Fig. 3.1
Diagram of a tube containing two different coloured fluids to demonstrate laminar flow: (a) no flow at rest; (b) a velocity profile is created as the red fluid begins to flow. Flow is faster and occurs further at the centre compared to the periphery
Copyright: [Author]
If bends are introduced into the tube, impediments like venous valves are found in the wall, the pipe diameter is very small or the velocity is very high, then turbulence occurs. This causes the blood to divert from its parallel path and flow in all directions, even towards the wall. This results in an increase in friction and resistance. Consequently, the forward velocity is reduced and pressure on the wall increases.
3.1.2 Relative Pressures in Veins
Veins are expandable adapting their diameter and length to volume and pressure. This adaptability is called compliance. If the vein walls were rigid, the intravenous pressure would rise in direct proportion to an increase in volume. However, veins are able to contain differing amounts of blood without these pressure increases. The compliance of veins is much greater than that of arteries making them an ideal blood reservoir for the body. In fact, 70–85 % of the circulating blood volume is in the post-capillary veins, including the deep and superficial leg veins (Dodd and Cockett 1976).
The hydrostatic pressure differences within veins are generally predetermined by gravity. The pressure in the right atrium of a healthy person is equal to 0 mmHg. After 30 s standing still, the pressure in both the deep and superficial veins in the region of the foot, regardless of whether the venous system is healthy or pathological, is 90–100 mmHg. This is determined by the hydrostatic pressure of the blood column from the right atrium to the foot. In this way, a hydrostatic pressure difference is created by the force of gravity. This needs to be exceeded before antegrade flow can resume.
When the calf muscles contract during muscular systole, the pressure in the deep veins rises to up to 235 mmHg. This is higher than systolic blood pressure. Pressures of up to 115 mmHg are found in the thigh. This increased pressure exceeds that of the hydrostatic column, thereby driving blood upwards towards the heart. After muscle contraction, venous valves prevent the volume expelled from flowing backwards. The valves close during diastole and divide the hydrostatic column into sections. This process is called fractionation. During calf diastole, very low pressures of about 25 mmHg are generated in the deep veins. This leads to a new pressure difference between the deep and superficial veins causing drainage of the superficial veins inwards into the deep veins.
The frequently described condition of venous hypertension occurs in the superficial veins when the system decompensates. In this situation, calf muscle systole is not longer able to cope with the excess recirculating volume. This excess of volume is caused by reflux down the superficial veins. Varicose veins then begin to appear with stretching of the vein walls before any noticeable increases in pressure. When the patient is standing still, the pressure in the deep and superficial veins approximates to hydrostatic pressure. If the perforating veins are incompetent, they reflux during muscular systole causing blood to flow outwards into the superficial veins.
The flow pattern influences the pressure transmitted onto the vein wall. Turbulent flow is more likely to cause higher pressures than laminar flow. The properties of the wall are also important in resisting dilatation. Interestingly, unlike superficial tributaries, the great saphenous vein almost never becomes varicose, irrespective of whether it is used as an arterial bypass or is subjected to venous pressures considerably higher than arterial.
3.2 Recirculation
In healthy veins, blood flows from superficial to deep veins, from tributaries into the saphenous or deep veins directly and from the saphenous trunks into the deep veins (Fig. 3.2). Venous blood flows upwards generally leaving the leg through the deep system. As shown in Fig. 3.2, saphenous blood in the standing patient during muscle diastole has a brief duration of retrograde flow between a perforating vein and the next higher valve. In healthy veins, the quantity of blood flowing in superficial veins is very small. The venous reservoir in health consists almost entirely of the deep and muscle veins.
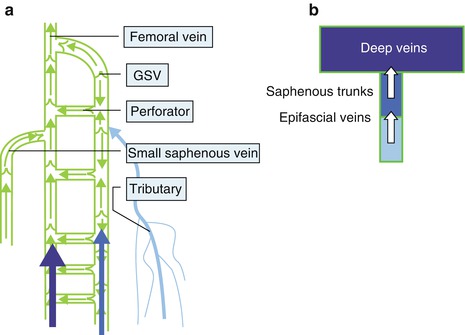
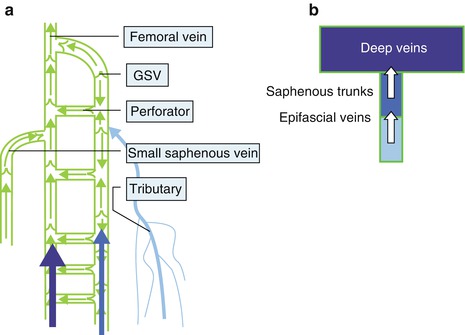
Fig. 3.2
(a) Diagram of the blood flow in healthy veins, standing; (b) diagram of the total blood volume in the veins of a healthy subject. The arrows indicate that the blood in the leg flows from the superficial to the deep veins from where it leaves the leg (From Mendoza (2002); by kind permission of Arrien GmbH)
Copyright: Arrien, Wunstorf
Recirculation can cause varicose veins which is dependent on two conditions:
1.
The flow direction must be reversed so that blood flows from the deep to the superficial veins or from a saphenous vein into tributaries. The starting point of reverse flow is called the reflux source. The receiving vessel is not adapted to receive this flow and therefore dilates.
2.
This reflux volume must re-enter the deep veins at some point further down the leg; otherwise, the blood column would thrombose. Re-entry occurs through perforating veins or healthy saphenous veins. They may become secondarily dilated because they carry the same extra volume as the dilated superficial veins which are pathologically filled. This may lead to secondary incompetence.
In isolated saphenous vein incompetence, without the participation of any tributaries, recirculation occurs between the deep veins and the saphenous veins (Fig. 3.3a). The saphenous vein therefore becomes volume overloaded (Fig. 3.3b). Despite this, it still continues to drain the normal tributaries with blood flowing from the tributaries through the refluxive saphenous vein and into the deep veins. Eventually, the net blood flow is out of the leg through the deep veins, but this is constantly hampered by the recirculation.
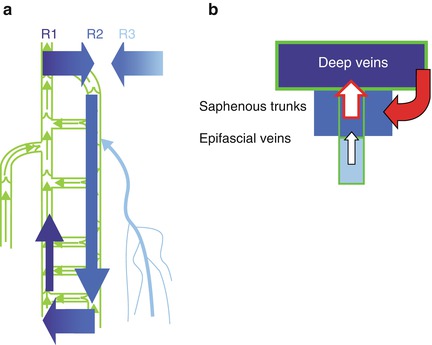
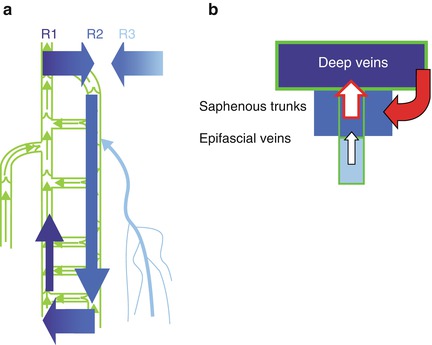
Fig. 3.3
(a) Blood flow with reflux confined to the great saphenous vein. Recirculation starts from the deep veins and enters the great saphenous vein where it refluxes down until it re-enters back into the deep veins; (b) diagram of the total blood volume in the leg veins in the recirculation loop shown in (a). The healthy veins are shown in green (cf. Fig. 3.2b) (From Mendoza (2002); by kind permission of Arrien GmbH)
Copyright: Arrien, Wunstorf
With saphenous vein incompetence and additional refluxive tributaries, the situation is more complex. The tributaries may also become overloaded by participating in the recirculation loop (Fig. 3.4). Assuming healthy deep veins, this results in an extra volume load through a perforating vein as well as the deep veins. The volume burden caused by recirculation may result in secondary deep venous insufficiency. This is because the blood volume which flows refluxively into the superficial veins must be transported inwards in addition to the blood normally present in the deep veins (Fig. 3.4b; note the wider profile of the dark blue box)
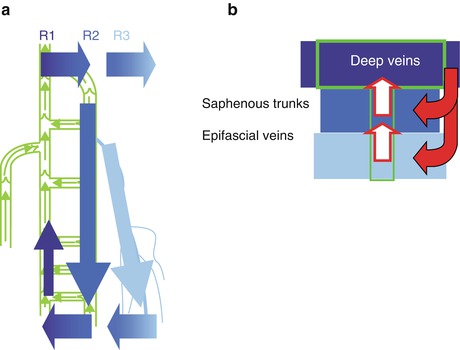
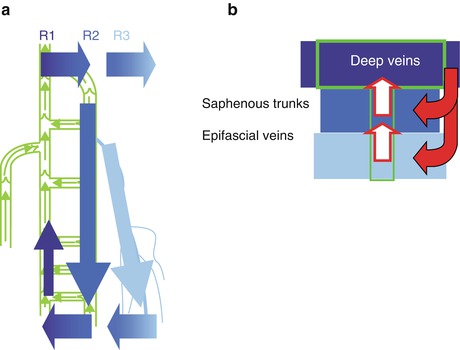
Fig. 3.4
(a) Diagram of recirculation in the great saphenous vein and its tributaries with re-entry through perforating veins at the ankle; (b) diagram of the blood volumes in the three vein systems. The epifascial and saphenous systems are completely overloaded. However, blood will only leave the leg through the deep veins (From Mendoza (2002); by kind permission of Arrien GmbH)
Copyright: Arrien, Wunstorf
Only those perforating veins which have suffered secondary dilatation from refluxive outward flow will serve as re-entry points for a recirculation. Undilated perforating veins are present but do not participate in recirculation. This can be demonstrated by measuring the flow in a varicose vein, without compressing the perforating vein, and then measuring the flow in the re-entry perforating vein under compression. In the first case, there is a typical reflux curve. In the second case, there is no retrograde flow during muscular diastole. This is termed the reflux elimination test (Zamboni et al. 2010) (see Sect. 4.2.9).
3.2.1 Analysis of the Flow Curve in PW Mode
In B scan with colour duplex ultrasound, it is easy to see the flow direction. However, this information is often not sufficient (Fig. 1.20), and important information can be lost. Therefore, when investigating venous insufficiency, it is recommended to analyse the PW curve at a minimum of one point at least, since this is the easiest way of confirming a diagnosis of reflux.
Unlike an arterial examination, flow curve analysis is only a semi–quantitative assessment. Flows may differ in the same vein during the same examination, so flow velocities and blood volumes should not be regarded as absolute values. They depend on how long the patient has been standing, how long it is since the last stimulation manoeuvre, how much force was used or even the size of the examiner’s hand.
The PW Doppler mode measures the velocities of the erythrocytes per unit of time in the measurement window. The PW curve records these velocities as white points along the time axis. If the velocities of the individual erythrocytes are similar, as in laminar flow, a curve will be formed with a white contour and a black space under the curve. If different velocities are recorded (turbulent flow), the whole curve will be filled in with white points.
The following data are important (Fig. 3.5):
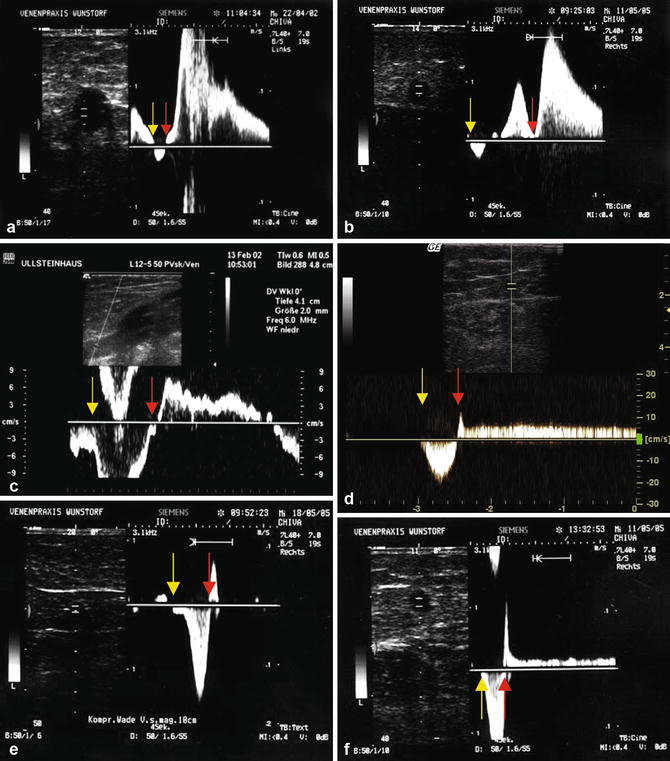
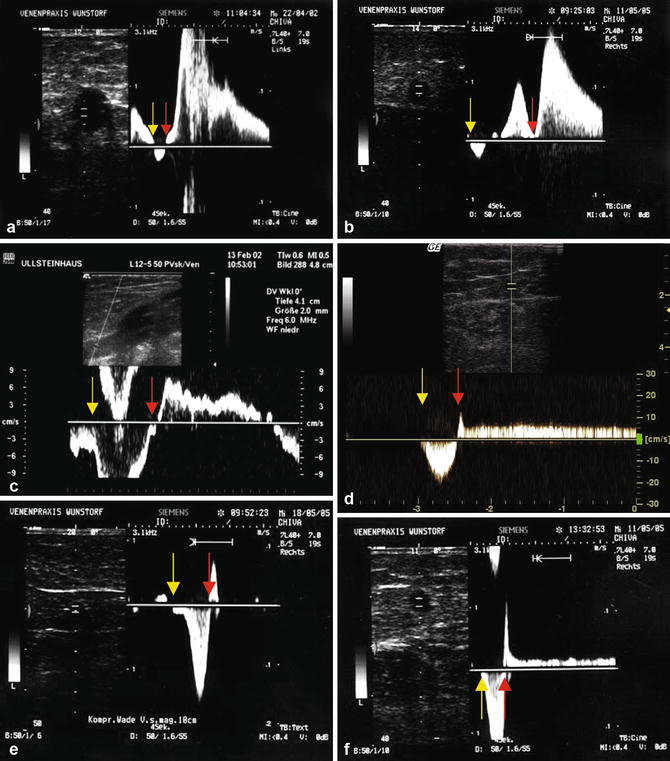
Fig. 3.5
Flow curve analysis. All measurements except (c) were taken from the great saphenous vein in the mid thigh. The yellow arrow indicates the beginning of muscular systole, and the red arrow the beginning of diastole. (a) Sharp rise, high reflux velocity. The area under the curve is not filled indicating that the flow is not very turbulent. Length of reflux is approximately 4 s which is clearly stronger than antegrade flow. (b) Short antegrade flow with reflux in two phases: one short, not very rapid curve during the period of muscular contraction (explanation Fig. 6.15) and one longer-lasting, faster curve. The flow is turbulent as the area under the curve is almost completely filled with white. This indicates the wide range of different velocities being measured which are typical of turbulence. (c) Flow in the popliteal vein just above an incompetent saphenopopliteal junction. Almost laminar flow as the curve contour is thin. The blood volume which flows in an antegrade direction during muscular systole is much greater than the volume which flows back during diastole. This blood flows in a retrograde direction from the popliteal vein into the refluxive small saphenous vein. The popliteal vein itself is not incompetent (explanation Fig. 6.12c). (d) Slow, long-lasting reflux. (e) Antegrade flow during muscle contraction with a short reflux until the valve closes. There is a sharp rise lasting <0.5 s confirming the vein is competent. (f) Short, steep reflux at first until valve closure, as in (e), but followed by a slow, long-lasting reflux. The saphenofemoral junction is competent. The short retrograde flow indicates the closure of the first subterminal valve. The long-lasting reflux which follows is from the epigastric vein draining into a refluxing great saphenous vein
Copyright: [Author]
Velocity of retrograde flow (curve height).
Duration of retrograde flow (curve length).
Evolution or change in velocity – velocity profile (curve contour).
Area under the flow curve with reflux as compared to area under the flow curve with antegrade flow. This estimates the blood volume ejected upwards during the stimulation manoeuvre as compared to the blood volume which finally flows towards the foot.
Filling of the area under the flow curve – black with laminar or white with turbulent flow.
Flow curve analysis in the following veins is particularly important:
As a rule, a high reflux velocity is associated with a sharp rise and a short reflux duration (Fig. 3.5a, b). This is typical in large-calibre venous insufficiency from reflux sources with large lumina. These are generally saphenous vein junctions which permit fast filling of the incompetent vein from a large blood reservoir of deep veins and in large-calibre re-entry perforating veins which allow a fast drainage of the recirculation volume.
There are four possible causes of slow reflux which is usually long-lasting (Fig. 3.5d, f and Sect. 3.2.3):
1.
Small blood reservoir as a source of reflux (e.g. reflux from a healthy saphenous vein into a refluxive tributary)
2.
Small-calibre link between reflux source and refluxive vessel (e.g. reflux from the pelvis through the pudendal or epigastric veins)
3.
Lack of compliance in the refluxive vein so that it cannot receive large blood volumes (e.g. due to sclerosis or irradiation)
4.
Small-calibre drainage (e.g. through re-entry perforating veins)
3.2.2 Definitions of Reflux
Recirculation
The pathological situation in varicose vein disease is recirculation. The blood which should flow towards the heart leaks out of the deep veins at some point to enter the superficial veins where it overloads a segment. Then usually further down the leg, this re-enters the deep system where it flows upwards once more towards the heart. This recirculation is the pathophysiology behind varicose vein disease. It describes the superfluous blood circuit in a varicose vein which has been termed a repetition or private circuit (Trendelenburg 1891). These terms are also applied when blood from a competent saphenous vein fills an incompetent tributary.
Volume Overload of the Superficial Venous System
The affected veins in the superficial venous system are filled with more blood by the recirculation than the veins were originally supposed to contain. In response to this volume overload, the vein walls dilate.
Reflux
This is defined as pathological blood flow following normal, antegrade flow. Blood which flows normally towards the heart during muscular systole then flows in a retrograde direction towards the foot to become reflux. Reflux is the part of the recirculation loop which occurs in incompetent veins during diastole. It includes blood already within the vein from antegrade flow as well as blood which originally entered another vein like the deep veins and then passed through an incompetent valve into the refluxive superficial vein. The reflux fills the incompetent vein with an additional volume of blood.
Drainage
This is defined as blood in retrograde flow, which physiologically belongs to the vessel. It is not extra blood and therefore does not overload the vein. An example of drainage occurs in the venous tributaries draining into the vein of Giacomini after closure of the proximal reflux source. Another example is in the great saphenous vein after ligation of the saphenofemoral junction or crossectomy. The saphenofemoral tributaries normally drain into the proximal great saphenous vein. After closure of an incompetent junction, this blood is diverted retrograde down the great saphenous vein during muscular diastole to the next perforating vein further down through which it enters the deep veins. The great saphenous vein is the correct drainage for this blood, which is neither a pathological volume nor part of a recirculation loop.
3.2.3 Drained and Poorly Drained Systems
The rate of recirculation depends on two main variables:
The compliance of the refluxive vein
The calibre of the re-entry perforating vein
Compliance is the capacity of the vein wall to stretch (Sect. 3.1.2). It can receive different volumes of blood by varying its diameter. Indirect measurements of venous compliance can be achieved by measuring venous diameter standing and then lying. If there is little variation in the diameter, the elasticity of the wall is slight and its compliance is poor. Poorly compliant veins fill when the patient stands and are more likely to remain full if they have reduced venous elastic recoil. Patients with venous disease have an increased venous volume, increased rate of filling and reduced venous elastic recoil. These can be measured using air plethysmography.
If the patient has been standing for some time, the veins become quite full regardless of their compliance. The calibre of the re–entry perforating veins then has a considerable influence on the flow curve. During muscular diastole, only so much blood will flow towards the foot as can pass back into the deep veins through the perforating vein. Thus, the perforating vein acts like a gatekeeper throttling the rate of recirculation.
These two variables determine how well varicose veins drain. In general, good compliance is associated with large perforating veins (drained system), while poor compliance is associated with narrow re-entry points (poorly drained system).
3.2.3.1 Drained System
Because of their capacity to stretch, varicose veins receive more blood than their diameter at rest allows. This excess of blood then flows down to drain through the large-calibre perforating veins, allowing the vein to collapse. The flow curve in PW mode will rise steeply and then fall again over a few seconds during a stimulation manoeuvre. These patients generally have large-calibre, very winding varicose tributaries but little distress.
3.2.3.2 Poorly Drained System
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree