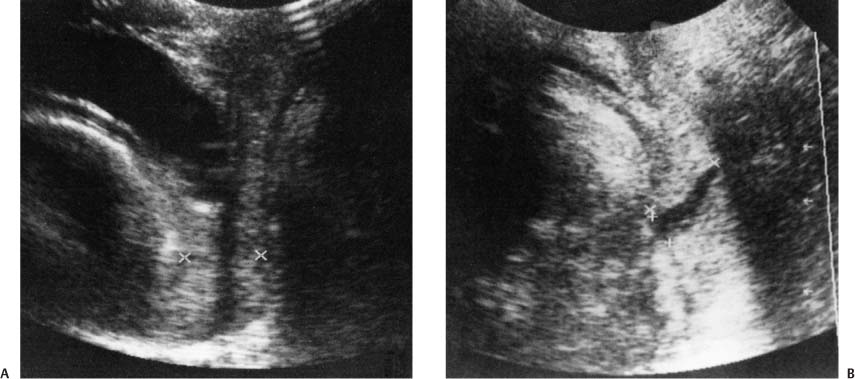
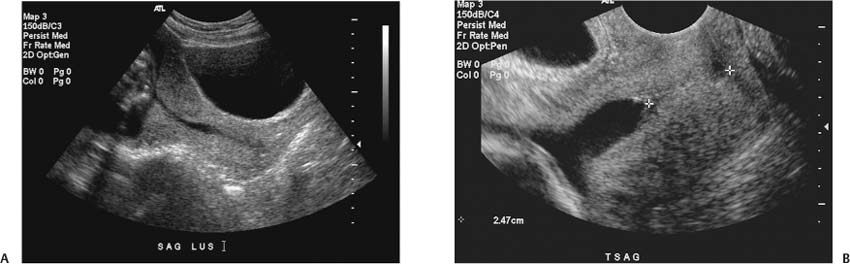
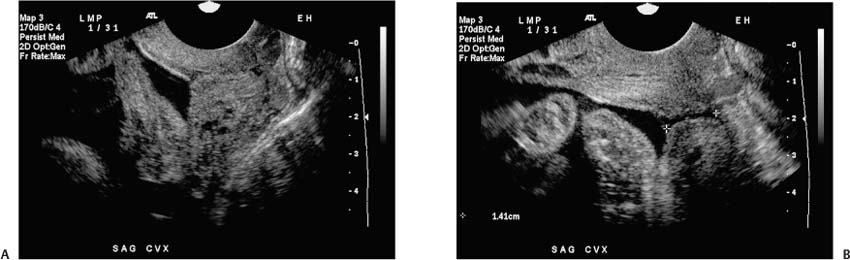
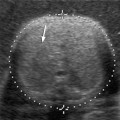
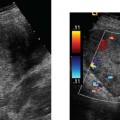
11 Premature Labor Premature delivery (delivery before 37 weeks gestational age) is a major cause of perinatal morbidity and mortality, being responsible for 70% of perinatal deaths.1,2 The rate of premature delivery in the United States increased from 9.4% in 1981 to 11.9% in 2001.3 This change is attributed to an increase in the population at high risk for premature delivery. The number of twin births increased by 32% between 1989 and 2000. In the same time period, the number of triplet births almost tripled and the number of quadruplet births more than doubled. These changes are, in part, attributable to the increased use of assisted reproductive technology.4 In addition, patients with either or both medical and reproductive risk factors previously advised not to conceive are now attempting pregnancy under the supervision of high-risk obstetrical teams. These patients often deliver before full term for medical reasons. Indicated premature delivery presently accounts for 15 to 25% of premature births.3 However, there are some encouraging trends in pre-term morbidity and mortality. Advances in prenatal and neonatal care have reduced perinatal mortality from premature deliveries. The lower limit of infant viability has been extended: presently over 50% of infants born at 24 to 25 weeks survive to be discharged home from the hospital.3,2 However, the cost of providing care to an extremely premature infant in the immediate neonatal period is 50 times more than that of an infant born at term, and the health care cost for the rest of the first year of life is 20 times more expensive.6 There are frequently significant physical and neurological sequelae in children born very prematurely as well.7 Although the total number of premature births in the last decade has not decreased, there has been a decrease in the proportion of infants born very prematurely: 1.57% of singleton births occurred before 32 weeks in 2001, compared with 1.69% in 1990. The proportion of singleton births between 32 to 36 weeks increased from 8.01% in 1990 to 8.81% in 2001.3 These infants are technically considered as premature births but have fewer morbidities than those delivered at an earlier gestational age. This shift to a less vulnerable stage of the pregnancy may in part be the result of advances in the diagnosis of premature labor so that intervention can be instituted earlier and more effectively. Figure 11–1 Normal transvaginal view of the cervix. The endocervical canal is indicated with calipers. Obstetrical ultrasound plays an important role in the evaluation of patients in spontaneous premature labor, not only in the determination of gestational age and fetal well-being, but also in the assessment of the cervix. Sonography, using a transvaginal (Fig. 11–1) or transperineal (Fig. 11–2) approach, provides an additional method beyond the traditional digital examination for the study of the uterine cervix during pregnancy. The cervix plays a unique role in pregnancy. The closed and uneffaced cervix physically maintains the fetus in utero, and secretions from the cervix form the mucous plug that is partly responsible for preventing ascending infection. The cervix can be the cause of premature delivery in cases of incompetent cervix. An incompetent cervix, which may be congenital or acquired, is associated with a silent decrease in cervical length and painless dilatation of the cervix that may result in premature labor recognized only at an advanced stage. Changes in cervical length, dilatation, and effacement can reflect the progression of premature labor. Recognizing these changes can help identify patients that are heading toward premature delivery. This chapter reviews the use of sonography in the assessment of the cervix in premature labor and delivery. Figure 11–2 Transperineal scan. (A) Calipers mark the internal and external os in a normal-appearing cervix. (B) In a different patient, ballooning membranes are present measures length of open cervix; meaures dilation. Figure 11–3 (A) Transabdominal view of the cervix and lower uterine segment of a patient scanned at the 20th week of her pregnancy. (B) Funneling of the cervix noted incidentally 40 minutes into the scan. There was no subjective complaint of uterine contraction. (C) Cervical funneling was confirmed on transvaginal scan. The closed cervical length (1.4 cm) is marked with calipers. Transvaginal or transperineal scan of the cervix should be performed if a short cervix is noted transabdominally. Figure 11–4 Pitfalls of overfull bladder and contraction at the lower uterine segment. (A) Compression of the cervix by a full bladder may give the impression of a long cervix. In this image there is also a contraction at the lower uterine segment that adds to the impression of a long cervix. The contraction can be recognized by the thickness of the myometrium in the anterior and posterior lower uterine segment. This can give the false appearance of funneling above a long closed cervix. (B) Cervical funneling was demonstrated by transvaginal scan with an emptied bladder a few minutes after the image in (A) was taken. The transabdominal approach to scanning the cervix is less accurate than the transvaginal or transperineal approach because the cervix is poorly visualized when the maternal bladder is empty (Fig. 11–3).8 However, overdistention of the bladder artificially increases the length of the cervix and can obscure the presence of a dilated cervix (Fig. 11–4). Maternal body habitus or a low fetal presenting part can also limit visualization of the cervix transabdominally. Because of the problems inherent with transabdominal scanning, imaging of the cervix is best performed with either a transperineal or a transvaginal approach.9–11 Transperineal scanning (Fig. 11–2) is performed with a 3.5 to 5 MHz sector probe. The probe should be covered by a condom or plastic wrap for hygienic reasons and infection control.12 The probe is placed on the perineum, over the labia minora, and is aimed in the direction of the vaginal canal toward the cervix. Transperineal scanning is very operator-dependent. Pitfalls include obscuration of the cervix by rectal gas, shadowing by the pelvic bones, and inadequate visualization of the external os due to direct contact of the vaginal wall with the cervix. Hertzberg et al have shown that elevating the patient’s hips and buttocks off the scanning table can improve cervical visualization in cases where routine transperineal views are inadequate.13 Transperineal sonography has an advantage over transvaginal sonography in that the probe is not introduced into the vagina. Therefore, in patients with active bleeding or in whom ruptured membranes are suspected, transperineal scanning is our recommended approach. Additional benefits are that transperineal scanning is more comfortable for the patient than is transvaginal scanning and no artifact is produced by pressure exerted on the cervix. A 5 to 10 MHz vaginal probe is used in transvaginal scanning of the cervix (Fig. 11–1). The probe should be disinfected prior to use and covered by a condom or probe cover. Latex allergy is present in some patients, and in those cases, a nonlatex condom or a nonlatex glove can be used to cover the probe. When using the transvaginal approach, care should be taken not to insert the probe abruptly or too deeply. The ultrasound monitor should be viewed in real time during insertion of the probe to avoid traumatizing prolapsed fetal membranes or a low placenta (Fig. 11–5). The cervix should be identified and then the probe should be slightly withdrawn to obtain an accurate image of the internal os, external os, and cervical length (Fig. 11–6). The image of the cervix should meet the following criteria: (1) the internal os appears either flat or as an isosceles triangle, (2) the whole length of the cervical canal can be visualized, (3) a symmetric image of the external os can be obtained, and (4) the distance from the surface of the posterior lip to the cervical canal is equal to the distance from the anterior lip to the cervical canal.14 The cervix should be observed for several minutes to detect dynamic change of the internal os and cervical length. Even patients with known placenta previa can be safely scanned with a transvaginal probe, although for patients with active bleeding we recommend the transperineal approach. Figure 11–5 Ballooning membranes. When ballooning membranes are seen, the probe should not be inserted further into the vagina, but should be removed. The patient should be placed in Trendelenburg’s position and transferred to labor and delivery. Figure 11–6 Pitfall in measuring cervical length. (A) Pressure was exerted on the cervix by the vaginal probe. Note the relatively thin anterior cervical lip when compared with the posterior lip. (B) Funneling of the internal os and a short cervix (calipers) were noted after the probe was withdrawn slightly to eliminate the pressure artifact. The cervical length is measured from the internal os to the external os. When the internal os is open, with funneling, only the closed portion of the cervix is measured. When funneling is present, the anteroposterior diameter (at the region of the presumed internal os) and length of the funnel (from the presumed internal os to the closed portion of the cervix) are also measured. A cervix that has prolapsing membranes into the cervical canal on ultra-sound may still feel long and closed on clinical examination. The technical success of placing a cervical cerclage when there are prolapsing fetal membranes into the cervical canal is influenced by the clinical length of the cervix and the width and length of the canal dilation, and not just the functional length of the cervix. In addition, it is not clear how a 2-cm long cervix with a closed cervical canal behaves when compared with a 4-cm cervix with prolapsing membranes and a functional length of 2 cm. A complete description of the sonographic picture of the cervix, including the total length, the width of dilation of the internal os and along the cervical canal, and the remaining closed (functional) length conveys the entire appearance.15 It is difficult to distinguish the cervix from the lower uterine segment in the nonpregnant state and in the first trimester. By the second trimester, the growing amniotic sac provides a clear landmark for the internal cervical os. Cervical length measurements (defined as the distance between the internal and the external cervical os) have been shown to correlate well with digital examination of the cervix. Many authors suggest cervical sonography is superior to digital examination because the measurements are reproducible, the intraabdominal portion of the cervix can be measured, and the internal cervical os, where early changes from incompetent cervix and premature labor occur, can be assessed.16–20 Sonography also has the theoretical advantage of less risk of infection and irritation of the cervix than digital examination. Cervical length often measures over 5 cm in the first trimester,21 but some of this length may reflect the inability to define clearly the upper cervix from the lower uterine segment. Most studies define a normal cervical length as 3 to 4 cm in midpregnancy.22–24 In a study sponsored by the National Institute of Child Health and Human Development Network (NICHD), 2915 women with singleton pregnancies were studied by transvaginal cervical ultrasound examination at 22 to 24 weeks with follow-up examinations in 2531 patients at 26 to 28 weeks gestation. The mean cervical length was 3.52 cm in the first group and 3.37 cm in the second group.25 The distribution of cervical lengths in the population followed a normal bell curve. At 24 weeks gestation, the 10th and 90th percentiles are 25 mm and 45 mm, respectively. Normal cervical length appears to be the same in nulliparous and multiparous women, and both exhibit shortening of the cervix as pregnancy progresses. Such normal shortening of the cervix does not result in premature delivery.26–29 It is therefore important to distinguish between the normal, expected rate of cervical shortening as compared with an accelerated rate of change that may result in premature delivery. Patients carrying multiple gestations have significantly shorter cervical lengths than singleton pregnancies when matched for gestational age. Normograms of cervical length have been developed for twins.30,2 In singleton pregnancies, cervical length usually remains above 4 cm through 37 weeks, whereas in twin pregnancies it is often less than 3 cm by 32 weeks. The most commonly used sonographic parameters in the assessment of premature labor are cervical length, dilation of the cervix, and the appearance of the internal cervical os. The length of the cervix of patients who have a history of premature delivery might not be different from the general population when measured in the first trimester.32–34 It is important to follow patients who are at risk for premature delivery. There is an inverse relationship between the sonographically measured length of the cervix at midpreg-nancy and the risk of preterm delivery. Most studies place the at-risk threshold at 2 to 3 cm.35–38 The NICHD study demonstrated that a sonographically measured cervical length of less than 3.2 cm at 24 weeks gestation is associated with a sixfold increased risk of premature delivery before 35 weeks, and a cervical length of 1.2 cm at 24 weeks has a 14-fold risk of premature delivery. A transvaginally measured cervical length of less than 2 cm at 24 weeks has a sensitivity of 23% and a specificity of 97% for the prediction of preterm delivery. Cervical lengths measured sonographically at 24 weeks gestation of 3, 2.5, and 2 cm are associated with premature delivery in 9.3, 18, and 25%, respectively, of cases.25 Combining the patients’ obstetrical history and the cervical length measurement may increase the predictive value of the cervical sonography. Some authors have proposed using a single transvaginal measurement of cervical length at midpregnancy to detect patients at risk for premature delivery.39,2 However, the cost-effectiveness of such a program for the general population is questionable given the low prevalence of premature birth in the low–risk population.41–43 The inverse relationship between cervical length and the risk for premature labor also holds for multiple gestations.43–50 Imseis et al in their study of twin pregnancies noted that a cervical length of 3.5 cm at 24 to 26 weeks predicts delivery at term in the majority of cases, whereas a mean cervical length of 2.7 cm is associated with either premature delivery or necessity for obstetrical intervention.44 In addition to cervical length, the appearance of the internal os is important in the assessment of preterm labor. The presence of funneling or wedging (dilation of the internal os with prolapse of fetal membranes into the cervical canal) is associated with preterm delivery. Ominous signs predicting preterm delivery include a funnel length of greater than 1.5 cm, a funnel width of greater than 1.4 cm, a residual cervical length of less than 2 cm, and funneling over 40% of the cervical length.15 There are still controversies as to which of these is most important. Guzman et al maintain that cervical length has the highest predictive value.52 Other studies, however, find that the internal cervical os dilation and the extent of the cervical funneling are equally important in predicting the group at risk for premature delivery.53–55 Further research with standardized criteria for the description of cervical change will help evaluate the importance of these markers. Recently, there has been interest in the use of fetal fibronectin,56–59 prostaglandin,60 and interleukin-6 and 8 as-says61 on swab specimens in combination with cervical sonography to identify patients at risk for premature labor and delivery. The most promising of such combined protocols found that a negative fetal fibronectin test on the vaginal swab and a cervical length of over 3 cm on ultrasound examination have a 97% negative predictive value for premature delivery in the subsequent 14 days.59
Ultrasound Evaluation
Technical Aspects
The Cervix in Normal Pregnancy
The Role of Cervical Sonography in Premature Labor
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree