Drawing 15.1
(a) Anatomy of the pancreatic gland, (b) anatomy of the pancreatic duct
In adults, the pancreas weighs approximately 100 g and is about 17–20 cm long, it has a soft texture and friable.
The main pancreatic duct of Wirsung (3–4 mm) traverses the entire length of the gland and pours the pancreatic secretion into the duodenum. The caliber of the duct decreases homogeneously from head to tail. The duct receives 25–35 side branches; at the level of the papilla it merges with the choledocus into the Vater ampulla (Drawing 15.1b). There is a secondary duct named Santorini; it is the embryonic vestige of the primitive pancreas and as such may not be working. If it is anatomically functional, it drains the back of the pancreas head. It opens in the duodenum about 2–3 cm above the main duct, in the papilla called “minor” that does not have sphincter, and for this reason, if the ostium is stenotic, it is related to pancreatitis.
Pancreatic vascular supply is owing to the superior pancreaticoduodenal artery from the gastroduodenal artery and the inferior pancreaticoduodenal artery from the superior mesenteric artery which supplies the head of the pancreas.
The pancreatic branches of the splenic artery (the largest is called the greater pancreatic artery) supply the neck, body, and tail of the pancreas.
The head of the pancreas drains into the superior mesenteric and portal veins; the neck and the body drains into the splenic vein [2].
15.2 Etiopathogenesis
Pancreatic trauma, due to its retroperitoneal position, is relatively rare especially as an isolated lesion; it is still more frequent in children [3].
Pancreatic traumatic injuries have a mortality rate that can reach 39%, occur in 0.4% of total blunt abdominal trauma with an incidence of 7% (range 2–13%) in major trauma, such as in motor vehicle accidents, pedestrian accidents, or bicycle accidents especially in children “handlebar” trauma [4]. We must not forget that the pancreas for its “central position” is an organ particularly affected in child abuse cases; the injuries of this organ are responsible for about 1/3 of post-traumatic pancreatitis in pediatric age [5].
Nowadays we must take into consideration not only the blunt trauma but also the penetrating trauma as gunshot wounds and blade injuries that is rising in incidence and accounts for 70% of all traumatic pancreas injuries.
With regard to the zone of lesion, body and isthmus are affected in 2/3 of the cases generally for front force vectors (e.g., trauma caused by the steering wheel of the car in the absence of seat belt). The head and tail of the pancreas are involved in 1/3 of the cases generally for lateral force vectors.
Pancreatic lesions are often (in over 90% of cases) associated with other abdominal organ injuries, especially associated with the viscera situated in the upper abdomen [6]. Bone injuries are also often associated.
The absence of specific clinical symptoms and the frequent presence of multiple organ injuries make it difficult to develop a diagnosis. This injury is associated with considerably high morbidity and mortality in cases of delayed diagnosis, incorrect classification of the injury, or delays in treatment.
It’s important to notice that in children you may have pancreatic damage even in small claims traumas, due to the lower strength of the abdominal wall [7].
15.3 Clinical Presentation
Ecchymosis in either the upper abdomen or along the flank may be present in cases of pancreatic injury. In the child, in the bicycle handlebars trauma often there is a round bruise in mesogastric region.
The rise in the serum of amylase and lipase is present respectively in 73% and 82% of cases.
The classical clinical triad of pancreatic trauma is upper abdominal pain, leukocytosis, and elevated serum amylase level, that may, however, be absent in the first 24 h (in up to 40% of patients) or even after several days although it does not always indicate the severity of the injury [8].
Amylase may be elevated even in injuries of duodenum, salivary gland, hepatic trauma, and injuries of head and face [1].
The lack of clinical manifestations makes it difficult to diagnose, and delay in diagnosis is the main cause of complications, therefore it is necessary to have a second level radiological diagnosis.
15.4 Classification
Traumatic lesion could interest any site of the pancreas; those that are localized to the head and body (90%) are most frequent and are connected to the compression of the pancreas against lumbar spine.
The most recent grading system for pancreatic injuries was outlined by the American Association for Surgery in Trauma (AAST) [9].
It takes into account both the type of parenchymal damage and the site of the parenchymal gland in which the damage has occurred, the involvement of the duct of Wirsung, that usually occurs in 15% of cases, or of the ampulla.
The classification is divided into five degrees in relation to the severity of the damage.
In the grade I: there is a minor contusion/hematoma or superficial laceration without ductal injury (Drawing 15.2a, b); sometimes the minor contusion of the gland may be difficult to see especially in a patient with multiple organ lesions. The gland can be enlarged with ill-defined profiles also due to the surrounding fluid often present (see Fig. 15.6).


Drawing 15.2
I grade pancreatic lesion (a) minor contusion, (b) superficial laceration. Note in both cases the integrity of the pancreatic duct
In the grade II: there is a major contusion/laceration; the lesion is largest than in the first degree but the duct is always intact (Drawing 15.3a, b).


Drawing 15.3
II grade pancreatic lesion. (a) Major contusion, (b) major laceration. Note in both cases the integrity of the pancreatic duct
In the grade III: there is a laceration or parenchymal injury with duct injury in distal pancreas (Drawing 15.4a, b).


Drawing 15.4
III grade pancreatic lesion. (a) Distal laceration (b) distal parenchymal injury. In both cases there is a distal duct injury
In the grade IV: there is a proximal (right of superior mesenteric vein ) laceration or parenchymal injury with associated injury to bile duct /ampulla (Drawing 15.5a, b).


Drawing 15.5
IV grade pancreatic lesion. (a) Proximal laceration, (b) proximal parenchymal injury. In both cases there is a proximal duct injury
In the grade V: there is a massive destruction of pancreatic head (Drawing 15.6).


Drawing 15.6
V grade pancreatic lesion. There is a massive destruction of pancreatic head
Based on the severity and extent of the lesions that we can find at CT exam:






Pancreatic contusion: interstitial edema with focal or diffuse enlargement of the gland (Figs. 15.1 and 15.2).
Pancreatic hematoma: blood collection often intraglandular (Fig. 15.3).
Pancreatic laceration: partial thickness tear of the pancreas, frequently with vertical axis [10] (Fig. 15.4).
Pancreatic transection: full thickness tear of the pancreas (Fig. 15.5).
Intra- or extraglandular active bleeding (Fig. 15.6).

Fig. 15.1
Enhanced CT scan shows pancreatic head contusion as a focal enlarged area with hypodense aspect due to interstitial edema (white arrows)

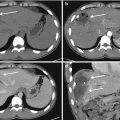
Fig. 15.2
CE-MDCT scans (a, b) show a fracture of the upper pole of the spleen associated with pancreatic body and tail contusion (arrows)

Fig. 15.3
Enhanced CT scan shows pancreatic hematoma: diffuse enlargement inhomogeneous hypodense aspect and irregular borders, in the head there is a focal rounded hypodense area with thin border. Hepatic lesion and free fluid are associated

Fig. 15.4
Pancreatic laceration: (a) axial CT scan and (b) coronal reconstruction show partial thickness tear of the body (arrow); there is a fluid collection behind and below the pancreatic body (arrowheads)

Fig. 15.5
Unenhanced CT (a) and enhanced CT scan in arterial (b) and portal (c) phases show a case of pancreatic body transection. In unenhanced CT (a) there is an inhomogeneous aspect of the pancreas body; CE-CT scans (b, c) well detect the complete transection of the body as a hypodense linear image

Fig. 15.6
Enhanced CT exam shows a case of pancreatic active bleeding (white arrows) complex trauma treated with splenectomy and packing
Pancreas head injuries are more severe than those in the body and tail. Pancreatic injury is uncommonly (<10%) an isolated lesion; other organs are frequently involved like: duodenum (involved in 60%), liver (46%), stomach (42%), spleen, kidney, mayor vascular: aorta, inferior cava vein, splenic artery and vein (41%), spine fractures (28–30%), stomach, and other tract of the bowel [11]. The involvement of mayor vessels is responsible for premature mortality for massive bleeding; the bowel involvement increases long-term mortality and late complications for septic state due to perforation and peritonitis. In case of pancreatic lesion, the dehiscence of intestinal anastomosis increases.
15.5 CT Imaging
Computed tomography (CT) is the imaging modality of choice in the study of hemodynamically stable polytrauma patient, detecting all grades of pancreatic lesions in 80% [8, 12]. The CT is also able to evaluate most of the prognostic indicators that can change the management of the patient and it is fundamental to follow complications which occur very often.
The pancreas can appear normal in 20–40% of patients in the first 12 h after trauma because pancreatic injuries may produce nuanced hyperdensity which may not be detectable [13].
The CT is not always able to view the pancreatic duct injury but its tear can be suspected in cases of parenchymal injury larger than 50% of the diameter of the pancreas and MPR reconstruction is fundamental in detecting injury. However, it often happens that the ductal lesions are discovered in the operating room. If ductal injury is suspected and the clinical condition of the patient allows further studies, the evaluation of pancreatic duct should be carried out with magnetic resonance (MRI) or endoscopic retrograde cholangio-pancreaticography (ERCP) [14].
15.5.1 CT Protocol
The CT scan is performed with MDCT scanner. The exams are obtained in cranio-caudal direction, in cases of polytrauma patients from “head to toe,” and in cases of localized minor trauma the evaluation can be limited to the abdomen.
CT examination includes unenhanced scans, followed by enhanced CT scans, in arterial and portal phases. Arterial phase is performed with bolus tracking (with a ROI located in abdominal aorta below the diaphragm) or with a delay of 30–40 s from the beginning of contrast administration; portal phase is usually performed with a delay of 70–80 s.
The quantity of a nonionic low-osmolar iodinated contrast depends on the patient’s weight and on the acquisition speed time of the machine; generally, the quantity is around 120–140 mL injected at a rate of 3–4 mL/s.
A thin collimation is necessary, MPR reconstruction on coronal plane is fundamental to assess the lesion of the duct, even 3D reconstructions can be of help.
The CT findings of acute pancreatic trauma may be separated into specific (direct) features and nonspecific (indirect) features [15].
Direct CT signs of pancreatic trauma include evidence of parenchymal contusion, hematoma, laceration, and transection [4, 16].
15.5.1.1 Pancreatic Contusion
Unenhanced CT scan: Contusion cannot be detectable; however, it is possible to find focal or diffuse pancreatic enlargement in case of intraparenchymal edema.
Enhanced CT scan: Small contusion can be difficult to detect; in some cases, it appears as focal or diffuse low attenuation area inside the parenchymal gland without discontinuity at the surface of the gland; the margins of the gland appear irregular, and fluid collection may surround the gland (Fig. 15.7).


Fig. 15.7
CE-MDCT in a case of pancreatic head and body contusion; note the difference between the hazy irregular contours of the head and part of the body (arrows) compared with the rest of the gland. There is also a small fluid collection surrounding pancreatic head and located along the right anterior renal fascia in the retroperitoneal space (arrowhead)
15.5.1.2 Pancreatic Hematoma
Unenhanced CT scan: Blood content determines focal hyperdensity that tends to become isodense in later hours.
Enhanced CT scans: Hematoma can be a very specific sign of pancreatic injury and manifests as an area of focal attenuation within the pancreatic parenchyma. It is often peripherally located and distorts the gland profile (Fig. 15.8).


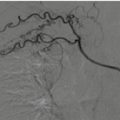
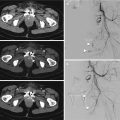
Fig. 15.8
Contrast-enhanced MDCT (a, b) shows hematoma of the pancreatic body in a polytrauma patient, already undergoing splenectomy. It is possible to detect focal attenuation within the pancreatic tail parenchyma; the tail is enlarged. In arterial phase (a) note active bleeding coming from a branch of the left hypogastric artery (white arrows). (c) Selective arteriography shows the active bleeding (arrow), treated by selective embolization with microcoils and spongostan (d, e)
15.5.1.3 Laceration
Unenhanced CT scan: Lacerations manifest as linear, irregular, low attenuation areas within the pancreatic parenchyma. The laceration is often perpendicular to the long axis of the pancreas. It is often difficult to see in basal conditions and can manifest only as an area of glandular inhomogeneity.
Enhanced CT scans: Lacerations are hypodense but more defined with a linear or irregular aspect. The line, ideally, represents the separation of fragments with fluid or blood within the fragments. This can be classified into superficial laceration (involving <50% of the parenchyma) and deep laceration (>50% pancreatic parenchyma) [4]. It’s possible to collect fluid effusion in retroperitoneal space.
In case of laceration, the pancreatic duct may be intact or damaged, depending on the extension of the laceration; sometimes the presence of a deep laceration leads to the suspicion of ductal lesion. In doubtful cases, it is recommended to complete the study as soon as possible with magnetic resonance cholangiopancreatography (MRCP) (Fig. 15.9).


Fig. 15.9
CE-MDCT. Pancreatic body laceration appears as linear, irregular line within pancreatic body (arrowhead); note also the enlargement of pancreatic tail expression of contusion (arrows)
15.5.1.4 Transection/Fracture
Unenhanced CT scan: Pancreatic transection/fracture was defined as a low-attenuating band extending throughout the thickness of the gland with fluid collection between the two separated fragments. Usually occurs vertical transection of the pancreatic body or head.
Enhanced CT scans: The CT aspects of transection previously described have better evidence in CE-MDCT; furthermore active hemorrhage from the pancreatic parenchyma can be seen as contrast extravasation with hyperdense spots.
In case of transection or fracture of the pancreatic gland, the main duct is always involved; this eventuality determines a change in the management of the patient (Fig. 15.10).