George M. Bridgeforth, David S. Wellman, and Charles Carroll IV
AN 80-year-old woman lost consciousness and fell down the stairs. She sustains multiple injuries as a result.
CLINICAL POINTS
- The majority of these fractures are isolated injuries.
- Either direct or indirect trauma may cause olecranon fractures.
- Olecranon bursitis may develop.
- During the physical examination, the clinician should
- evaluate range of motion.
- check for skin integrity and swelling (bursitis) around the joint.
- perform a complete neurovascular examination focusing on the following nerves:
- Median (opponens pollicis weakness with diminished grip strength associated with impaired sensation of the thenar eminence)
- Ulnar (decreased sensation and weakness of the ulnar wrist flexors, hypothenar eminence, fourth and fifth fingers)
- Radial (acute wrist drop or wrist extensor weakness with impaired sensation over the dorsal wrist and forearm)
- Median (opponens pollicis weakness with diminished grip strength associated with impaired sensation of the thenar eminence)
- check for neurovascular compromise or compartment syndromes (swollen painful cyanotic limb with numbness and diminished or absent pulses), and document findings prior to treatment.
- check the wrist and shoulder for associated injuries.
Clinical Presentation
Olecranon fractures account for approximately 20% of all elbow fractures. These fractures are caused by direct or indirect forces. Direct force fractures tend to occur secondary to falls onto the elbow. Indirect force injuries are caused by forceful contraction of the triceps and are often simple transverse or oblique fractures. Olecranon fractures are characterized by acute swelling, pain, and tenderness. Patients usually exhibit painful range of motion as well. Following acute trauma, several conditions, including olecranon bursitis and pseudofractures can mimic the picture seen with olecranon fractures.
OLECRANON BURSITIS AND OLECRANON PSEUDOFRACTURES
Olecranon bursitis is a condition that can present simultaneously or independently of an olecranon fracture. It can be grossly categorized into septic and nonseptic presentations.
A septic bursitis is characterized by warm, tender, painful swelling of the olecranon. Immediate evaluation with aspiration, gram staining, culture, and cell counts/fluid analysis is necessary. Most penetrating infections are caused by gram-positive organisms such as Staphylococcus aureus, Staphylococcus epidermidis, and Streptococcus. Initial treatment consists of aspiration and antibiotics. Repeat aspirations may be necessary if fluid reaccumulates. The clinician should consider formal incision and drainage if a trial of aspiration and antibiotics fails, as the infection could spread into the elbow joint. Care must be taken, as rheumatiod arthritis and gout can produce a similar picture and masquerade as a bacterial infection.
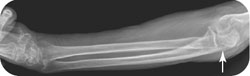
A traumatic or idiopathic (nonseptic) olecranon bursitis is a golf ball–like swelling over the olecranon (Fig. 35.1). Chronic changes may result in a thickening of the overlying skin with a peau d’orange (orange peel) appearance. Treatment consists of aspiration, fluid culture, and analysis (to rule out septic bursitis and evaluate for crystals). The clinician should consider starting a nonsteroidal anti-inflammatory drug and giving a steroid injection, because researchers have hypothesized that both hasten recovery. It is sometimes necessary to perform a surgical bursectomy in refractory cases.
Patients with elbow spurs (syndesmophytes) at the olecranon may present with a pseudofracture of the olecranon and chronic (nonseptic) bursitis. Pseudofractures appear as a small translucent line in the syndesmophyte. Generally, these lines do not extend into the cortical margin of the olecranon. Pseudofractures commonly appear in syndesmophytes because of the poor quality of the porous bone in elbow spurs. Generally, they do not require any treatment, and management of the bursitis can proceed as described above.

FIGURE 35.1 (A) Lateral radiograph of the left elbow in an 80-year-old man with 1 month of left elbow pain and swelling, which demonstrates a prominent olecranon spur at the insertion site of the triceps tendon (arrow) with soft tissue swelling posteriorly (arrowheads), suggesting olecranon bursitis. (B) A selected sagittal fluid-sensitive image of the left elbow in the same patient confirms abnormal fluid posterior to the olecranon (outline) compatible with olecranon bursitis. Fluid analysis should be performed to exclude an infectious etiology.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








