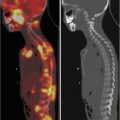

Fig. 14.1
Rhabdomyosarcoma. This patient presented with severe back pain, which proved to be secondary to metastatic RMS. Clinical work-up led to an FDG PET/CT (a–i). The MIP image (a) shows abnormal FDG uptake in L3 and also in the scalp. Transaxial CT and PET/CT fusion images showed abnormal FDG uptake in the L3 vertebra (b, c), corresponding to a compression fracture, an FDG avid right paraspinous soft tissue mass (d, e) with extension of FDG uptake into L3 vertebra and right neural foramen, and nodular scalp metastases (f, g). (h–j) An MRI (transaxial T1 images pre and post contrast) better defines the compression fracture and paraspinous disease. This was proven to be metastatic RMS. The asymptomatic primary tumor was found on the PET/CT of the lower extremities: MIP (k) and transaxial CT and PET/CT fusion images (l, m) show an FDG avid soft tissue nodule in the distal left foot. (n) Incidentally, a bone scan with Tc99m MDP shows increased tracer uptake in the L3 vertebra, but this study does not contribute any information that could not be derived (and better defined) by PET/CT. Bone scans contribute very little, if any, clinically relevant information in patients with RMS. All arrows are pointing at tumor sites
X-ray plain films remain essential for the primary assessment of bone tumors, even in the era of tomographic and molecular imaging; however, lytic lesions, principally occurring in Ewing’s sarcoma, remain undetectable on plain films until demineralization has reached 30–50 %. Some features that should be investigated on plain radiographs and may aid in the differential diagnosis include an assessment of the primary tumor matrix, presence or absence of margins around the primary bone lesion, presence of corticalis destruction, presence and configuration of periosteal reaction, and presence of new bone formation. OS (Fig. 14.2a–i) usually occur in the epiphysis, ES usually in the meta- and diaphysis (Fig. 14.3a–r). The 3-phase bone scan is still occasionally employed in the initial work-up of suspected bone tumors. Unfortunately, the findings are not specific although most malignant tumor will present with increased tracer uptake in all 3 phases of the scan. In particular in patients with OS, a whole-body bone scan may detect possible osseous metastases, as well as soft tissue metastases that contain a sufficient amount of osseous matrix leading to tracer retention. Whole-body scans are obtained 2–4 h after injection of Tc99m MDP. The amount of injected activity is based on body weight or body surface area. Guidelines for appropriate activities have been published by both EANM and SNM. Standard planar images of the torso can be supplemented by spot views of regions of interest if clinically necessary. SPECT or SPECT/CT is rarely performed because the yield of new and clinically relevant finings is low. The main imaging tests for malignant bone tumors are CT, MRI, and, increasingly, FDG PET. CT and MRI define the local extent of the primary tumor, any soft tissue involvement, and the relationship to neurovascular structures. However, peritumoral edema may lead to uncertainty in defining the exact tumor margins [4]. High-resolution CT of the lungs remains the most sensitive test for the detection of pulmonary metastases. High-pitch CT may reduce breathing and pulsation artifacts and may also lower the radiation dose to the patient [5]. FDG PET shows a high sensitivity for primary and recurrent tumors with sensitivities in the 85–95 % range [6, 7]. A recent meta-analysis studying the role of FDG PET and PET/CT in ES showed a high overall pooled sensitivity of 96 % and specificity of 92 % for both primary staging and restaging [8]. SUV numbers for OS and ES vary widely, from as low as 3.0 to as high as 20 [9]. However, it should be noted that aggressive benign bone lesions cannot be distinguished from sarcomas on PET alone. Some benign lesions, such as giant cell tumors, may show very high FDG uptake and SUV; conversely, some malignant tumors, in particular chondrosarcomas, show relatively low FDG uptake. Moreover, false-positive FDG uptake may occur at fractures, sites of infections, or inflammations (such as periostitis). Thus, the primary purpose of FDG PET lies in the evaluation for distant disease, in detection of possible recurrence, and increasingly in monitoring the response to neoadjuvant and adjuvant chemotherapy.

Fig. 14.2
Osteosarcoma. Newly diagnosed OS in a young patient with upper arm pain. (a, b) The plain radiograph shows a mixed lytic and sclerotic lesion with periosteal reaction and circumferential soft tissue mass. (c–e) Three-phase bone scan with Tc99m MDP performed at baseline shows increased radiotracer accumulation in the proximal left upper arm in the blood pool phase (c) and intense uptake in the metaphysis of the left humerus on the delayed images (d). The remainder of the bone scan is normal, thus excluding metastatic spread to other parts of the skeleton. (e–g) MRI images (sagittal T1 and fat-saturated axial T1 pre and post contrast) again show the primary tumor in the proximal humerus, predominantly subperiosteal circumferential soft tissue mass with thickness of up to 1.2 cm, and some penetration through the periosteum into adjacent soft tissues. There are also some prominent left axillary lymph nodes. (h) A follow-up bone scan after 3 months of neoadjuvant chemotherapy shows abnormal uptake in the proximal left humerus, similar to the appearance on baseline scan. Two weeks later, the patient underwent radical resection of the proximal left humerus with allograft placement (i); image I shows the status post resection and repair. The resected tumor measured 8.5 × 3.4 × 3.0 cm and was completely necrotic (100 % necrosis, grade 4 response). This case demonstrates that bone scan findings cannot be used to assess the response to chemotherapy. All arrows are pointing at tumor sites

Fig. 14.3
Ewing sarcoma. ES primary tumor in the left posterior chest wall with widespread metastatic disease. This adolescent patient initially presented with left shoulder pain and was misdiagnosed with tendinitis. Several weeks later, the patient palpated a lump in the chest wall, which led to further work-up and proper diagnosis. (a–g) FDG PET/CT: Maximum intensity projection (MIP; a) and transaxial images at baseline (b, c) show a hypermetabolic left posterior chest wall mass also involving pleura and lung. Numerous hypermetabolic metastases are seen in lungs (d, e), lymph nodes, and bones. (h–l) A follow-up PET/CT after 5 months of chemotherapy showed significant response with near resolution of primary tumor and metastases on MIP image (h) as well as on transaxial CT and PET/CT fusion images in the chest wall (i, j) and pelvic bones (k, l). The patient then underwent intensity-modulated radiotherapy (IMRT) to the chest wall, lungs, and ribs. PET/CT after completion of radiotherapy showed stable minimal uptake in a left femoral and right rib lesion. Approximately 1 year later, the patient noticed dark coloration of urine, and a clinical exam revealed minor jaundice. (m, n) PET/CT at that time showed new widespread metastatic disease that also involved the head of pancreas. (o) This was confirmed by subsequent MRI (axial T1 post contrast) that confirmed presence of a 3.4 × 2.3 cm mass in the pancreatic head. (p, q) Incidentally noted on PET/CT is mild FDG uptake surrounding distal left femur, status post radiotherapy to a single residual osseous metastasis at this site. This is a typical finding after localized radiotherapy. All arrows are pointing at tumor sites, except in (p) where the arrow points at postradiation inflammation in muscle
With very few exceptions (so-called osteosclerotic variant), ES is an osteolytic tumor and marrow-infiltrating tumor. Therefore, bone scans, which are generally more sensitive for osteoblastic lesions, may not be very informative in ES. Instead, distant disease is assessed better by FDG PET/CT or PET/MRI. In contrast, bone scans are quite sensitive for OS metastases because of the intense osteoid production and osteoblast activity in these lesions.
Nowadays, FDG scans are performed as PET/CT with 3D PET. If a dedicated CT scan of the torso has been ordered, it should be done in the same setting as the PET scan, using higher (as appropriate for patient age) dose settings. In this case, the usual low-dose CT of the PET/CT can be eliminated, and the data from the dedicated CT are used for PET attenuation correction, thus reducing overall radiation burden to the patient. The PET field of view should extend from the skull base to the proximal thighs unless the primary tumor is located more distally. Routine imaging of the lower extremities is not necessary in patients with primary tumor in the head and neck region or trunk [10] because the diagnostic yield is extremely low. The application of combined PET/MRI [11] in pediatric patients is of growing interest because this may lower the radiation dose from medical imaging [12] and possibly enable us to address a series of diagnostic and prognostic questions in one setting.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree