Fig. 12.1
TWB vs. LWB. Differences are the acquired field of views. The commonly used limited whole body field of view (left) from the base of the skull to the upper thighs
12.2.3 18F-fluoride
18F-fluoride is a sensitive agent for detecting altered osteogenic activity with a mechanism of uptake similar to that of 99mTc-MDP (Fig. 12.2). The radiotracer accumulates in the vicinity of metastatic lesions in bone like MDP. However, 18F-fluoride has the advantage of faster blood clearance and higher bone uptake. Deposition of the radiotracer in bone is secondary to the blood flow to the bone as well as the efficiency of the bone to extract the fluorine ions from the blood which are not bound to serum proteins [30]. Given these characteristics, studies have shown that this is more accurate and sensitive for detection of bone metastasis when compared to the current gold standard bone scan as well as MRI [31]. However, one of the drawbacks to this modality is the lack of physiologic information in regard to the soft tissues. At times, both 18F-FDG and 18F-fluoride studies are needed on a given patient. This is typically done as two separate studies on different days which are both inconvenient for the patient and increases radiation exposure from the CT component of both studies. Some have suggested that both 18F-FDG and 18F-fluoride can be combined in a single PET/CT scan by administering the two radiopharmaceuticals simultaneously or in sequence. Preliminary studies have shown this to increase the sensitivity for detecting bone lesions compared with 18F-FDG which only scans with the benefit of additional soft tissue evaluation [32].
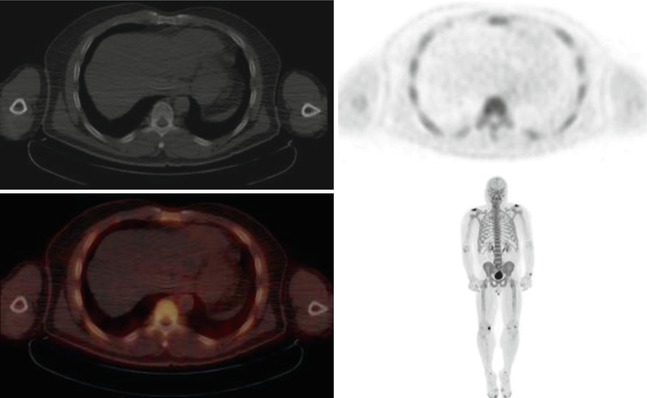
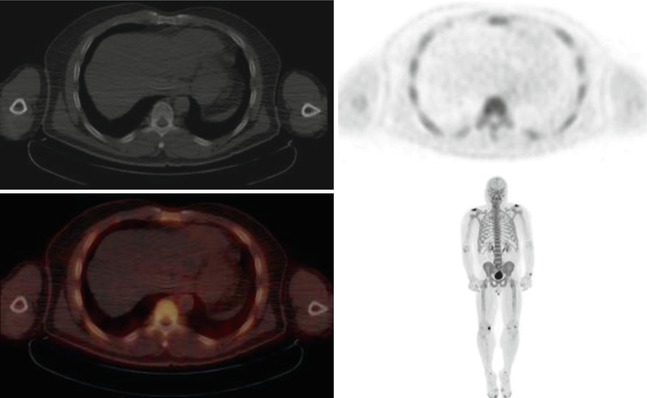
Fig. 12.2
A 57-year-old male patient with a history of prostate cancer. NaF PET/CT images demonstrate a normal radiotracer distribution throughout the skeleton with areas of focal uptake in the shoulders, wrists, knees, and feet which are consistent with degenerative arthropathy
12.2.4 Proliferation Agents
Currently, only 18F-FDG is widely accepted and used in clinical practice for proliferation imaging. 18F-fluorodeoxythymidine (18F-FLT) is an amino acid agent labeled with 18F that can be used to measure tumor cell proliferation [33, 34]. The agent is transported into the cell by the same nucleoside carrier as thymidine [35]. The agent is then phosphorylated within the cell by thymidine kinase-1 (TK1) which is upregulated in rapidly dividing tumor cells (thymidine kinase activity is a marker of cellular proliferation) [33, 36]. Because 18F-fluorodeoxythymidine is resistant to catabolism by thymidine phosphorylase, there is prolonged intracellular retention of the agent [33]. Based on 18F-FLT uptake, an overall reduction in the proliferative activity of gross tumor volumes was observed across the duration of treatment. This information may be useful to monitor changes in cellular proliferation occurring during treatment, to provide valuable prognostic information, and to adapt treatment based on individual biologic response [37].
Other agents of cell growth and proliferation imaging are based on utilization of the uptake of the molecules that are needed for synthetic pathways, including labeled amino acids for measuring transport and protein synthesis and nucleosides for DNA synthesis. Example of such agent to track cancer cell proliferation is C-11 thymidine, which is taken up into DNA but not by RNA to map proliferation. 11C-methionine is another example, which seeks amino acid transport. A higher correlation with proliferation of lung tumors was seen for (11)C-4DST than for (18)F-FDG [38]. C-11-labeled agents however have very short half-life. For this reason, F-18-radiolabeled tracers are preferred. This radiotracer was also used to evaluate the response to radiation therapy in patients with lung cancer (NSCLC).
11C-choline (11C-CHOL) is an agent that is incorporated into tumor cells by conversion into 11C-phosphorlycholine which is trapped inside the cell. This is followed by synthesis of 11C-phosphatidylcholine which constitutes a main component of cell membranes. Because tumor cells duplicate very quickly, the biosynthesis of cell membranes is also very fast, and there is increased uptake of choline and upregulation of the enzyme choline kinase [39]. Essentially, the uptake of 11C-CHOL in tumors represents the rate of tumor cell proliferation [40]. 11C-CHOL is very rapidly cleared from the blood, and optimal tumor-to-background contrast is reached within 5 min [39, 41].
12.2.5 Hypoxia Agents
It has been established that hypoxic tumor cells are more resistant than aerobic cells to ionizing radiation and chemotherapy. Hypoxic cells are more resistant to radiation therapy and therefore require additional radiation to achieve adequate cell killing, which might exceeds the tolerance of the surrounding normal tissues, called the tumor bed [42, 43]. Accordingly, tumor hypoxia is an important factor in relapse-free survival. The potential importance of tumor hypoxia as a cause of treatment failure in patients treated with radiation has been recognized for a long time. Methods have been developed to add compounds to act as hypoxic cytotoxin to potentiate the effect of radiation. Accordingly, evaluation of tumor hypoxia can help in patient’s management. PET/CT imaging using F-18-misonidazole (FMISO) is used in evaluating hypoxia and in evaluating prognosis in patients receiving radiation therapy and certain chemotherapy [44, 45].
18F-fluoromisonidazole (18F-FMISO) acts as a bioreceptor molecule and is incorporated into cell constituents under hypoxic conditions [42]. Unfortunately, there is slow cellular uptake and slow washout from non-hypoxic tissues. 62Cu-ATSM is another tumor hypoxia agent, which accumulates in hypoxic tissues where it is reduced, trapped, and has the advantage of rapid clearance from non-hypoxic tissue [42, 43].
12.2.6 68-Ga-DOTATOC and 68-Ga-DOTATATE
The increased expression of somatostatin receptors is a unique characteristic of neuroendocrine tumors. 68-Ga-DOTATOC and 68-Ga-DOTATATE are two radiolabeled somatostatin analogs for the diagnosis and pretreatment evaluation of neuroendocrine tumors with PET. There are five types of somatostatin receptors characterized (sst1 to sst5), but sst2 is the predominant one in neuroendocrine tumors [46]. The semiquantitative measurements such as SUV have been shown to be helpful in the assessment of response to therapy. Recent studies demonstrated that the sensitivity of these agents was up to 96 % with a specificity of up to 100 % in the diagnosis of neuroendocrine tumors on PET. In addition, this was found to be superior than conventional somatostatin receptor scintigraphy and diagnostic CT in diagnosis, staging, and restaging [47–49]. In addition, DOTATOC and DOTATATE can be labeled to Yttrium-90 for therapy of neuroendocrine tumors. However, this is beyond the scope of this chapter.
12.3 PET Imaging Interpretation
12.3.1 Normal Distribution
The normal pattern of 18F-FDG uptake on PET imaging performed approximately 1 h after intravenous administration reflects glucose metabolism and includes the brain, heart, kidneys, ureters, and bladder. The prominent uptake in the urinary tract is secondary to the clearance of the tracer. The brain typically demonstrates intense uptake when compared to the remainder of the body since it is an obligate user of glucose (Fig. 12.3). There is variable uptake in the heart which is based on the type of fuel being used for metabolism. In a prolonged fasting state (typically greater than 12 h), the metabolism shifts from glucose to free fatty acids resulting in an uptake similar to background activity. The liver and spleen demonstrate variable uptake but are most often greater than background with liver being slightly more prominent than the spleen. Bowel and stomach uptakes are seen with varying degrees and can be influenced by outside factors including medications such as the case of intense bowel uptake in diabetic patients on metformin. Uptake in the oropharynx can be variable as well including the salivary and parotid glands. Intense uptake is often seen in the pharyngeal and lingual tonsil. This uptake is often symmetric, but normal asymmetry is also seen [50, 51].
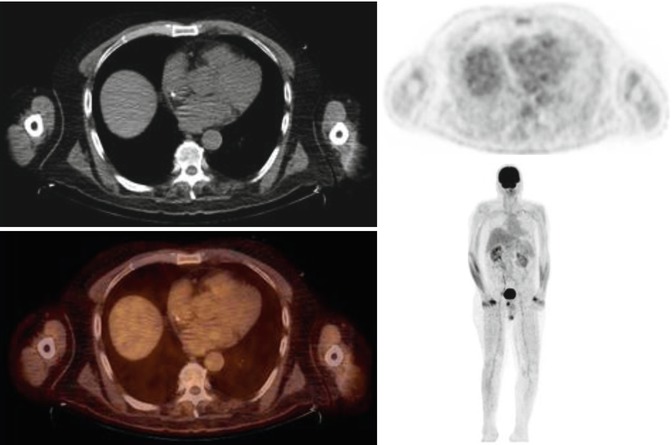
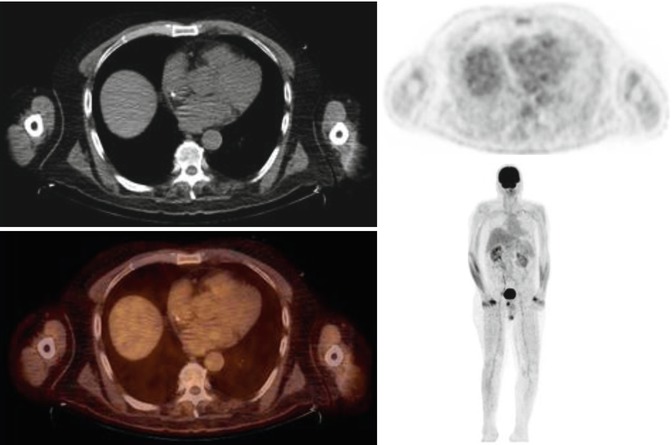
Fig. 12.3
A 64-year-old male with a history of lymphoma. PET/CT images demonstrate a normal distribution of radiotracer. Note physiologic activity in the forearm muscles and excretion of the FDG by the kidneys and urinary bladder
12.3.2 Benign Normal Variants
Skeletal muscle at rest demonstrates low FDG uptake. However, muscle uptake will increase when there is active contraction of muscles during the uptake phase or with heavy exercise within 24 h prior to the exam. Elevated insulin levels may also cause the same effect [52]. In addition, patients with labored breathing or COPD can demonstrate uptake in the diaphragm, intercostal, and scalene muscles depending on the severity (Fig. 12.4) [53]. Patients with head and neck cancers who have undergone surgery can demonstrate unilateral uptake in the vocal cord secondary to paralysis of the contralateral cord. This will also cause asymmetrical muscular uptake in the head and neck.
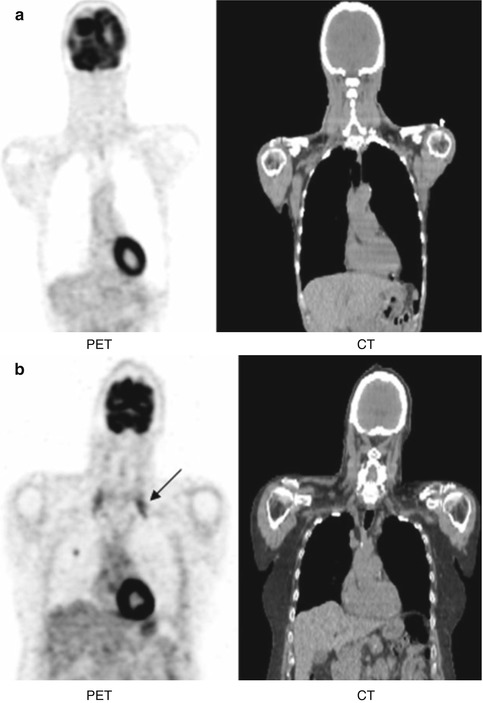
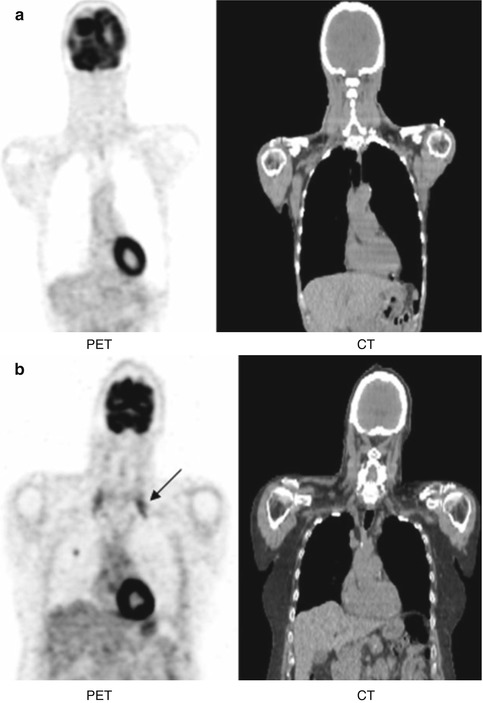
Fig. 12.4
(a) Patient with no COPD showing no uptake in scalene muscles. (b) Patient with COPD showing intense FDG uptake in scalene muscles bilaterally (arrow)
A common variant typically seen in colder months of the year is symmetric intense uptake in the bilateral neck which can extend to the supraclavicular, axilla, and paraspinal regions attributed to brown adipose tissue (BAT) (Fig. 12.5). These cells are characterized by multilocular lipid droplets and increased number of mitochondria, which express uncoupling protein 1 (UCP1). UCP1 is located in the inner membrane of the mitochondria and uncouples the rates of substrate oxidation and ATP production by favoring a loss of protons and thus energy release [54]. This uptake occurs due to heat generation in response to cold, ingestion of food, or increased sympathetic activity in anxious patients. There is abundance of BAT in infancy and slowly declines with age. Warming patients before injection as well as during the uptake phase has shown to be effective in decreasing this uptake [55].
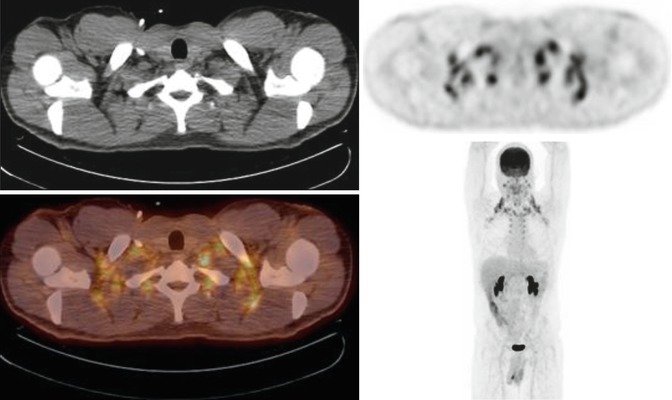
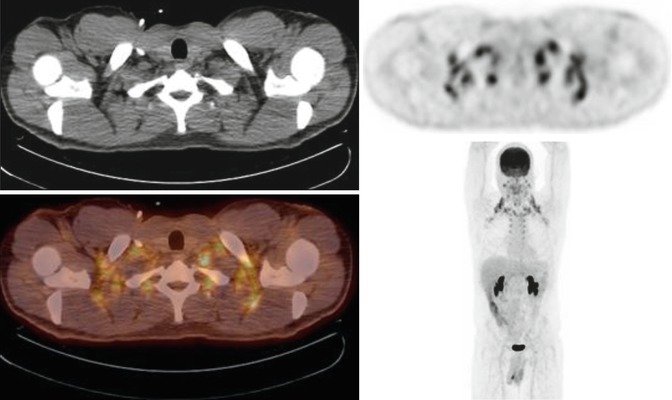
Fig. 12.5
A 34-year-old male with a history of colon cancer. PET/CT images demonstrate diffuse symmetric FDG uptake within the bilateral neck, supraclavicular, and axillary regions due to brown fat activity
Other variants such as normal thymic uptake in the anterior mediastinum can be seen in children and adults up to 30 years of age. In addition, uniform FDG distribution is commonly seen in circulation. However, when the normal blood flow is interrupted by a thrombus, a region of tracer void is seen on PET. In contrast, increased FDG uptake along a vessel wall is due to inflammation [56]. Normal thyroid tissue does not demonstrate significant FDG uptake. However, diffuse uptake can be seen in cases of thyroiditis and Graves’ disease. Focal uptake can be seen in benign nodules but carry a 33 % risk of malignancy [57]. Normal bone marrow uptake is commonly seen as similar intensity as the liver. FDG uptake is affected when a process alters marrow distribution. For example, hematopoietic stimulants such as colony stimulating growth factors will increase marrow uptake as will anemia or inflammatory processes [58]. On the other hand, radiation therapy will decrease uptake in the marrow. Compression deformities or fractures can cause intense uptake in the vertebra which can lead to misinterpretation as malignancy.
12.3.3 Uptake in Inflammation and Infection
18F-FDG uptake is not specific for only neoplasm. The agent also demonstrates activity in areas of active infection and inflammation. This can make it difficult to differentiate infections such as pneumonia from a malignant lesion. This can also cause misinterpretation in patients with sarcoidosis and granulomatous disease. A commonly encountered pattern of uptake is seen in lung cancer patients who have undergone radiation therapy. This causes intense FDG uptake initially in the lung parenchyma following the field used for therapy. This pattern of uptake may persist for many months and delaying the PET scan is recommended to allow for reduced inflammation (Fig. 12.6) [59]. FDG PET/CT also has a role in the evaluation of musculoskeletal infection demonstrating increased uptake in osteomyelitis as well as prosthetic joint loosening and infection [60].
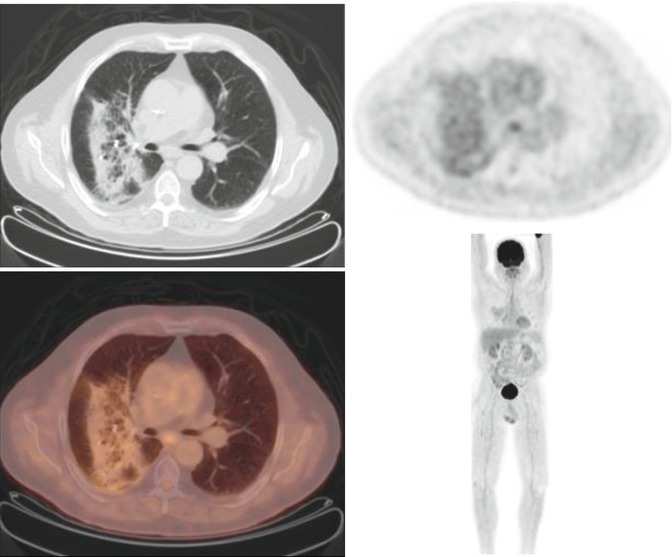
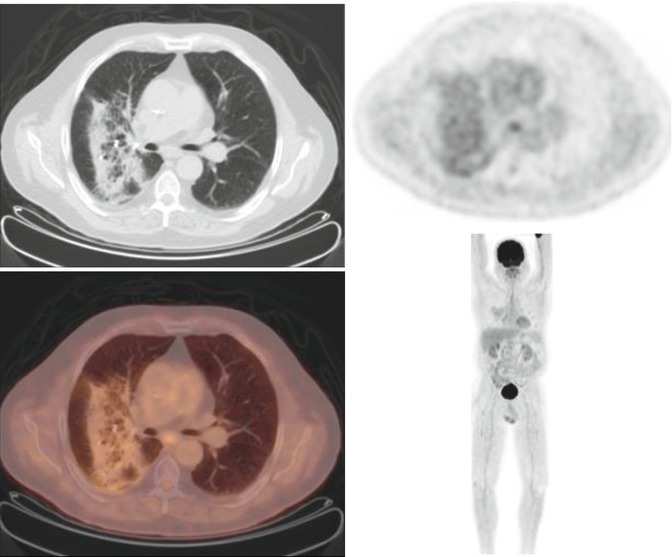
Fig. 12.6
A 68-year-old male with a history of right upper lobe adenocarcinoma. PET/CT images following cyber knife treatment showing fiducial markers at the site of a spiculated lesion surrounded by FGD avid postradiation changes
12.3.4 Artifacts
A commonly encountered pitfall of image interpretation is secondary to image acquisition and reconstruction algorithms causing artifacts. Dense objects such as metal from orthopedic hardware or iodinated contrast can produce areas of intense uptake on the attenuation-corrected PET images. Therefore, it is recommended to review the non-attenuation-corrected images for confirmation of these abnormalities. In addition, these can also cause beam hardening artifacts on CT. Respiratory motion artifact is also frequently encountered. This is due to the lung motion during normal breathing. PET/CT images are usually acquired during quiet respiration so the CT and images closely match PET. However, any deviation from this can cause abnormalities projecting in an incorrect location. This is commonly seen as a liver lesion which projects in the lung base (Fig. 12.7) [61].
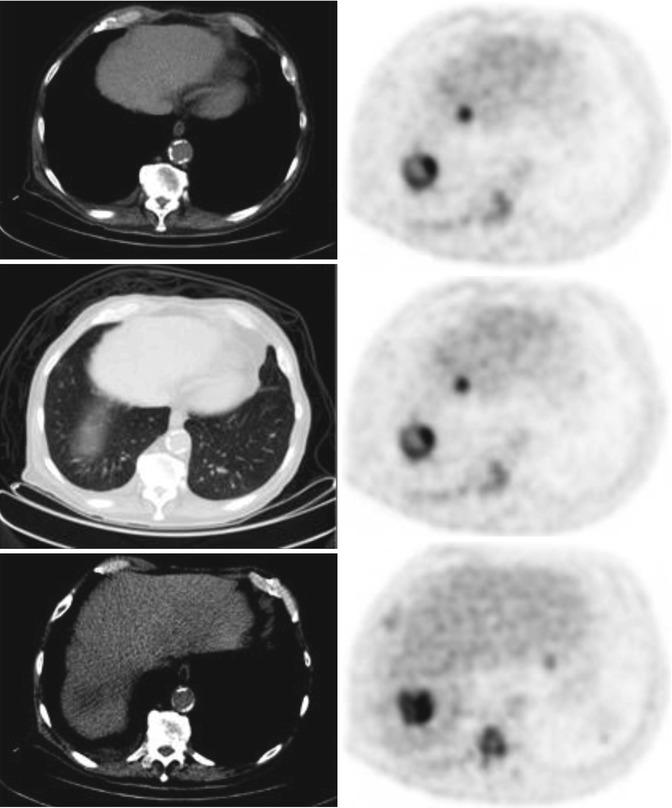
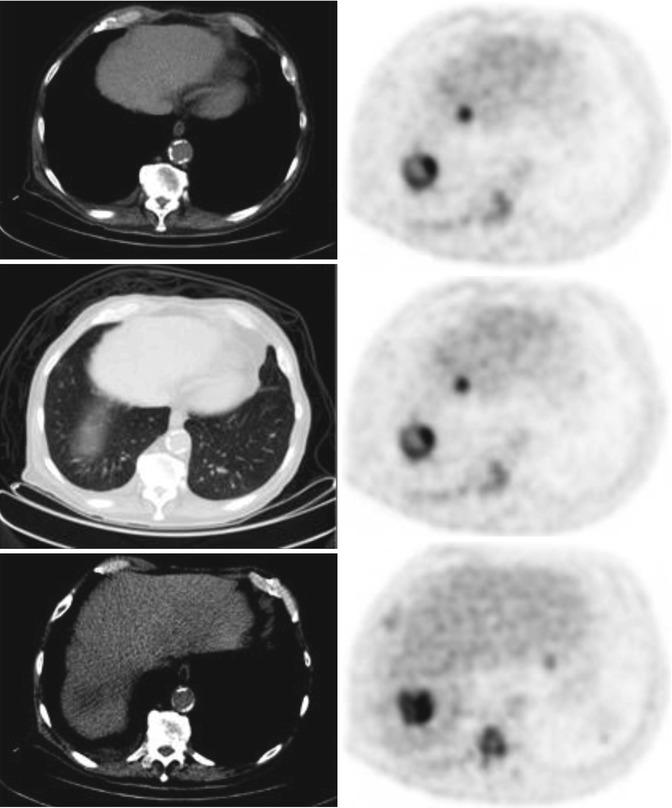
Fig. 12.7
A 71-year-old male with leukemia demonstrating respiratory motion artifact. Top row: Focal FDG uptake appearing in the lung base on PET image (right). Middle row: Lung window demonstrates no definite lung lesion. Bottom row: Hypodense lesion in the dome of the liver on CT matching the PET abnormality
12.3.5 Uptake Patterns of Malignancy
Interpretation of PET/CT imaging requires an understanding of normal and normal variant patterns of uptake. In addition, a familiarity of basic anatomy and physiology is needed to evaluate whether an area is normal or abnormal. In general, there is a higher degree of metabolism in tumors which is represented as increased FDG accumulation. However, low levels of uptake can be seen is certain malignancies such as bronchoalveolar carcinoma, carcinoid, prostate cancer, and mucinous adenocarcinoma. Areas of necrosis can demonstrate central photopenia on PET with a rim of increased uptake. Malignant pleural effusions can show variable uptake which is likely due to the dispersion of tumor cells in the effusion. Lesion activity is most commonly quantified as the standard uptake value (SUV). It is a measure of uptake in a specific region of interest and is corrected for body mass or body surface area.
12.4 Clinical Uses of PET/CT in Soft Tissue Malignancies
12.4.1 CNS Tumors
Brain metastasis is a common complication of cancer affecting 15–40 % of patients [62]. These patients have a poor prognosis even in the absence of systemic disease, with a median survival time ranging from 9 to 18 months [63]. The most common primary cancers that metastasize to the brain in adults are lung (40 %), breast, colon, renal cell carcinoma, and melanoma. In children, the most common are sarcoma and germ cell tumor. The cerebral cortex is the most common location for cerebral metastasis (80 %) with multiple lesions in two-thirds of the patients [64].
On the other hand, primary CNS tumors are much more rare with 7–19 cases per 100,000 [65]. According to the World Health Organization, there are three main types of gliomas: astrocytomas, oligodendrogliomas, and mixed oligoastrocytomas. Tumors are then graded I–IV based on the most malignant region within the tumor. Grades I and II are considered low grade and grades III and IV are considered high grade. Grading is based on the amount of mitosis, microvascular proliferation, nuclear atypia, and necrosis. There are three subtypes of low-grade gliomas, pilocytic astrocytoma (grade I), astrocytoma (grade II), and oligodendroglioma (grade II). High-grade gliomas include anaplastic tumors (grade III) and glioblastoma (grade IV). Glioblastoma is the most common glioma which also happens to be the most malignant. It accounts for 45–50 % of all gliomas [66].
The gold standard for brain imaging continues to be MRI which provides excellent anatomic details. FDG uptake within these tumors usually correlates with the grade of the tumor. Low-grade gliomas demonstrate lower metabolic activity than high-grade gliomas. In addition, high FDG uptake in a lesion that was a previously known low-grade tumor is suggestive of anaplastic transformation. Although MRI is the gold standard, there are limitations after treatment. In general, these tumors are surgically resected followed by radiation with or without chemotherapy. On follow-up imaging, MRI cannot clearly distinguish tumor recurrence from radiation necrosis. PET imaging has the upper hand in this situation. Tumor recurrence will show intense metabolic activity in the region of the lesion, whereas radiation necrosis will demonstrate reduced uptake or photopenia in the region (Fig. 12.8) [65].
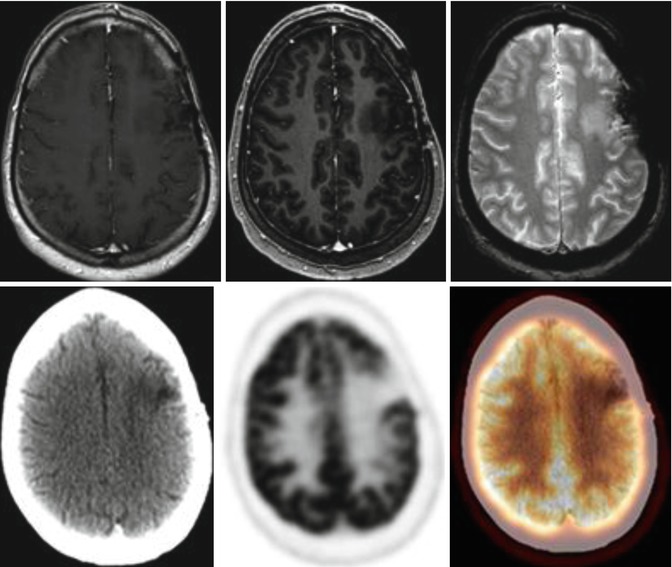
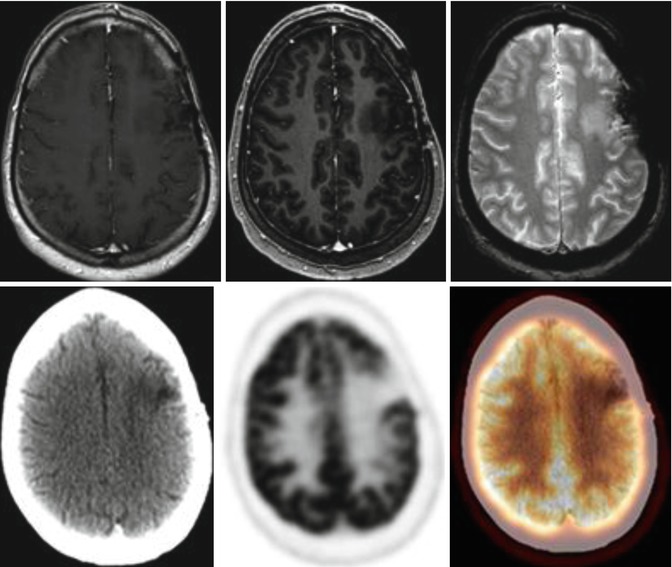
Fig. 12.8
A 41-year-old male with left frontal lobe mixed oligoastrocytoma, WHO grade 3, status post-resection and radiation therapy. Top row: Axial post contrast T1WI, STIR, and T2 WI showing slightly increased T2 hyperintensity adjacent to the superior medial aspect of the resection cavity in the left frontal lobe concerning for gliosis vs. tumor recurrence. Bottom row: FDG PET/CT images showing postoperative changes of left frontoparietal craniotomy with gliosis in the left frontal without evidence of focal FDG uptake in this region to represent tumor recurrence
A commonly seen phenomenon in brain imaging is reduced uptake in the cerebellar hemisphere contralateral to a supratentorial insult and referred to as crossed cerebellar diaschisis (Fig. 12.9). This manifestation is not only seen in tumors but in any supratentorial process including trauma, demyelination, gliosis, unilateral edema, and infarction [67]. This phenomenon occurs as a result of an interruption to the corticopontocerebellar pathway from the cerebral hemispheres to the contralateral cerebral cortex [68].
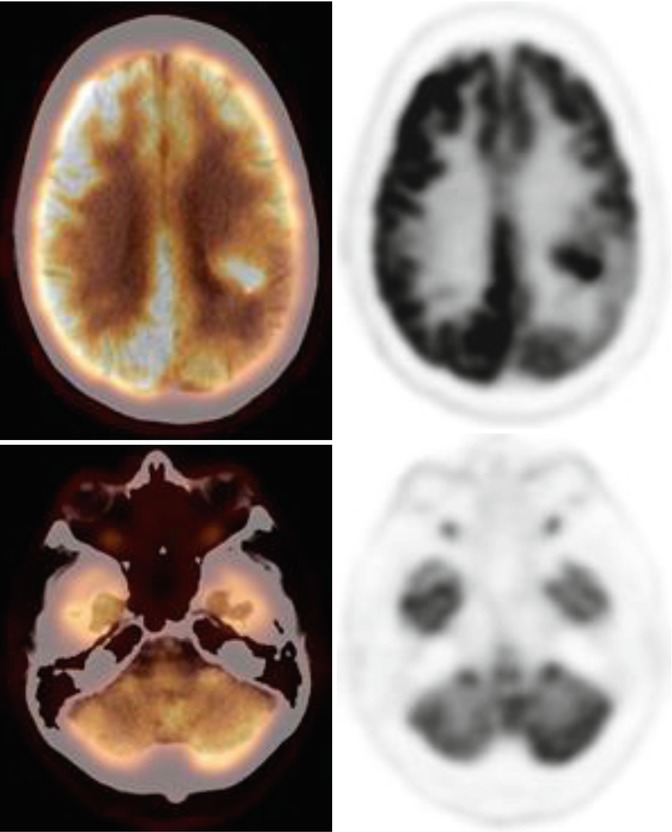
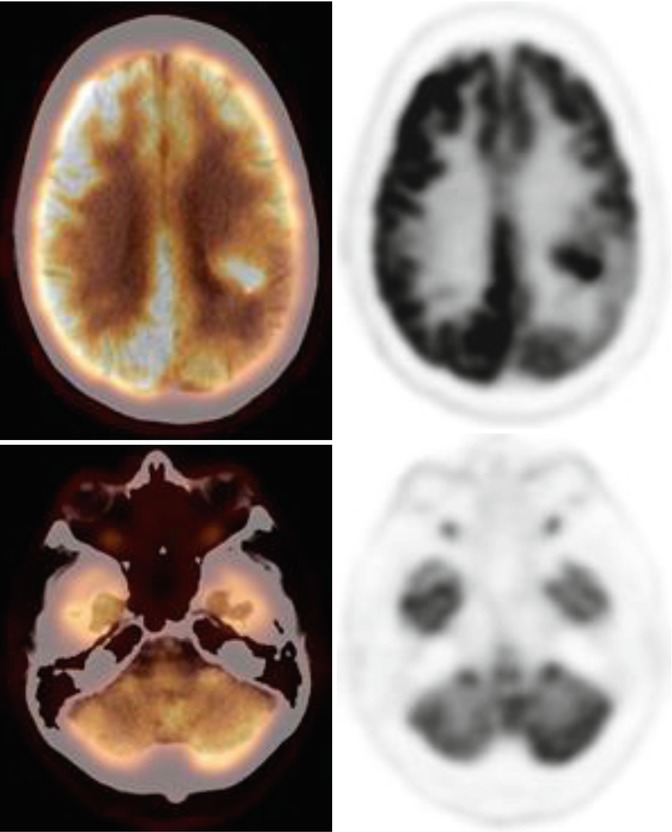
Fig. 12.9
A 61-year-old male with a history of biopsy-proven left temporal glioblastoma multiforme. PET/CT images demonstrate the left temporal lesion (top row). There is also decreased metabolic activity in the right cerebellum consistent with crossed cerebellar diaschisis (bottom row)
12.4.2 Head and Neck Tumors
Head and neck cancers account for up to 5 % of all cancers in the United States. Of these, the majority of cases are due to squamous cell carcinomas of the oral cavity, nasopharynx, oropharynx, and larynx. The overall annual mortality rate in the United States is 23 % with a 5-year survival rate of 56 % [42, 69]. Lymph node involvement is crucial in assessing if a patient should undergo surgical resection. The location, number, and size are all important considerations for treatment planning. It has been reported that nearly 40 % of patients have localized disease, while the remaining 60 % have advanced disease. FDG PET has been found to be equivalent if not superior to CT and MRI for the detection of nodal disease. PET has the upper hand when evaluating nodes which are normal in size by CT and MRI criteria. These tumors are often treated with surgical resection and/or radiations. PET/CT is particularly helpful in assessing for tumor recurrence in the postoperative patient. Due to the loss of symmetry and distortion of the normal anatomy, evaluation of post-therapeutic changes from recurrent or residual disease can be challenging (Fig. 12.10). False-positive findings can occur secondary to recent surgery or radiation therapy. In addition, laryngeal muscle activity, patterns of increased muscle uptake, and reactive lymph nodes can also lead to misinterpretation. However, PET has been found to have a sensitivity for diagnosing recurrence up to 100 % with a specificity of 85 % [70].
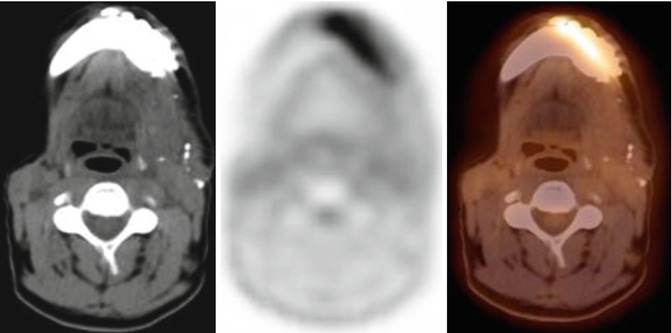
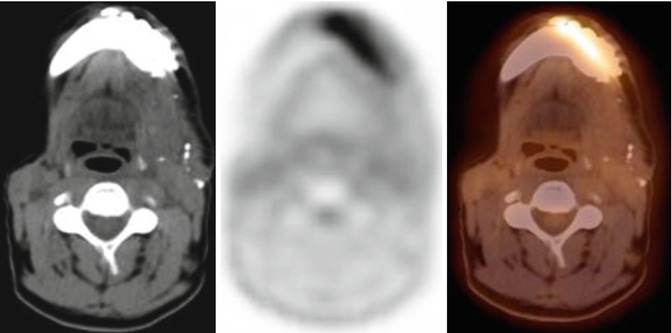
Fig. 12.10
A 49-year-old male with a history of squamous cell carcinoma of the floor of the mouth and alveolar ridge, status post left marginal mandibulectomy and bilateral supraomohyoid neck dissection. PET/CT images show multiple surgical clips at the operative bed with distorted anatomy of the floor of the mouth. There is no evidence of focal activity to suggest tumor recurrence
12.4.3 Thyroid Cancer
Radioiodine imaging with I-131 has been the mainstay for the evaluation of thyroid cancer. The follicular cells within the thyroid gland are responsible for neoplasm and gives rise to papillary, follicular, or mixed cell variants and are commonly well differentiated. These tumors are iodine avid and diagnosed and treated with I-123 or I-131. FDG does not accumulate in these cell types and is therefore not indicated for the diagnosis of thyroid cancer. However, tumor recurrence is not always iodine avid which is secondary to tumor dedifferentiation. When tumors have lost the ability to synthesize hormones from iodine, they have increased glucose metabolism [71]. These patients present with elevated human thyroglobulin levels with negative I-131 scans. In these patients with a high clinical suspicion for disease but negative I-131 scan, FDG PET/CT can aid in the detection of metastatic disease (Fig. 12.11). In addition to poorly differentiated tumors, FDG has also been found to be useful for medullary thyroid carcinoma. This is a relatively rare disease which arises from the parafollicular cells and does not accumulate I-131. It accounts for 3–10 % of all malignant thyroid tumors [72]. This type of cancer typically demonstrates intense FDG avidity making PET/CT essential for proper staging and follow-up with a sensitivity of 76–78 % and specificity of 79 % [71].
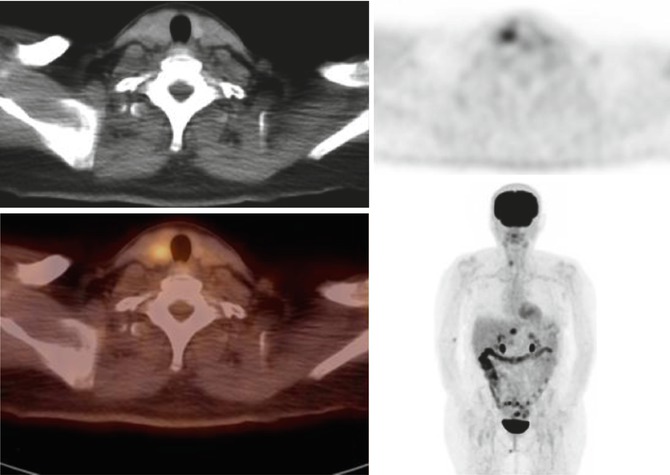
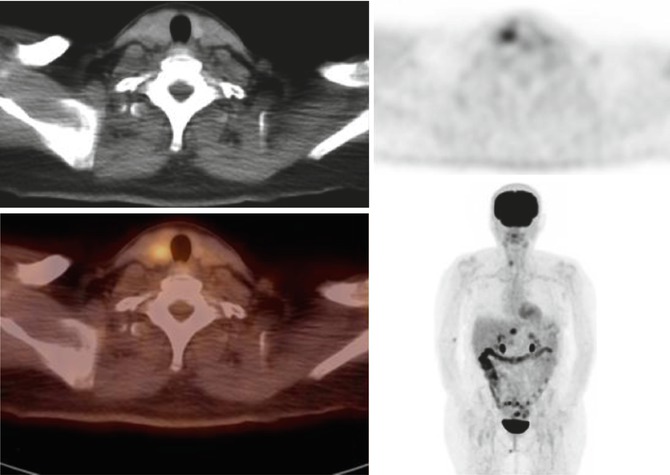
Fig. 12.11
A 56-year-old female with a history of esophageal cancer. PET/CT images demonstrate an FDG avid focus in the right lobe of the thyroid gland. Biopsy of the focus was positive for malignancy
12.4.4 Esophageal Cancer
The esophagus is a hollow muscular tube that connects the pharynx to the stomach. The mucosal lining of the esophagus is primarily comprised of stratified squamous epithelium. Malignancy in this area is commonly due to squamous cell carcinoma, accounting for 85 % of cases. The distal portion is comprised of columnar epithelium. Adenocarcinoma is commonly encountered in this area. Patients will often present with dysphagia or by endoscopic biopsy in patients with Barrett’s esophagus, considered a premalignant condition which predisposes patients to the development of adenocarcinoma. Barrett’s esophagus has been shown to increase the risk of developing adenocarcinoma by 30-fold when compared to the general population [73].
The normal metabolic activity in the esophagus is typically low, resembling background. Both squamous cell carcinoma and adenocarcinoma are FDG avid, and any focal areas of uptake within the esophagus should raise a suspicion for malignancy. However, focal FDG uptake can also be seen in many benign processes such as esophagitis, postprocedural inflammation, postradiation inflammation, hiatal hernia, and Barrett’s esophagus (Fig. 12.12).
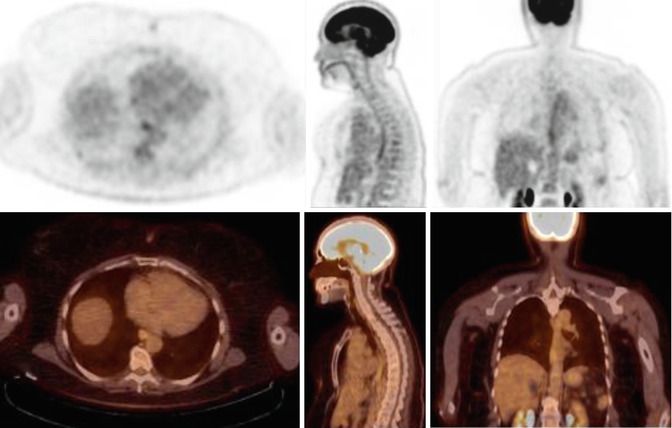
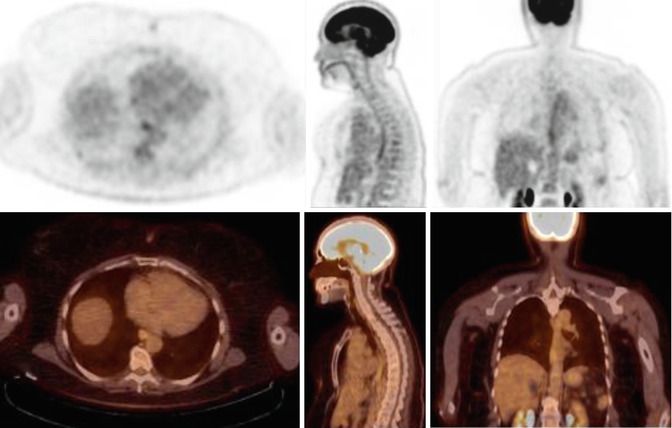
Fig. 12.12
A 63-year-old female with a history of meningioma. FDG PET/CT images show mild liner activity along the mid- and distal esophagus related to esophagitis from gastroesophageal reflux disease
The most important indicators for prognosis are depth of tumor penetration and nodal involvement. The 5-year survival rate for patients without nodal involvement is 40 % but then decreases to 3 % when nodal disease is present [73]. Locoregional nodal metastasis is most common, but the location of nodes often depends on the level of the primary tumor. Cervical nodes are often found with more proximal esophageal lesions, and abdominal nodes are often associated with more distal lesions (Fig. 12.13). FDG PET/CT has been found to be more sensitive than CT alone for diagnosing nodal metastasis is esophageal cancer [74]. In addition, PET/CT has also been found to affect patient staging in up to 40 % and change management in up to 34 % of cases [75].
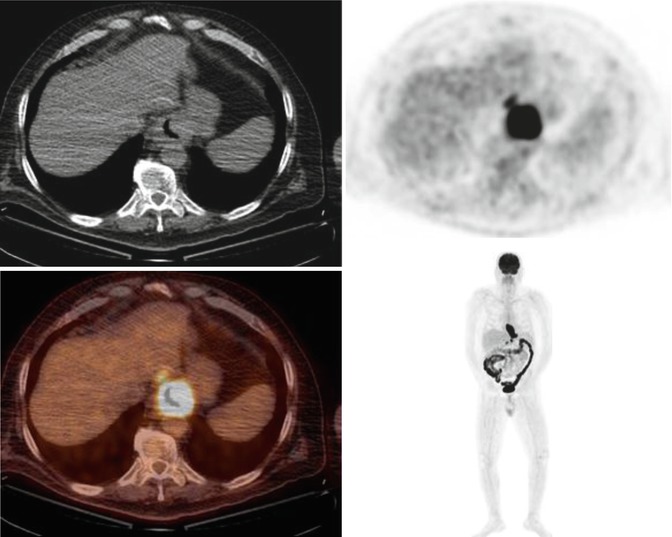
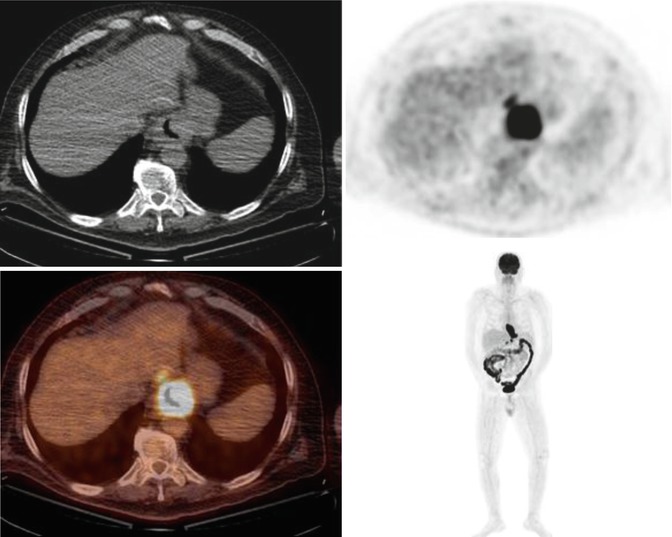
Fig. 12.13
A 69-year-old male complaining of dysphagia, odynophagia especially after solid food, and weigh loss of 35 lb over 6 months. FDG PET/CT shows an FGD avid mass in the distal esophagus extending into the gastric fundus with FDG avid metastatic gastrohepatic, perigastric, and precaval/peripancreatic lymph nodes. Biopsy revealed moderately differentiated adenocarcinoma of the gastroesophageal junction
12.4.5 Breast Cancer
Breast cancers are predominantly screened with mammography and breast ultrasound. Mammography is highly sensitive and can identify 80–90 % of patients with breast cancer. However, a positive mammogram does not always lead to malignancy. Based on histologic analysis, only between 20 and 40 % of patients with abnormal mammograms are found to have breast cancer. In addition, about 10 % of breast cancers cannot be identified on mammograms even when palpable [76]. The most common type of breast cancer is invasive ductal carcinoma consisting of 70–80 % of cases. Invasive lobular carcinoma is relatively uncommon and consists of 5–10 % of cases [77]. Although FDG PET/CT is primarily used in the evaluation of restaging, recurrence, and response to therapy, it is also useful in the evaluation of non-palpable masses in dense breast as well as when mammography is equivocal.
A major benefit of PET is that it is not affected as other modalities by dense breast tissue, prior surgery, breast augmentation, or radiation therapy. It has the ability to not only identify primary tumors but also locoregional nodes and distant metastasis (Fig. 12.14). The ability of PET/CT to localize primary lesions is related to tumor size. For lesions less than 1 cm, PET has a sensitivity of 25 %, but for lesions 1–2 cm, the sensitivity can be as high as 84 % [78]. In general, the amount of metabolic activity within a tumor correlates with tumor grade as well as proliferation index (Ki67 expression). In addition, there is higher uptake in infiltrating ductal carcinoma than in infiltrating lobular carcinoma. This may be secondary to its infiltrative properties as well as low tumor cell density [79].
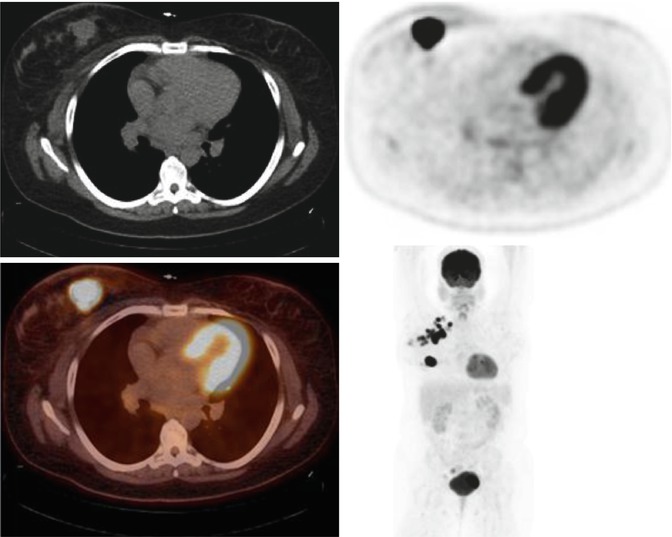
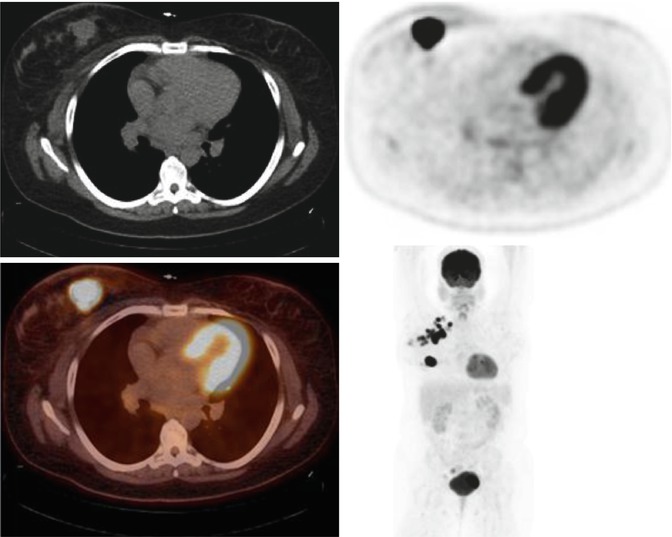
Fig. 12.14
A 34-year-old female presenting with a right breast mass. FDG PET/CT images show an intensely hypermetabolic right breast mass with multiple hypermetabolic right axillary lymph nodes. Biopsy revealed right breast invasive ductal carcinoma with metastatic right axially lymph nodes
Lymph node involvement is the most important variable in staging and essential in the proper therapeutic approach. The gold standard in the evaluation of axillary lymph nodes continues to be lymphoscintigraphy with 99mTc sulfur colloid. FDG PET/CT is helpful in evaluating metastasis in lymph nodes that would otherwise be normal by CT criterion. However, it has been reported that the sensitivity of detecting axillary lymph node metastasis with PET/CT rages from 44 to 67 % with a specificity of 90–99 %. False-negative results tend to occur in patients with small deposits of tumor in subcentimeter nodes. Nonetheless, in a noninfectious setting, increased metabolic activity in an axillary lymph node is suspicious for malignancy with a positive predictive value of up to 80 % [79].
12.4.6 Renal and Bladder Cancers
Both renal and bladder cancers are difficult to evaluate with PET/CT primarily due to the variability of FDG uptake in both entities as well as the intense urinary excretion of 18F-FDG within these structures (Fig. 12.15). Renal cell carcinoma account for approximately 3.5 % of all malignancies and is the most lethal. The sensitivity of PET/CT in renal cell carcinoma ranges from 31 to 94 % [80]. Therefore, PET/CT tends to have a complimentary role in the diagnosis of renal cell carcinoma. It is, however, superior to conventional imaging for detecting recurrence and metastasis. Bladder cancers too tend to follow the same pattern. Diagnosis is based on cystoscopy and biopsy with transitional cell carcinoma accounting for more than 90 % of all bladder cancers. PET/CT has a limited role in this setting, but it has been noted that the use of various techniques such as delayed imaging, fluid loading, diuresis, and bladder catheterization can help with disease detection [81].
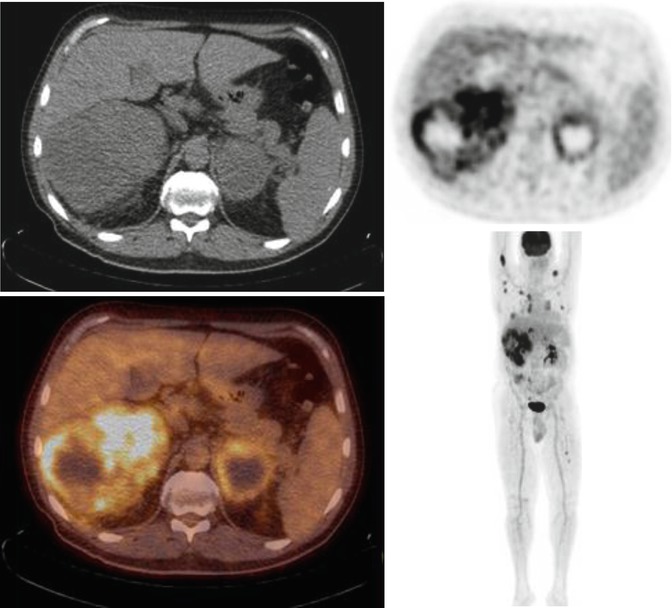
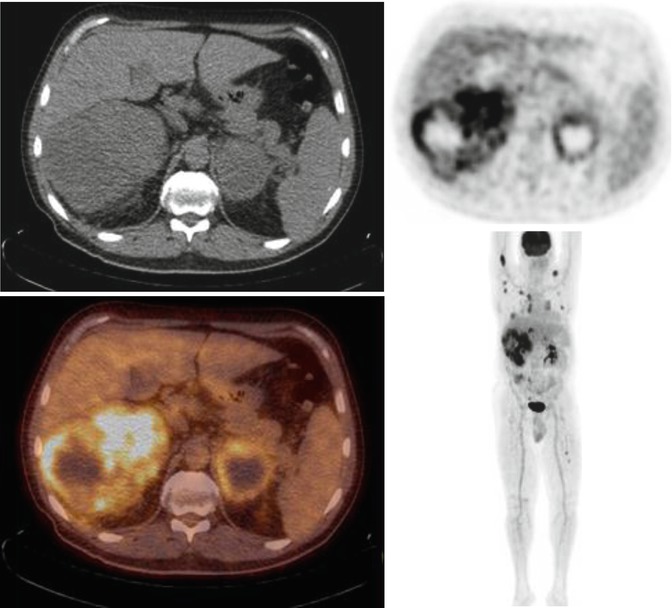
Fig. 12.15
A 54-year-old male with incidentally discovered enlarged mediastinal lymph nodes on a CT angiography of the neck/done for a bleeding cavernoma of the brain. FDG PET/CT images show a large FDG avid right renal cell carcinoma with widespread metastasis to the lungs, mediastinal lymph nodes, left adrenal gland, and multiple bones
12.4.7 Gynecologic Cancers
Cervical cancer is the most common gynecologic cancer and the second most common cancer in women [82]. It is commonly treated with surgery, but chemotherapy and radiation can be required for advanced disease. Although FDG PET/CT has limited value of staging primary tumors due to the variable uptake in nearby structures (bowel and urinary tract), it does have a role in detecting lymph node metastasis [83]. It has been shown that FDG PET can detect lymph node metastasis in these patients with a sensitivity of 91 % and specificity of 100 %. On the other hand, MRI had a sensitivity of 73 % and specificity of 83 % [84].
Ovarian carcinoma is the second most common gynecologic cancer and the leading cause of death in women with gynecologic malignancies [85]. Again, FDG PET/CT has limited value of staging primary tumors due to the nearby structures, but to further complicate matters, physiologic conditions such as ovulation and menstruation can also lead to false-positives. Many other false-positives have been reported and are due to inflammatory adnexal masses, endometriomas, corpus luteum cysts, and other benign ovarian tumors. FDG PET/CT is often used for restaging and detecting metastatic disease in conjunction with serum markers (Ca-125, Ca 19-9, alpha-fetoprotein, and human chorionic gonadotropin). The sensitivity of FDG PET has been reported to be 58 % with a specificity of 76 % [86].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree