, Gustav Andreisek2 and Erika J. Ulbrich2
(1)
Phoenix Diagnostic Clinic, Cluj-Napoca, Romania
(2)
Institute of Diagnostic and Interventional Radiology, University Hospital Zürich, Zürich, Switzerland
7.1 Anatomy and Normal MRI Appearance
7.1.1 Patella and Patellar Retinaculum
The patella is the largest sesamoid bone in the body and is part of the extensor mechanism of the knee together with the quadriceps muscle and tendon, patellar tendon, and patellar retinaculum [1]. The bone has two surfaces, three borders, a base, and an apex. The vastus intermedius and the rectus femoris tendons attach to the base (syn. proximal pole) of the patella and the vastus medialis and vastus lateralis to the medial and, respectively, lateral border. The quadriceps muscle is the active stabilizer of the patella. The apex (syn. distal pole) of the patella is extra-articular and is the site of the attachment of the patellar tendon. The patellar tendon, the major passive stabilizer of the patella, inserts distally to the tibial tuberosity and has a length of approximately 4–6 cm. The thickness of the tendon is 5–6 mm and the width is 3 cm at the patellar insertion and 2.5 cm at the tibial insertion [2]. Normal tendons have uniformly low signal intensity on all MRI sequences and display distinct margins [3]. The quadriceps muscle and tendon, patellar tendon, patella, and patellar retinaculum represent the extensor mechanism of the knee [1].
The patellar anterior surface is related to the quadriceps tendon and to the prepatellar bursa that is not apparent on MR images in the absence of bursitis. The patellar posterior surface is divided into a superior intra-articular surface and a lower extra-articular portion. The mean patellar height varies between approximately 4 and 5 cm from which a height of 2.4–3.7 cm represents the intra-articular segment [4]. The intra-articular surface is divided into seven facets [5]. Three medial and three lateral facets are in contact with the medial and lateral femoral condyles, and the odd facet on the medial border of the patella articulates with the medial femoral condyle only in deep knee flexion [5].
The medial and lateral retinacula are passive stabilizers of the patella. The medial patellar retinaculum is part of the anterior third of the medial joint capsule and is formed by the superficial layer of MCL and the deep crural fascia [6]. It extends from the proximal aspect of the medial border of the patella to the medial femoral epicondyle and represents, together with the medial femoropatellar ligament (MPFL), the most important patellar ligamentous stabilizers. The medial femoropatellar ligament inserts to the medial femoral epicondyle, and its fibers fan out to the patella where they insert to the most prominent medial edge of the patella [7]. The ligament is adherent to the vastus medialis obliquus, and its fibers may be hidden to a variable extent by the overlying muscle and tendon [8]. The ligament is 55 mm long and 3–30 mm wide and is the primary passive restraint to patellar lateral displacement [7]. On MR imaging, the medial retinaculum and the medial femoropatellar ligament are seen as well-defined low-signal-intensity bands but are often difficult to be distinguished from each other (Fig. 7.1) [9].


Fig. 7.1
Normal medial and lateral retinaculum in a 34 year old female. Axial proton-density (PD) FSE fat-suppressed image shows the medial (small arrow) and lateral retinacula (large arrow) as well-defined low-signal-intensity bands connecting the patella (star) with the femoral condyles
The lateral retinaculum has a more complex anatomy with three layers difficult to delineate both macroscopically and on MR imaging, because of converging and interdigitating structures (Fig. 7.1) [10]. The superficial layer is represented by the deep fascia that is not adherent to the patella. Deep to it, there is the anterior longitudinal expansion of the iliotibial tract that merges with the anterior quadriceps aponeurosis and attaches to the patella (syn. intermediate layer) [11]. The intermediate layer is the most substantial layer of the lateral retinaculum [10]. Although these fibers are often called the lateral femoropatellar band, there is no attachment to the femur, except indirectly via proximal and distal attachment of the iliotibial band (Fig. 7.2) [12]. The deepest layer of the lateral retinaculum is part of the joint capsule and is referred to as the lateral femoropatellar ligament reinforced by an epicondylopatellar and a patellotibial band that are less substantial [10].
Fig. 7.2
The intermediate layer of the lateral retinaculum in a 17 year old male. Axial proton-density (PD) FSE fat-suppressed image shows the anterior longitudinal expansion of the iliotibial tract (large arrow). Note that there is no direct connection to the femur or to the lateral collateral ligament (curved arrow)
7.1.2 Femoropatellar Joint
The femoropatellar joint is formed by the posterior intra-articular surface of the patella and its counterpart represented by the femur trochlea. The articular congruence between femoral and patellar surfaces enables the static stability of the patella. However, there are anatomical variants of the patellar facet sizes by comparing the configuration of the medial and lateral bony facets [13]. In Wiberg type I patella (prevalence of 10 %), the medial and lateral facets are concave and are almost equal in size (Fig. 7.3). In Wiberg type II patella (prevalence of 65 %), the medial facet is flat and is smaller than the lateral facet (Fig. 7.4). In Wiberg type III patella (prevalence of 25 %), the medial facet is also smaller than the lateral facet but has a convex shape (Fig. 7.5). The femoral trochlea consists of the medial and lateral facets of the femoral sulcus or femoral groove. On axial MR imaging, the lateral facet of the trochlea is more elevated and larger than the medial facet. The sulcus angle of the trochlea is normally less than 144° [14].
Fig. 7.3
Wiberg type I patella in a 45 year old female. Axial proton-density (PD) FSE fat-suppressed image shows that the medial (large arrow) and lateral (small arrow) facets are concave and are almost equal in size
Fig. 7.4
Wiberg type II patella in a 34 year old female. Axial proton-density (PD) FSE fat-suppressed image shows that the medial facet (large arrow) is much smaller than the lateral facet (small arrow) and is flat or even concave
Fig. 7.5
Wiberg type III patella in a 50 year old female. Axial proton-density (PD) FSE fat-suppressed image shows that the medial facet (large arrow) is much smaller than the lateral facet (small arrow) and has a convex shape
Both surfaces, patellar facets and femoral trochlea, are covered by articular cartilage, but there are significant differences between the subchondral bone geometry and the articular cartilage surface geometry [15]. This means that the measurements on plain radiographs or on computed tomography (CT) may not represent the real articular femoropatellar congruence and all measurements, which are based on these imaging modalities, should be used with caution. MRI is the only imaging method that is able to reveal the real articular congruence due to visualization of the articular cartilage and the subchondral bone at the same time. This especially applies to cases with normal morphology of trochlea or in a low-grade dysplasia.
Whenever quantitative or semiquantitative measures of the patellar position are required or asked for, we suggest determining the position of the articular patellar cartilage in relation to the trochlear cartilage [16]. This relation can be quantitatively assessed on sagittal MR images by using the patellotrochlear index measured with the knee fully extended (Fig. 7.6) [17].
Fig. 7.6
The patellotrochlear index in a 16 year old female. Sagittal proton-density (PD) FSE image enables the calculation of the patellotrochlear index. The baseline trochlea (BT) is measured as the distance from the most proximal trochlear cartilage margin to an horizontal line which is drawn at the inferior margin of the patellar cartilage (horizontal line). The baseline patella represents the length of the patellar cartilage measured from the most proximal margin of the patellar cartilage to the most distal margin of the cartilage (BP). The patellotrochlear index is calculated using the formula: BT/BP × 100. An index value of more than 50 % documents patella baja and an index value less than 12.5 % documents patella alta. These values are not valid in the cases of patients with patellar dislocation
7.1.3 Infrapatellar Fat Pad and Suprapatellar Fat Pad
The infrapatellar fat pad, also referred as Hoffa’s fat pad, is intracapsular and extrasynovial and is bordered by the patellar tendon and joint capsule anteriorly, proximal tibia and deep infrapatellar bursa inferiorly, synovia posteriorly, and the inferior pole of the patella superiorly. On MR images, it appears as a relatively homogeneous triangular shape fatty tissue on sagittal plane. Some vessels might be seen within the fat pad (Fig. 7.7). An infrapatellar synovial plica may be present, extending from the distal pole of the patellar to the intercondylar notch close to the anterior cruciate ligament (Fig. 7.8).
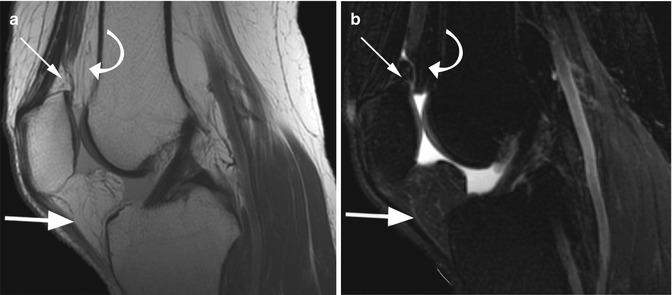
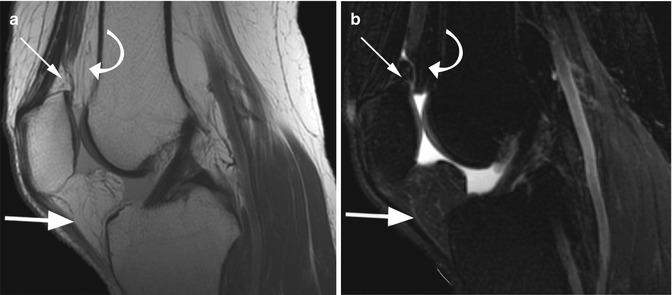
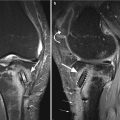
Fig. 7.7
The infrapatellar fat pad (Hoffa’s fat pad) and the suprapatellar fat pad in a 34 year old female. Sagittal proton-density (PD) FSE image (a) and sagittal T2-weighted FSE fat-suppressed image (b) show the infrapatellar fat pad as a triangular shape fatty tissue between the patella and proximal tibia (large arrows in a, b). Note the presence of small vessels within the fat pad. The suprapatellar fat pad is divided into an anterior suprapatellar fat pad (small arrows in a, b) and a posterior suprapatellar fat pad (curved arrows in a, b)
Fig. 7.8
Infrapatellar synovial plica in a 22 year old male. Sagittal proton-density (PD) FSE image shows a linear hypointense structure extending from the distal pole of the patellar to the intercondylar notch (arrow)
The suprapatellar fat pad is also intracapsular and extrasynovial and is divided into an anterior suprapatellar fat pad (quadriceps fat pad) and a posterior suprapatellar fat pad (prefemoral fat pad). Both fat pads are often separated by the suprapatellar bursa (Fig. 7.7).
7.1.4 Patellar Calcar
Patellar calcar is a constant and normal anatomical finding of the patella represented by a dense bone lying as a ridge within the subchondral patellar bone. The patellar calcar is always present on the lateral facet of the patella and is better seen on sagittal images as a linear low-intensity-signal change or the subchondral patellar bone (Fig. 7.9) [18]. Although the presence of this normal bone condensation is not correlated with any clinical symptoms, recognizing the imaging appearance is important in order to exclude a misinterpretation of a normal finding as osteochondritis dissecans or patellar fracture [18].
Fig. 7.9
Patellar calcar in a 27 year old male. Sagittal proton-density (PD) FSE image shows a linear low-signal intensity line within the subchondral area of the lateral facet of the patella (arrows) which represents a normal bone condensation
7.2 MRI Pathological Findings
Abnormalities of the patella, femoropatellar joint, and infrapatellar fat pad are often associated with anterior knee pain which is one of the most frequent complaints in orthopedics and sports medicine practice. However, there is a long list of possible differential diagnoses of anterior knee pain that implies bone and/or soft tissue pathology (Table 7.1) [19].
Table 7.1
Possible causes of anterior knee pain
Anatomical structure | Pathology |
|---|---|
Patella | Patella bipartite |
Unstable synchondrosis | |
Pseudoarthrosis | |
Patellar alta/patella baja | |
Patellar dislocation/subluxation | |
Patellar/femoral fractures/contusions | |
Subchondral bone and cartilage (patella/femur) | Cartilage injuries – osteoarthritis/arthritis |
Subchondral edema | |
Subchondral cysts | |
Osteochondritis dissecans | |
Bone tumors | |
Meniscus | Meniscal tear |
Meniscal cyst | |
Meniscal extrusion | |
Muscles and tendons | Tendinosis – quadricipital tendon/patellar tendon |
Tendon tear – quadricipital tendon/patellar tendon | |
Osgood-Schlatter disease | |
Sinding-Larsen-Johansson disease | |
Muscle tumors | |
Synovia | Inflammatory synovitis |
Pigmented villonodular synovitis (PVNS) | |
Prepatellar/infrapatellar bursitis | |
Medial plica syndrome | |
Infrapatellar plica syndrome | |
Synovial osteochondromatosis | |
Synovial sarcoma | |
Infrapatellar fat pad | Hoffa disease |
Intra-articular chondroma | |
Postoperative fibrosis (including cyclops lesion) |
7.2.1 Patellar Dysplasia
The patella is cartilaginous at birth and ossifies from one or several centers after the age of three years. The most common patellar dysplasias are hypoplasia, aplasia, patella bipartite or multipartite, duplication, and fragmentation. Congenital hypoplasia and aplasia are very rare diseases and are the result of the phenotype and gene defects including the nail patella syndrome or hereditary osteo-onychodysplasia (HOOD disease), small patella syndrome, isolated patella aplasia or hypoplasia, Meier-Gorlin syndrome, RAPADILINO syndrome, and genitopatellar syndrome [20].
Patellar duplication or double-layered patella may be seen in multiple epiphyseal dysplasia and is identified on axial and sagittal MR images as two separate anterior and posterior layers [21]. The fragmentation of the patella may involve the superior or the inferior pole. It may be seen in patients with cerebral palsy. The excessive tension in the quadriceps tendon, usually in the presence of a flexion contracture, appears to cause the lesion [22].
Patella bipartite is a developmental dysplasia in which the ossification centers fail to fuse and may be a cause of anterior knee pain. Usually, the bipartite fragment is situated at the superolateral quadrant of the patella at the insertion of the vastus lateralis muscle (type III patella bipartite). Patella bipartite occurs usually bilaterally. Very rarely the fragment is located at the medial border (type II patella bipartite) or at the inferior pole (type I patella bipartite) [23]. The bone fragments are connected through a synchondrosis, and the associated patellar articular cartilage remains intact in most of the cases. However, due to overuse or acute injury, synchondrosis may be disrupted allowing friction and abnormal motion that can lead finally to pseudoarthrosis [24]. In clinical practice, patella bipartite is repeatedly misdiagnosed as patellar fracture. The continuity of the articular cartilage, the presence of the cartilage between the fragments (normal synchondrosis), and the absence of abnormal signal intensity within the fragments are normal MRI findings in uncomplicated patella bipartite.
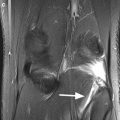
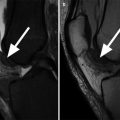
MR imaging is also the method of choice for differentiation between symptomatic and asymptomatic patients with patella bipartite by demonstrating the presence of bone edema within the patellar fragment and along the margins of synchondrosis that is the result of impaction and trabecular injuries of the bone (Fig. 7.10). The presence of fluid signal between the patellar body and the bipartite fragment represents a suggestive MRI finding for pseudoarthrosis (Fig. 7.11) [23].
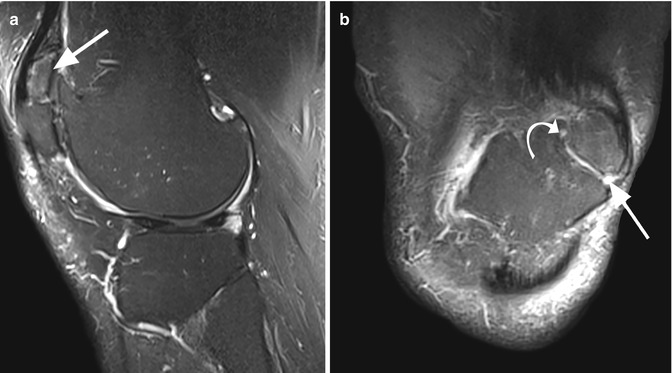
Fig. 7.10
Patella bipartite in a 21 year old male with intermittent anterior knee pain. Axial proton-density (PD) FSE fat-suppressed image shows normal synchondrosis (presence of the cartilage) between patellar fragments with subchondral bone marrow edema along the margins of synchondrosis (arrows)
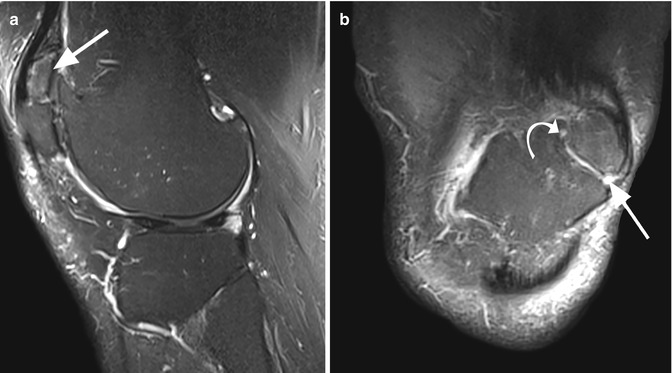
Fig. 7.11
Complicated patella bipartite in a 57 year old male. Sagittal T2-weighted fat-suppressed image (a) shows an irregular bipartite fragment (arrow). Coronal proton-density (PD) FSE fat-suppressed image (b) shows the presence of fluid signal between the patellar body and the bipartite fragment (arrow) and even a small subchondral cyst (curved arrow). Both signs are suggestive for pseudoarthrosis
7.2.2 Patella Alta and Patella Baja
Patella alta or high-riding patella is a patella that is situated too high above the femoral trochlea. Although patella alta is considered a normal anatomical variant secondary to a long patellar tendon, the high position of the patella leads to reduced contact area with the femoral trochlea and may cause pain due to instability. In conjunction with other factors, this increases the risk of patellar lateral dislocation [25, 26]. Patella baja is the result of the shortening of the patellar tendon and may occur following trauma or surgery (harvesting of a patellar tendon autograft) [27].
Numerous methods are used to determine the patellar height, but there is a high frequency of differing results in determination of patellar position [28]. This finding has led many clinicians to question the utility of commonly used ratios for accurate assessment of patellar position [28]. Nevertheless, some of these measures are still used and requested.
The first method described was the Insall-Salvati ratio that is calculated as the ratio between the length of the patellar tendon and the length of the patella on lateral radiographs. It is ideally measured with the knee in 30° flexion [29]. As on radiographs, the Insall-Salvati ratio can be reliably assessed on sagittal MR images independent on the degree of knee flexion (Fig. 7.12), and a ratio greater than 1.3 is suggestive for patella alta, while a ratio smaller than 0.8 is suggestive for patella baja [5, 30].


Fig. 7.12
Insall-Salvati ratio in a 34 year old female. Insall-Salvati ratio is calculated as the ratio between the length of the patellar tendon (PTL) and the length of the patella (PL). A ratio greater than 1.3 is suggestive for patella alta, while a ratio smaller than 0.8 is suggestive for patella baja
Several studies have demonstrated that the Insall-Salvati ratio and modified Insall-Salvati ratios do not correlate with femoropatellar cartilage congruence [28, 31]. Moreover, this ratio may be influenced by form variations of the patella and variations of the patellar tendon (Sinding-Larsen or Osgood-Schlatter diseases, surgical interventions) [17]. Biedert and Albrecht [17] have thus proposed another measure, namely, the patellotrochlear index. It is thought to provide a more reliable measurement of the patellar height because the most important factor in patellar position evaluation is the position of the articular cartilage in relation to the trochlear cartilage [16]. The patellotrochlear index is calculated as the ratio between the baseline trochlea, measured as the vertical length of the femoral trochlea that is engaged with the patella, and the baseline patella, calculated as the vertical length of the patellar articular surface (Fig. 7.6). An index value of more than 50 % documents patella baja, and an index value less than 12.5 % documents patella alta [17].
7.2.3 Patellar Instability
The stability of the patella is maintained by a complex interaction between bone and soft tissue structures (Table 7.2). Morphological variations of the bone anatomy of the femoropatellar joint and ligamentous insufficiencies can disturb this interaction resulting in patellar instability [32]. Patellar instability is one of the most frequent clinical syndromes and is defined as an abnormal lateral course of the patella during knee flexion with or without dislocation. Chronic instability of the femoropatellar joint and recurrent dislocation may lead to progressive cartilage damage and severe arthritis if not treated adequately [9]. In patients without any history of knee dislocation, the diagnosis is difficult because anterior knee pain is often nonspecific and the clinical examination of the knee may be normal. The most important predisposing factors for instability are trochlear dysplasia, patella alta, and the lateralization of the tibial tuberosity.
Structure | Role in patellar stability |
|---|---|
Femoropatellar bone and cartilage congruence | Static stability: restraint to lateral patellar displacement at flexion angles more than 30° |
Quadriceps muscle | Active stability: quadriceps contraction pulls the patella proximally, posteriorly, and slightly laterally; the force of quadriceps is resisted by patellar tendon tension |
Retinacula | Passive stability: medial femoropatellar ligament is the most important passive restraint to lateral patellar displacement in early flexion (0–30°) |
Trochlear dysplasia is believed to be a developmental morphological abnormality, often present bilaterally, defined by the flattening of the femoral trochlea that can result in lateral patellar dislocation with flexion [36]. There are several quantitative and qualitative MRI criteria for the diagnosis of trochlear dysplasia. The mean trochlear depth in normal knees 3 cm above femorotibial joint level including the cartilaginous surface is 5.2 mm (Fig. 7.13) [19]. On axial MR images at this level, a trochlear depth less than 3 mm has a sensitivity of 100 % and a specificity of 96 % for trochlear dysplasia [19].
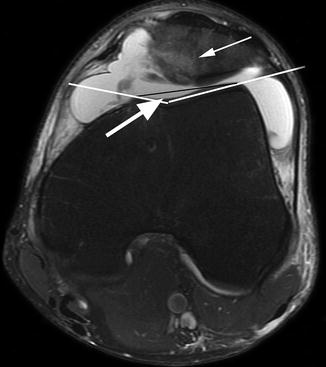
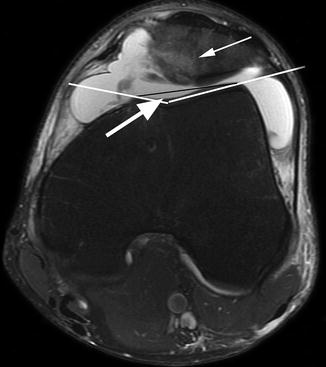
Fig. 7.13
Trochlear dysplasia in a 32 year old male. Axial proton-density (PD) FSE fat-suppressed image 3 cm above femorotibial joint level shows that the trochlear depth is less than 3 mm (large arrow). Note the osteochondral fracture of the medial patellar facet (small arrow) resulting from lateral patellar dislocation
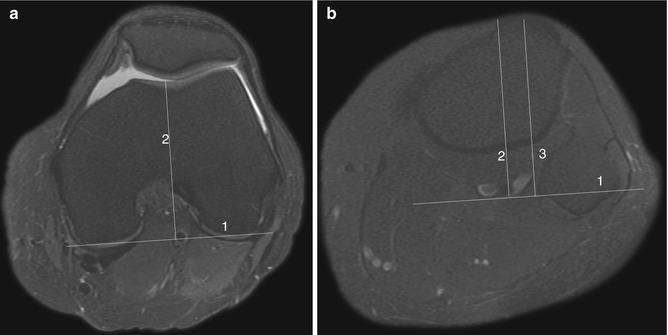
The lateral trochlear inclination and trochlear facets asymmetry are other quantitative MR findings that can be measured on axial images. The lateral trochlea inclination enables evaluation for the presence of dysplasia at the proximal portion of trochlea and is measured on the first craniocaudal image that demonstrates cartilaginous trochlea by means of a line tangential to the subchondral bone of the posterior aspect of the two femoral condyles crossed with a line tangential to the subchondral bone of the lateral trochlear facet (Fig. 7.14) [37]. A horizontal lateral facet with an inclination angle smaller than 11° is suggestive for diagnosis [37]. Trochlear facet asymmetry 3 cm above the femorotibial joint level is measured by lateral facet length (LFL) to medial facet length (MFL) ratio (LFL/MFL × 100) (Fig. 7.15) [19]. A value of 40 % or less shows a decrease of the lateral facet length having a sensitivity of 100 % and a specificity of 96 % for diagnosis [19].
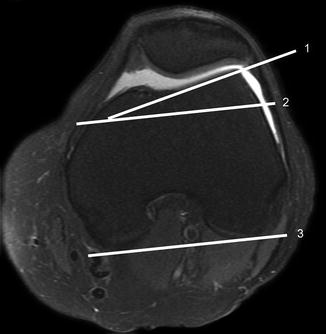
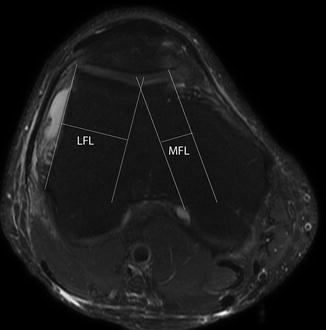
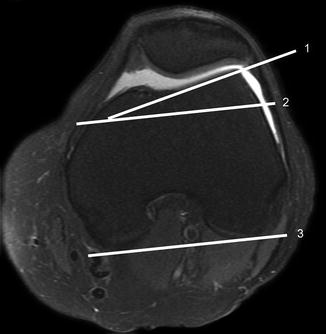
Fig. 7.14
The lateral trochlear inclination in a 34 year old female. The first craniocaudal axial proton-density (PD) FSE fat-suppressed image that demonstrates cartilaginous trochlea enables the measurement of the lateral trochlear inclination. An inclination angle smaller than 11° is suggestive for trochlear dysplasia. The angle is measured between the cartilaginous femoral trochlea (line 1) and a parallel line (line 2) with the posterior plane of the femoral condyles (line 3)
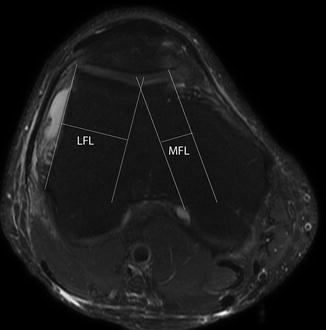
Fig. 7.15
Measurement of the trochlear facet asymmetry in a 43 year old male on axial proton-density (PD) FSE fat-suppressed image 3 cm above femorotibial joint level. The trochlear facet asymmetry is measured by lateral facet length (LFL) to medial facet length (MFL) ratio (LFL/MFL × 100). A value of 40 % or less shows a decrease of the lateral facet length having a sensitivity of 100 % and a specificity of 96 % for diagnosis of trochlear dysplasia
The presence of a nipplelike anterior prominence at the superior border of the trochlea on midsagittal MR images can be used as semiquantitative criteria for trochlea dysplasia with a 91 % specificity when the nipplelike prominence is larger than 2 mm (Fig. 7.16) [19]. However, the sign is reliable only in patients without degenerative changes of the femoropatellar joint.
Fig. 7.16
Semi-quantitative criteria for trochlea dysplasia: nipplelike anterior prominence at the superior border of the trochlea in a 43 year old male. Midsagittal proton-density (PD) FSE image shows a prominence larger than 2 mm in a patient with trochlear dysplasia (arrow)
The lateralization of the tibial tuberosity and the lateralization of the patella are other quantitative findings that can be used in the evaluation of patellar instability. The lateralization of the tibial tuberosity results in lateral displacement of the patella during flexion. On axial MR images, the lateralization of the tibial tuberosity can be measured by using the tibial tuberosity-trochlear groove distance by superimposing axial images through the tibial tuberosity and the apex of the intercondylar groove (Fig. 7.17) [9, 38]. A distance greater than 2 cm is usually associated with patellar instability [9].