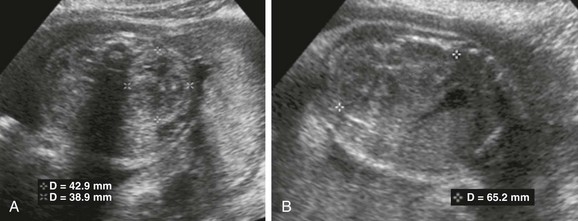
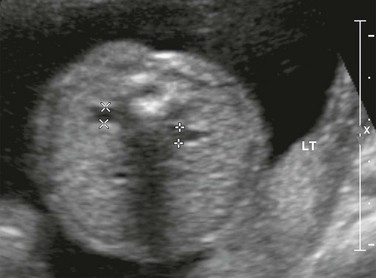
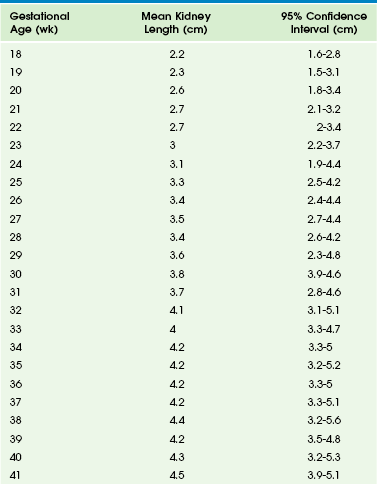
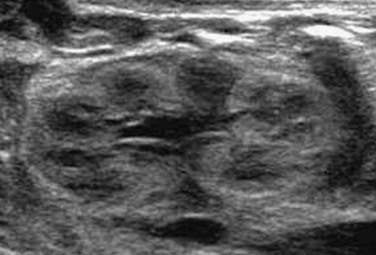
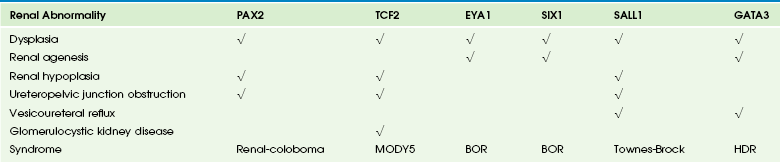
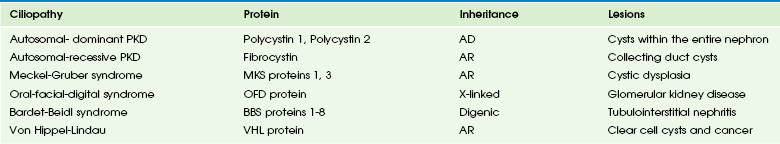
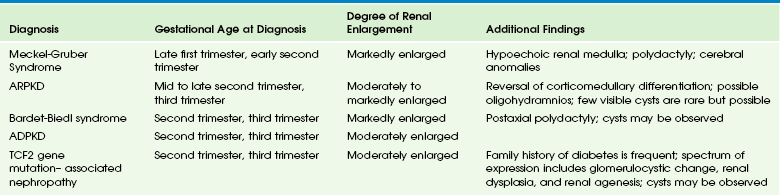
Chapter 113 Fetal genitourinary system abnormalities encompass a wide spectrum of disorders varying in degrees of severity and include developmental anomalies, obstructive lesions in the urinary tract, and renal parenchymal diseases. The prenatal evaluation of the genitourinary system includes assessment of the amniotic fluid, the kidneys, the bladder, and associated anomalies. Amniotic fluid is important for normal fetal development, particularly the fetal lungs. In the first trimester, amniotic fluid forms as a dialysate of maternal serum. Fetal urine production begins by 12 weeks of gestation and becomes the major source of amniotic fluid by 16 weeks. Fetal urine production is typically 120 mL/day at 20 weeks and increases gradually to 1200 mL/day by term. The fetus voids every 30 to 60 minutes. The bladder should be visualized at least once during an examination.1,2 Identification of the fetal urinary bladder is attempted in the first trimester ultrasound, and more detailed evaluation of the kidneys and bladder is a fundamental part of the second trimester fetal anatomic assessment. Complex cases such as exstrophy, confusing duplex collecting systems, and obstructive masses may be further evaluated by fetal magnetic resonance imaging (MRI).3–5 Sonographic fetal anatomic assessment may be limited in the setting of oligohydramnios, and MRI may be particularly useful. Prenatal findings may influence the further pursuit of genetic and laboratory testing or surgical intervention and may guide the delivery plan. Overview and Imaging: Fetal kidneys can be identified at 13 weeks of gestation. Normal renal sizes at various gestations (mean kidney length in millimeters is slightly longer than weeks of gestation) are shown in Table 113-1.6,7 Corticomedullary differentiation is apparent by 20 weeks of gestation (Fig. 113-1). Renal calyces and ureters typically are not seen on ultrasound unless they are pathologically dilated,8 and the renal pelvis is only readily visualized once the anterior-posterior diameter exceeds 2 mm.9 The fetal bladder can be visualized at 10 weeks of gestation. The bladder wall should not measure more than 3 mm. Bladder wall thickening may be a sign of outlet obstruction.10,11 Table 113-1 Modified from Cohen HL, Cooper J, Eisenberg P, et al. Normal length of fetal kidneys. AJR Am J Roentgenol. 1991;157:545-548. Figure 113-1 A normal fetal kidney at 32 weeks of gestation. As mentioned earlier, the amniotic fluid volume is a reflection of renal health. Oligohydramnios (defined by an amniotic fluid index less than 8 cm)12 may be seen in the setting of placental insufficiency, intrauterine growth retardation, chromosomal abnormality, premature rupture of membranes, post-dates gestation, or urologic pathology (Box 113-1).13 Overview: Fetal renal echogenicity may be abnormally increased as a normal variant but more often reflects an underlying abnormality. The fetal kidney is considered echogenic if sonographically it is brighter than the fetal liver. Echogenic kidneys are observed in approximately 1 to 2 per 1000 fetal ultrasounds, and approximately 10% of cases of renal malformations include echogenic kidneys.14,15 Etiologic considerations for the echogenic kidney are summarized in Box 113-2.16–24 If echogenic kidneys are identified and the amniotic fluid volume is normal, the findings suggest nonlethal renal disease. Echogenic kidneys with oligohydramnios portend a very poor prognosis.25 Overview: Congenital cystic renal diseases occur in about 2 to 4 in 1000 live births and include autosomal-dominant and autosomal-recessive polycystic kidney disease (Fig, 113-2 and Video 113-1), multicystic dysplastic kidney (Fig. 113-3), cystic glomerulopathies, and other cystic renal dysplasias. The complex pathogenesis of these disorders involves an abnormal orchestration of transcription and growth factor expression (Table 113-2), as well as ciliopathies affecting the renal tubule primary cilium (Table 113-3).26–29 Structural and functional abnormalities in primary cilia contribute to various cystic phenotypes that involve not only the kidney but the liver and pancreas as well.27 Table 113-2 Selected Examples of Gene Mutations Resulting in Congenital Urinary Tract Abnormalities Modified from Bonsib SM. The classification of renal cystic diseases and other congenital malformations of the kidney and urinary tract. Arch Pathol Lab Med. 2010;134(4):554-568. Table 113-3 Ciliopathies: Molecular, Genetic, and Pathologic Features AD, Autosomal dominant; AR, autosomal recessive; PKD, polycystic kidney disease. Modified from Bonsib SM. The classification of renal cystic diseases and other congenital malformations of the kidney and urinary tract. Arch Pathol Lab Med. 2010;134(4):554-568. Figure 113-2 Autosomal-dominant polycystic kidney disease (ADPKD). Figure 113-3 A multicystic dysplastic kidney. Imaging: These types of cystic renal dysplasias may be demonstrated in the fetus either by ultrasound or MRI.27,30–37 Fetal sonographic evaluation of the kidneys should include renal length, overall echogenicity, preservation of corticomedullary differentiation, and presence of macroscopic cysts. Renal size may be considered abnormally increased if it is ≥2 standard deviations (moderately enlarged) or ≥4 standard deviations (markedly enlarged) greater than expected for gestational age.6 Renal echogenicity greater than that of the liver or spleen is abnormal (Fig. 113-4), and corticomedullary differentiation may be lost or reversed if renal parenchymal disease is present.27 MRI also readily shows abnormalities in renal size and detects renal cysts. Dysplastic parenchyma typically increases the T2-weighted signal (e-Fig. 113-5). Figure 113-4 Echogenic kidneys in a fetus at 29 weeks’ gestational age by ultrasound. e-Figure 113-5 Hydronephrosis and renal dysplasia. Approach to Diagnosis: A differential diagnostic approach to fetal echogenic renal cystic diseases is summarized in Table 113-4. If macroscopic cysts are observed without abnormal renal echogenicity, possible etiologies will depend on the number of cysts observed. Visualization of a single renal cyst should prompt consideration of a cystic tumor, a duplex collecting system with cystic dysplasia of the upper pole, urinoma, asymmetric presentation of autosomal-dominant polycystic kidney disease (ADPKD), or an isolated cyst in an otherwise normal kidney. Multiple cysts may be seen with multicystic dysplastic kidney, ADPKD, tuberous sclerosis complex, and TCF2 gene mutation–associated nephropathy. Table 113-4 Differential Diagnosis: Fetal Renal Cystic Disease with Echogenic Kidneys by Ultrasound78,211 From Avni FE, Hall M. Renal cystic diseases in children: new concepts. Pediatr Radiol. 2010;40:9399-946; and Cassart M, Eruin D, Didier F, et al. Antenatal renal sonographic anomalies and postnatal follow-up of renal involvement in Bardet-Biedl syndrome. Ultrasound Obstet Gynecol. 2004;24:51-54. Overview and Imaging: A solid, rounded echogenic mass in the fetal kidney (Fig. 113-6) is most likely to be a congenital mesoblastic nephroma (CMN), also known as a leiomyomatous hamartoma or a fetal renal hamartoma, although a Wilms tumor may present in the fetus as well.38 Both tumor types can replace the kidney or be localized. Tumors may be vascular with cystic areas as a result of hemorrhage and cystic degeneration. Polyhydramnios may occur (it is seen in 40% of renal tumor cases) and may lead to premature labor. Although the CMN is benign, a low-grade malignancy cannot be excluded, and resection is recommended. In one review of 28 prenatally diagnosed renal masses, 26 were CMNs and two were Wilms tumors (stage 1). The two children with Wilms tumors were followed up and remained disease free at ages 4 and 5 years.39 Overview: A commonly seen fetal renal abnormality is pyelectasis (dilatation of the fetal renal collecting system), which is seen in 1% to 5% of screened fetuses.40–46 Numerous factors influence renal pelvis dilation, including maternal hydration, fetal bladder filling, or the presence of an extrarenal pelvis (Fig. 113-7). Fetuses with trisomy 21 have an increased incidence of mild pyelectasis (>4 mm in the second trimester).47 Other anomalies or risk factors should be present before recommending an amniocentesis if mild pyelectasis is observed, because the specificity of aneuploidy with isolated pyelectasis is low.48–50 Most fetuses with mild pyelectasis are normal (approximately 90% or more).43,46,51,52 Regardless of the risk for chromosomal abnormalities, pyelectasis in the fetus may signify either obstruction (Fig. 113-8 and e-Fig.113-9) or vesicoureteral reflux, and therefore follow-up later in gestation and postnatally must be considered. Causes of bilateral hydronephrosis are presented in Box 113-3. Figure 113-7 Extrarenal pelvis. Figure 113-8 A unilateral duplex collecting system with a ureterocele. e-Figure 113-9 Ureteropelvic junction obstruction. Imaging: The degree of collecting system dilatation is based on the anterior to posterior diameter (APD) of the renal pelvis as imaged in transverse plane (Fig. 113-10). Other imaging characteristics that may be pertinent include the morphology of the collecting system (for instance, disproportionately dilated renal pelvis in a configuration suggesting a ureteropelvic junction obstruction), visualization of the ureter, and features of the renal parenchyma, such as cortical echogenicity and the presence of cortical thinning.
Prenatal Imaging and Intervention
Overview
Normal Fetal Genitourinary Tract
A longitudinal sonogram of the fetal kidney shows a thin layer of perinephric fat with normal corticomedullary differentiation. Fetal lobulation is present. A small amount of fluid is present in the central renal pelvis.
Renal Parenchymal Disorders
Cystic Renal Disease
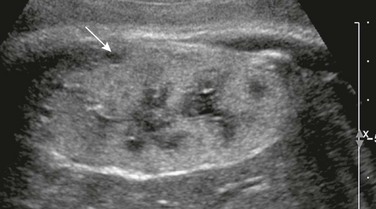
A longitudinal sonogram of a fetus at 36 weeks’ gestational age shows an enlarged echogenic kidney measuring more than 6 cm in length with small peripheral cysts (arrow). The contralateral kidney also was large and echogenic. Amniotic fluid remained normal throughout the pregnancy. The father also has ADPKD. See also Video 113-1 for fetal autosomal-recessive polycystic kidney disease on fetal ultrasound (a cine loop).


A, A sagittal ultrasound view of the right kidney in this 31-week gestational age fetus shows an enlarged kidney with macroscopic cysts not communicating with the collecting system. The minimal amount of discernible renal parenchyma is echogenic and disorganized. B, A sagittal single-shot fast-spin echo T2-weighted magnetic resonance image of a 32-week gestational age fetus shows a multicystic mass (arrow) in the renal fossa with no normal renal tissue.
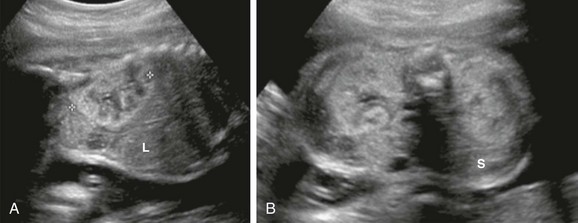
A, The sagittal plane through the right kidney. B, The transverse plane through both kidneys. The renal cortices are brighter than the liver (L) and spleen (S). Renal length is normal for this gestational age, and the amniotic fluid volume is normal.
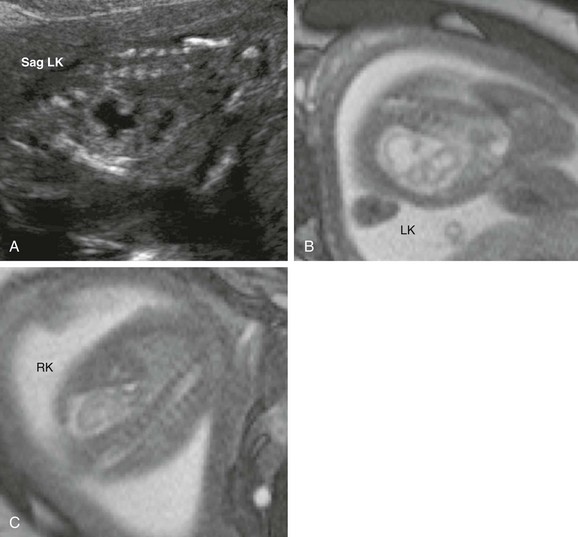
A, A sagittal sonogram of the right kidney in this 21-week gestational age fetus shows hydronephrosis disproportionately affecting the lower calices, as well as echogenic parenchyma. Single-shot fast-spin echo T2-weighted fetal magnetic resonance images acquired at the same age show the left kidney (LK) (B) and the right kidney (RK) (C) in the coronal plane. The more echogenic left lower pole cortex demonstrates subjectively higher T2-weighted signal than does the left upper pole or right kidney. Sag, Sagittal.
Renal Tumors
Antenatal Hydronephrosis

An axial single-shot fast-spin echo T2-weighted magnetic resonance image of both fetal kidneys shows a large extrarenal pelvis on the right (arrow). The renal cortex remains thick.

Sagittal ultrasound images of the right (A) and left (B) kidneys of a 28-week gestational age fetus show abnormal kidneys bilaterally. A right duplex right collecting system is present with pelvocaliectasis. The left kidney shows massive, disproportionate dilatation of the upper collecting system suggestive of a duplex system. A sagittal view of the left aspect of the fetal bladder (C) shows a thin-walled anechoic structure within the bladder lumen consistent with a ureterocele (u).

A coronal single-shot fast-spin echo T2-weighted magnetic resonance image shows a dilated right renal pelvis (arrow) and calyces with parenchymal thinning. The ureter was not dilated.