in children are abdominal pain localized in the right upper quadrant or epigastric region. Other symptoms include nausea, vomiting, anorexia, and fever for several days.
The most common clinical signs are represented by a right upper quadrant tenderness, jaundice, and enlarged and palpable gallbladder. Regarding the laboratory tests, leukocytosis is a common finding [61–63]. In the diagnosis of cholecystitis, ultrasound is basic in the evaluation of the biliary tract and detecting gallstones; however, its diagnostic accuracy presents a substantial margin of error. In a recent systematic review of different imaging modalities in patients with suspected acute cholecystitis [64], hepatobiliary scintigraphy is the most accurate diagnostic imaging modality for acute cholecystitis, with a sensitivity and specificity for hepatobiliary scintigraphy of 96 % and 90 %, respectively. The sensitivity of hepatobiliary scintigraphy results significantly higher than ultrasound (81 %).
99mTc-disofenin or 99mTc-mebrofenin is administered intravenously, with a dose for infants and children of 1.85 MBq/kg (0.05 mCi/kg). Mebrofenin is always preferred in jaundiced infants with hyperbilirubinemia, with a minimum administered activity of 37 MBq (1.0 mCi), as up to 24 h delayed images are often required. The patient should be fasting for 4 h prior to the test. Immediately after the injection, dynamic imaging is acquired for 60 min (0.5–1 min/frame) in anterior projects using preferably a high-resolution collimator and 128 × 128 matrix. Additional views such as right lateral and left or right anterior oblique may be performed, if required. When acute cholecystitis is suspected and the gallbladder is not seen within 60 min, delayed images for up to 4 h should be obtained [65].
In adult patients, acute cholecystitis is associated with non-visualization of the gallbladder on hepatobiliary scintigraphy, and the visualization of gallbladder activity excludes the diagnosis of acute cholecystitis with high accuracy. However, in children, the presence of cholecystitis is not entirely excluded if there is gallbladder visualization, because this is possible in acalculous cholecystitis [46]. After 60 min images, if the gallbladder is visualized, it is possible to perform additional dynamic imaging for 60 min following infusion of 0.02 μg/kg sincalide, a synthetic C-terminal octapeptide of cholecystokinin. Poor contraction and emptying of the gallbladder following sincalide may occur in partial cystic duct obstruction, acalculous cholecystitis, or chronic cholecystitis.
Hepatobiliary scintigraphy in children can also be used for the evaluation of choledochal cyst and biliary leak. Biliary atresia is characterized by obliteration or discontinuity of the extrahepatic biliary system, resulting in obstruction of bile flow [66]. The disorder represents the most common surgically treatable cause of cholestasis encountered during the newborn period. If not surgically corrected, secondary biliary cirrhosis invariably results. In infants, hepatobiliary scintigraphy is used to differentiate biliary atresia from hepatocellular disease [67]. The disorder, if not surgically corrected, results in secondary biliary cirrhosis. Thus early diagnosis of biliary atresia remains imperative, and the gold standard within the diagnostic modalities is liver biopsy and/or intraoperative cholangiogram. Studies have demonstrated 100 % sensitivity of 99mTc-mebrofenin hepatobiliary scintigraphy (HIDA scan) for picking up biliary atresia, and its specificity has been reported to range from 88.6 to 92 % [68, 69].
The premedication with phenobarbital or ursodeoxycholic acid before hepatobiliary scintigraphy may increase bile secretion and improves the diagnostic differentiation between biliary atresia and neonatal hepatitis [65]. The administered activity for infants and children is 1.8 MBq/kg (0.05 mCi/kg), with a minimum administered activity of 18.5 MBq (0.5 mCi). Mebrofenin is always preferred in neonates with hyperbilirubinemia, with a minimum administered activity of 37 MBq (1.0 mCi), as up to 24 h delayed images are often necessary [67].
For the image acquisition [67], a large-field-of-view γ-camera equipped with a low-energy all-purpose or high-resolution collimator is recommended. Whenever possible, continuous (dynamic) computer acquisition (usually in the anterior or left anterior oblique view) should be performed (1 frame/min). The image matrix of 128 by 128 is optimal on a standard large-field-of-view camera. In pediatric patients, an appropriate electronic acquisition zoom should be used. Initial images are usually acquired dynamically, starting at injection and continuing for 60 min. When visualization of the gallbladder is the end point of the study, it can be stopped earlier when activity is seen in the gallbladder. Additional views (e.g., right lateral, left or right anterior oblique) may be obtained as needed to clarify anatomy. To resolve concern about common bile duct obstruction (highly unlikely in the presence of gallbladder visualization), demonstration of tracer activity in the small bowel may need to be pursued.
The digital data can be reformatted to 4 to 6 min images for filming or digital display. Cinematic display of the data may reveal additional information not readily apparent on reformatted display. Image intensity scaling should be study relative rather than individual frame relative. The former allows for appreciation of activity changes over the duration of the study.
If there is visualization of the biliary drainage of the radiotracer into the bowel, scintigraphy can exclude the presence of biliary atresia. If no bowel activity is detected up to 24 h and liver uptake is normal, the diagnosis of biliary atresia is suspected [46, 67]. If the patient is being studied for a biliary leak, 2 to 4 h delayed imaging (or longer delays in some cases) and patient-positioning maneuvers (e.g., decubitus views) may be helpful. Any drainage bags should be included in the field of view if the biliary origin of a leak or fistula is in question. In patients with a suspected leak, it may be helpful to acquire simultaneous right lateral or other views on a multihead camera.
However, normal liver uptake of tracer with no excretion up to 24 h can occur in severe cases of neonatal hepatitis, Alagille syndrome, dehydration, sepsis, TPN cholestasis, and bile plug syndrome in cystic fibrosis. Neonatal hepatitis typically demonstrates reduced hepatocyte uptake and delayed hepatobiliary transit of tracer into the bowel [46]. Failure of tracer to enter the gut is consistent with biliary atresia but can also be caused by hepatocellular disease or immature intrahepatic transport mechanisms. Renal or urinary excretion of the tracer (especially in a diaper) may be confused with bowel activity and is a potential source of erroneous interpretation [67].
An interesting application of 18F-FDG PET in this setting is its use in children with biliary cirrhosis and fever of unknown origin (FUO) on the waiting list for liver transplantation. Infection imaging with FDG-PET relies on the fact that granulocytes and mononuclear cells use glucose as an energy source specifically during their metabolic burst upon activation by triggers. The advantages of FDG-PET are early imaging after injection, higher resolution and higher target-to-background ratio, sensitivity to chronic low-grade infections, and high interobserver agreement [70].
Systemic infections are considered to be contraindications for liver transplantation; however, hepatic infections are frequently only cured by the removal of the infected organ during transplantation. Therefore the information obtained by FDG-PET imaging to identify intrahepatic infections may be crucial for the management of patients with FUO awaiting liver transplantation [71].
9.6 Hyperinsulinism
Congenital hyperinsulinism (CHI) is a rare disease of hypoglycemia due to dysregulated and excessive insulin secretion, with an incidence of severe cases estimated at 1:50,000 and the incidence rising in consanguineous populations [72, 73].
In infants, the treatment of congenital hyperinsulinism is required to prevent possible neurologic complications. Forty percent of cases of hyperinsulinism in children results from pathologic adenomatous pancreatic β-cells. Diffuse hyperinsulinism involves the whole pancreas with enlarged abnormal β-cell nuclei. Ten percent of cases of infantile hyperinsulinism are atypical and fit neither classification. Focal hyperinsulinism is cured by resection of the adenoma, whereas diffuse pancreatic involvement may be treated with subtotal pancreatectomy. [74, 75].
Positron emission tomography (PET) using 6-L-(18)F-fluorodihydroxyphenylalanine ((18)F-DOPA) may be useful for classifying pancreatic involvement in infantile hyperinsulinism as focal or diffuse and can be used preoperatively to identify the two forms of infantile hyperinsulinism, differentiating between patients who should receive curative focal pancreatic resection and those who should receive medical management [76, 77]. (18)F-DOPA is a radioactive isotope of L-dihydroxyphenylalanine (L-DOPA), an intermediate in the catecholamine synthesis pathway. L-DOPA is avidly taken up by neuroendocrine cells, including CHIb-cells, while uptake is minimal in the normal pancreas. It is not understood why CHI pancreatic tissues exhibit more a differential uptake and retention pattern than normal tissue, particularly as CHI is not apparently linked with altered catecholamine metabolism.
Initial observations showed a high sensitivity (88–94 %) and specificity (100 %) of (18)F-DOPA PET imaging in differentiating focal from diffuse CHI [78, 79] which was further enhanced by the concurrent use of CT angiography using iodine-based dyes. The latter is useful to localize the site of the lesion, in relation to anatomical structures, which is particularly useful at the time of focal lesionectomy. Although meta-analyses of (18)F-DOPA PET imaging studies indicate good diagnostic performance [80, 81], recent studies have suggested that the predictive value of scanning may not be as accurate as initially estimated [82, 83].
9.7 Protein-Losing Enteropathy
Protein-losing enteropathy can be the result of primary intestinal lymphangiectasia or secondary intestinal lymphangiectasia in association with cardiac diseases or obstructed lymphatics. Abnormal or inflamed mucosal surface secondary to intestinal inflammation/infection and immunologic, inflammatory, and vasculitic disorders can also cause enteric protein loss [84].
This pathophysiologic condition generally results from an abnormal mucosal permeability, desquamation, inflammation, or back pressure in the intestinal lymphatic network [85].
The protein loss is nonselective and includes plasma proteins such as albumin, globulins, and transferrin. Radiolabeled proteins that have been used for determining enteric protein loss include 131I-albumin, 51Cr-albumin, and 67Cu-ceruloplasmin [84].
99mTc-human serum albumin (HSA) has been successful in localizing the site of enteric protein loss in adults [86–92]; however, the literature is lacking concerning pediatric patients [93–95].
A study performed on children [96] reported that the scan has a higher sensitivity in patients with lower albumin and total protein values, presumably reflecting a higher rate of protein loss; they submitted all patients to an anterior abdominal scintigraphy after the intravenous injection of freshly prepared 99mTc-HAS. The administered age-adjusted doses were 185–503 MBq based on an adult dose of 740 MBq. They acquired dynamic images every minute for 1 h, using an all-purpose collimator and a large-field-of-view γ-camera. Additional delayed images were obtained at 2–6 h in most patients and 24 h in a few patients.
They found enteric 99mTc-HSA uptake in 67 % of the children, suggesting the site of protein loss. The location of the uptake was most likely in the small bowel in 91 % of the early images and in 27 % of the delayed images. Colonic activity was noted in 72 % of the delayed images, most likely representing transit of activity rather than a second site of protein loss.
9.8 Colonic Transit
Two different types of chronic functional constipation have been identified in children based on colonic transit time measurement: a more generalized and severe form known as slow transit constipation and a segmental type known as functional fecal retention [97].
Both entities present with similar symptomatology but involve different pathophysiological mechanisms and require different treatment strategies.
It has been shown that children thus classified respond to different treatment strategies. Only a small proportion of cases require surgical intervention such as appendicostomy, colostomy, or colonic resection [99–101]. The different types of abnormal colonic transit can be identified using radiopaque markers: slow transit (pancolonic or globalized delay), normal transit, and functional fecal retention (outlet obstruction or distal obstruction) [98]. Colonic transit scintigraphy can aid in the identification and therapeutic decision-making in patients with functional fecal retention, the most common cause of chronic constipation in children [102].
This method has been used to determine colonic transit in adults with chronic constipation, and the reported advantages, compared with radiopaque marker studies, include a low radiation dose and the acquisition of multiple images allowing estimates of gastric, small bowel, and segmental colonic transit to be made [103, 104].
Intake of laxatives has to be stopped 5 days before the transit studies, and fasting is required for 4 h before the start of the test. The radiopharmaceutical 99mTc-calcium phytate colloid, suspended in 20 mL of milk, can be administered by mouth. The dose is determined according to each patient’s weight and is based on an adult dose of 250 MBq. Anterior and posterior view images are obtained immediately after ingestion and during the subsequent 2 h to estimate gastric emptying. Three categories of colonic transit could be readily distinguished by visual assessment of the acquired images. In studies considered to demonstrate normal transit, the tracer reached the cecum by 6 h, passed through the colon, and was largely excreted by 48 h. Slow transit was identified when the tracer reached the cecum at 6 h, but most radioactivity was retained in the proximal colon and transverse colon at 24, 30, and 48 h. Patients in whom the tracer reached the rectosigmoid by 24–30 h but was not passed at 48 h were appreciated. This pattern was defined as consistent with functional fecal retention or outlet obstruction.
9.9 Gastrointestinal Bleeding
Gastrointestinal (GI) bleeding is often encountered in daily clinical settings. Dramatic advances in endoscopic technology in recent years have facilitated diagnosis and treatment of bleeding from the esophagus, stomach, and duodenum, as well as most cases of bleeding from the large intestine. Although it is now possible to observe the small intestine using video capsule endoscopy and double-balloon enteroscopy [105], diagnosing the source of GI bleeding and providing treatment remain the challenges in some patients [106].
GI bleeding scintigraphy is a noninvasive examination that enables detection with a bleeding rate as low as 0.1 mL/min [107]. In children, while most gastrointestinal bleeding may not be life threatening, it is necessary to determine the source, degree, and possible cause of the bleeding and to distinguish minor from major bleeding [108]. In the stable child with occult bleeding, management is geared toward making the diagnosis and excluding more serious conditions. Investigations are directed by the history and physical examination, but most diagnostic tests can be performed on an outpatient basis [109].
99mTc-red blood cell (RBC) scintigraphy generally is useful for assessing GI bleeding in patients. Meckel’s diverticula also may be identified through this technique, although other causes of bleeding may include intussusception, IBD, Henoch-Schonlein purpura, gastritis, duodenitis, Mallory-Weiss tear, infectious enterocolitis, allergic enterocolitis, midgut volvulus, polyps, tumors, vascular malformations, enteric duplication cysts, nodular lymphoid hyperplasia, hemolytic uremic syndrome, and foreign body and trauma [110].
The main advantage of the use of 99mTc-RBCs is the possibility of visualization of GI bleeding over the course of several hours. Bleeding rates as low as 0.1–0.4 mL/min may be detected. Large bowel endoscopy of actively bleeding patients has a low diagnostic yield and is potentially harmful to the patient, and the small bowel is not successfully visualized endoscopically. Angiography typically localizes bleeding when the rate is greater than 1 mL/min. However, for bleeding to be identified, it should occur during the 20 to 30 s time interval during which contrast is administered. Scintigraphy permits the visualization of the entire GI tract.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree