Fig. 1.1
Room analogy © SHOBEIRI 2013
Fig. 1.2
Room analogy with three compartments separated © SHOBEIRI 2013
Fig. 1.3
Room analogy with anterior, middle, posterior compartments, and the lateral walls marked © SHOBEIRI 2013
Fig. 1.4
Room analogy; pubocervical fibromuscularis and rectovaginal fascia separating the three compartments © SHOBEIRI 2013
Anteriorly, pubocervical fibromuscularis is attached to the levator ani using arcus tendineus fascia pelvis (Fig. 1.5). Posterior attachment of rectovaginal septum to the levator ani is poorly understood but we will refer to it as the posterior arcus (Fig. 1.6) [10]. The anterior compartment is home to the urethra and the lower part of the bladder. The middle compartment is the vagina, and the posterior compartment is home to anorectum (Fig. 1.7). This analogy is not far from reality. When one looks at the pelvic floor structures, the three compartments are clearly separated as described (Fig. 1.8). Compartmentalization of the pelvic floor has lead to different medical specialties looking at that specific compartment and paying less attention to the whole pelvic floor (Fig. 1.9).
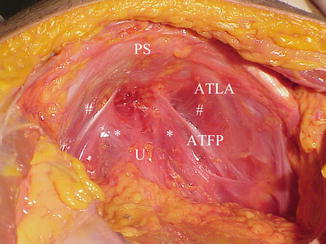
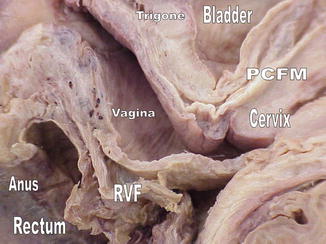
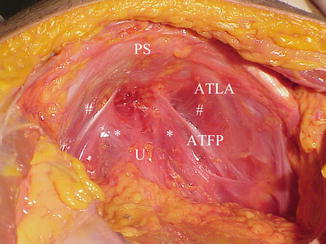
Fig. 1.5
Retropubic anatomy showing points of attachments of the ATLA and the ATFP. The urethra sits on the hammock like pubocervical fibromuscularis. # denotes the levator ani attachment to the obturator internus muscle © SHOBEIRI 2013
Fig. 1.6
Room analogy; the line of attachment of the pubocervical fascia to the levator ani is arcus tendineus fascia pelvis. The line of attachment of the rectovaginal fascia to the levator ani is the posterior arcus. Both are shown as red lines © SHOBEIRI 2013
Fig. 1.7
Room analogy; three compartments separation © SHOBEIRI 2013
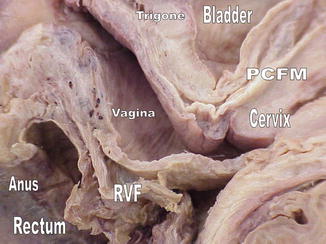
Fig. 1.8
Midsagittal anatomy of an intact cadaveric specimen demonstrating the three different compartments © SHOBEIRI 2013
Fig. 1.9
Room analogy; each area or compartment may be managed by a different specialist. There is a great need for one specialty that understands the interaction between different compartments and manages them concurrently as much as possible © SHOBEIRI 2013
If one looks at the middle compartment from the side, he or she can appreciate different levels of support as described by DeLancey and colleagues [11] (Fig. 1.10). Looking at these supportive structures from the sagittal view exposes the connective tissue elements that keep the room standing. Generally, a “suspension bridge” analogy is useful for to describing these structures (Fig. 1.11). Although in room analogy, the anterior, middle, and posterior compartments house the pelvic organs; in reality, the pelvic organs are part of the pelvic floor and play an important supportive role through their connections with structures, such as the cardinal and uterosacral ligaments. Adapting this suspension bridge to human body, perineal body and the sacrum become the two anchoring points of the bridge. Perineal membrane (DeLancey Level III) and the uterosacral ligaments (DeLancey Level I) form the two masts of the suspension bridge (Fig. 1.12). The lateral wires are the levator ani muscles of the lateral wall (Fig. 1.13) and the attachments of the vagina to the levator ani muscles laterally in the mid part of the vagina forms Delancey’s Level II support. The levator ani muscles and the interconnecting fibromuscular structures support bladder and urethra anteriorly, vaginal canal in the middle, and anorectal structures posteriorly (Fig. 1.14).
Fig. 1.10
Room analogy; level one support are provided by the uterosacral-cardinal ligament complex which keep the room upright. These are demonstrated as the yellow arrows. The level II supports are provided by the lateral tendineus attachments drawn as red lines. The level III support is provided by perineal membrane which is the green area © SHOBEIRI 2013
Fig. 1.11
Suspension bridge analogy; the depiction of a normal bridge © SHOBEIRI 2013
Fig. 1.12
Suspension bridge analogy; the depiction of a suspension bridge adapted to human female pelvic floor structures. The red masts are the ischial spine and the pubis. The blue lines are the levator ani fibers. The green line is the uterosacral ligaments continuous with the posterior arcus line. The anococcygeal ligament provides anchoring point for the posterior structures © SHOBEIRI 2013
Fig. 1.13
Suspension bridge analogy; the depiction of a suspension bridge adapted to human female pelvic floor structures. The levator ani fibers have intricate and overlapping paths. The puboanalis (PA) and puboperinealis form some of the supportive structures of the perineum. The puborectalis (PR) fibers form the sling behind the rectum. Pubovisceralis (PV) is a collective term we have applied here to the iliococcygeus and pubococcygeous fibers. The levator plate (LP) is formed by overlapping of the PV and PR fibers © SHOBEIRI 2013
Fig. 1.14
Suspension bridge analogy; the depiction of different compartments of pelvic floor © SHOBEIRI 2013
Like a room or a suspension bridge, the pelvic floor is subjected to loads that should be appropriate for its design. Should these loads exceed what the pelvic floor is capable of handling there would be failure in one or multiple supportive elements. Pelvic floor is not a static structure. The levator ani works in concert with the ligamentous structures to withstand intraabdominal pressure that could predispose to POP and urinary or fecal incontinence during daily activities (Fig. 1.15). The lower end of the pelvic floor is held closed by the pelvic floor muscles, preventing prolapse by constricting the base. The spatial relationship of the organs and the pelvic floor are important. Pelvic support is a combination of constriction, suspension, and structural geometry.
Fig. 1.15
Right lateral standing anatomic depiction of the three compartments exposed to intraabdominal pressure which results in activation of the muscles to prevent prolapse or urinary and fecal incontinence. B bladder, Cx cervix, R rectum, LA levator ani, U urethra, V vagina, A anus © SHOBEIRI 2013
The levator ani muscle has puboperinealis, puboanalis, pubovaginalis, puborectalis, pubococcygeus, and iliococcygeus subdivisions (Fig. 1.16). Pubococcygeus is a functional unit of the iliococcygeus and these two collectively are known as the pubovisceralis muscle. The relationship of these muscles to each other is interesting as they criss cross in different angles to each other (Figs. 1.17 and 1.18).
Fig. 1.16
The relative position of levator ani subdivisions during ultrasound imaging. IC iliococcygeus, PP puboperinealis, STP superficial transverse perinei, PA puboanalis. Illustration: John Yanson. Shobeiri. Ultrasono-graphy Validation. Obstet Gynecol 2009
Fig. 1.17
Right hemipelvis of a fresh frozen pelvis showing the overlapping of the levator ani subdivisions fibers. The orange arrows: puborectalis; the blue arrows: iliococcygeus; the white arrows: pubococcygeus. Note the relationship between the iliococcygeus and pubococcygeus fibers. © SHOBEIRI 2013
Fig. 1.18
Right hemipelvis of a fresh frozen pelvis with the organs removed. The puborectalis (PR), iliococcygeus (IC), and pubococcygeus (PC) form the lateral sidewall. Note the relationship between the iliococcygeus and pubococcygeus fibers. © SHOBEIRI 2013
1.2 Practical Anatomy and Prolapse
1.2.1 Overview
Level I support is composed of the uterosacral and cardinal ligaments which form the support of the uterus and upper 1/3 of the vagina. Stretching and failure of level I can result in pure apical prolapse of the uterus or an enterocele formation. At Level II, there are direct lateral attachments of the pubocervical fibromuscularis and rectovaginal fibromuscularis to the lateral compartments formed by the levator ani muscles. The variations of defects in this level will be described in the following sections. In the Level III the vaginal wall is anteriorly fused with the urethra, posteriorly with the perineal body. Levator ani muscles in this area are poorly described, but mostly consist of fibrous sheets that envelop the lateral aspects of the vaginal introitus.
1.2.2 Apical Segment
While level I cardinal and uterosacral ligaments can be surgically identified supporting the cervix and the upper 1/3 of the vagina [12, 13], as they fan out toward the sacrum and laterally, they become a mixture of connective tissue, blood vessels, nerves, smooth muscle, and adipose tissue. The uterosacral ligaments act like rubber bands in that they may lengthen with initial Valsalva, but resist any further lengthening at a critical point in which they have to return to their comfortable length or break (Fig. 1.19). Level I and levator ani muscles are interdependent. Intact levator ani muscles moderate the tension placed on the level I support structures and intact level I support lessen the pressure imposed from above on the pelvic floor.
Fig. 1.19
Right hemipelvis of a fresh frozen pelvis showing the uterosacral fibers. The borders of the ligament are shown in dotted line. Cx cervix, C coccyx, PS pubic symphysis. © SHOBEIRI 2013
1.2.3 Anterior Compartment
Anterior compartment support depends on the integrity of vaginal muscularis and adventitia and their connections to the arcus tendineus fascia pelvis. The arcus tendineus fascia pelvis is at one end connected to the lower sixth of the pubic bone, 1–2 cm lateral to the midline, and at the other end to the ischial spine. A simple case of a distension cystocele could result from a defect in pubocervical fibromuscularis (Fig. 1.20a, b)
Fig. 1.20
Room analogy; (a): an occult pubocervical fibromuscularis defect can result in an overt cystocele (b). © SHOBEIRI 2013
The anterior wall fascial attachments to the arcus tendineus fascia pelvis have been called the paravaginal fascial attachments by Richardson et al. [14]. Detachment of arcus tendineus from the levator ani is associated with stress incontinence and anterior prolapse. The detachment can be unilateral (Fig. 1.21) or bilateral (Fig. 1.22) causing a displacement cystocele. In addition, the defect can be complete or incomplete. The surgeon who performs an anterior repair on Fig. 1.22 in reality worsens the underlying disease process. The upper portions of the anterior vaginal wall can prolapse due to lack of Level I support and failure of uterosacral-cardinal complex. Over time this failure may lead to increased load in the paravaginal area and failure of level II paravaginal support. A study of 71 women with anterior compartment prolapse has shown that paravaginal defect usually results from a detachment of the arcus tendineus fascia pelvis from the ischial spine, and rarely from the pubic bone [15]. Resuspension of the vaginal apex at the time of surgery in addition to paravaginal or anterior colporrhaphy may help to return the anterior wall to a more normal position or at least prevent future failures. Another scenario that the surgeon faces is the lack of any tangible fibromuscular tissue in the anterior compartment (Fig. 1.23). Plication of the available tissue may cause vaginal narrowing and dyspareunia. The knowledge of this condition is essential as it will require bridging of the anterior compartment with autologous fascia lata graft [16] or other commercially available tissue augmentation.
Fig. 1.21
Right hemipelvis of a fresh frozen pelvis showing a paravaginal defect repair outlined in green © SHOBEIRI 2013
Fig. 1.22
Room analogy; bilateral detachment of the pubocervical fibromuscularis can result in a cystocele © SHOBEIRI 2013
Fig. 1.23
Room analogy; absence or severe deficiency of the pubocervical fibromuscularis can result in a cystocele © SHOBEIRI 2013
Various grading systems such as Pelvic Organ Prolapse Quantification (POPQ) system [17




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree