Pruned appearance of biliary tree develops over time
• CT/MR
 Visualization of greater than expected number of peripheral ducts on MRCP is clue to presence of peripheral intrahepatic ductal strictures
Visualization of greater than expected number of peripheral ducts on MRCP is clue to presence of peripheral intrahepatic ductal strictures
 Chronic involvement results in atrophy of peripheral liver, massive hypertrophy of central liver/caudate (pseudotumor of caudate), and lobulated, rounded liver contour
Chronic involvement results in atrophy of peripheral liver, massive hypertrophy of central liver/caudate (pseudotumor of caudate), and lobulated, rounded liver contour
 Hepatolithiasis, cholelithiasis, and choledocholithiasis are common and appear as signal voids on MR
Hepatolithiasis, cholelithiasis, and choledocholithiasis are common and appear as signal voids on MR
 Visualization of greater than expected number of peripheral ducts on MRCP is clue to presence of peripheral intrahepatic ductal strictures
Visualization of greater than expected number of peripheral ducts on MRCP is clue to presence of peripheral intrahepatic ductal strictures Chronic involvement results in atrophy of peripheral liver, massive hypertrophy of central liver/caudate (pseudotumor of caudate), and lobulated, rounded liver contour
Chronic involvement results in atrophy of peripheral liver, massive hypertrophy of central liver/caudate (pseudotumor of caudate), and lobulated, rounded liver contour– Frequent periductal and perivascular fibrosis, as well as confluent fibrosis in central liver: Low density on CT and T2 hyperintense on MR
 Hepatolithiasis, cholelithiasis, and choledocholithiasis are common and appear as signal voids on MR
Hepatolithiasis, cholelithiasis, and choledocholithiasis are common and appear as signal voids on MR

 with partial opacification of a very dilated left intrahepatic bile duct.
with partial opacification of a very dilated left intrahepatic bile duct.

 is dilated, thickened, and hyperenhancing, suggesting active ductal inflammation.
is dilated, thickened, and hyperenhancing, suggesting active ductal inflammation.IMAGING
General Features
MR Findings
• MRCP demonstrates multifocal “beaded” strictures of intrahepatic and extrahepatic ducts
 Visualization of greater than expected number of peripheral ducts on MRCP is clue to presence of peripheral intrahepatic ductal strictures
Visualization of greater than expected number of peripheral ducts on MRCP is clue to presence of peripheral intrahepatic ductal strictures
 Pruned appearance of biliary tree develops as disease progresses, with obliteration of small peripheral ducts
Pruned appearance of biliary tree develops as disease progresses, with obliteration of small peripheral ducts
 Visualization of greater than expected number of peripheral ducts on MRCP is clue to presence of peripheral intrahepatic ductal strictures
Visualization of greater than expected number of peripheral ducts on MRCP is clue to presence of peripheral intrahepatic ductal strictures Pruned appearance of biliary tree develops as disease progresses, with obliteration of small peripheral ducts
Pruned appearance of biliary tree develops as disease progresses, with obliteration of small peripheral ducts• T1W C+ images (particularly on arterial phase images) demonstrates heterogeneous, patchy hyperenhancement often in periductal distribution
• Chronic involvement results in atrophy of peripheral liver, hypertrophy of central liver, and lobulated, rounded liver contour
CT Findings
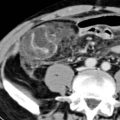
• Dilation of intrahepatic and extrahepatic ducts
 “Beaded” morphology may be difficult to appreciate on CT, but multiplanar reformations often helpful
“Beaded” morphology may be difficult to appreciate on CT, but multiplanar reformations often helpful
 Irregularity and mild dilatation of peripheral ducts, with sites of dilatation alternating with normal caliber ducts
Irregularity and mild dilatation of peripheral ducts, with sites of dilatation alternating with normal caliber ducts
 “Beaded” morphology may be difficult to appreciate on CT, but multiplanar reformations often helpful
“Beaded” morphology may be difficult to appreciate on CT, but multiplanar reformations often helpful Irregularity and mild dilatation of peripheral ducts, with sites of dilatation alternating with normal caliber ducts
Irregularity and mild dilatation of peripheral ducts, with sites of dilatation alternating with normal caliber ducts• End-stage PSC: Markedly dysmorphic, cirrhotic liver with progressive hypertrophy of caudate lobe/deep right lobe and atrophy of peripheral liver with abnormally rounded, lobulated liver contour
 Markedly hypertrophied central liver/caudate (with atrophy of liver periphery) often described as pseudotumor of caudate
Markedly hypertrophied central liver/caudate (with atrophy of liver periphery) often described as pseudotumor of caudate
 Periphery of liver often appears hypodense due to fibrosis and hepatocellular necrosis resulting from poor biliary drainage of liver periphery
Periphery of liver often appears hypodense due to fibrosis and hepatocellular necrosis resulting from poor biliary drainage of liver periphery
 Central liver often relatively higher attenuation compared to peripheral liver due to preserved drainage by patent short bile ducts
Central liver often relatively higher attenuation compared to peripheral liver due to preserved drainage by patent short bile ducts
 Markedly hypertrophied central liver/caudate (with atrophy of liver periphery) often described as pseudotumor of caudate
Markedly hypertrophied central liver/caudate (with atrophy of liver periphery) often described as pseudotumor of caudate Periphery of liver often appears hypodense due to fibrosis and hepatocellular necrosis resulting from poor biliary drainage of liver periphery
Periphery of liver often appears hypodense due to fibrosis and hepatocellular necrosis resulting from poor biliary drainage of liver periphery Central liver often relatively higher attenuation compared to peripheral liver due to preserved drainage by patent short bile ducts
Central liver often relatively higher attenuation compared to peripheral liver due to preserved drainage by patent short bile ductsRadiographic Findings
• Cholangiography (ERCP or PTC)
 Multifocal short segment biliary strictures involving both intrahepatic and extrahepatic ducts with intervening sites of normal or mildly dilated ducts
Multifocal short segment biliary strictures involving both intrahepatic and extrahepatic ducts with intervening sites of normal or mildly dilated ducts
 Intraluminal filling defects (5-10%) usually represent intraductal calculi particularly when small (2-5 mm)
Intraluminal filling defects (5-10%) usually represent intraductal calculi particularly when small (2-5 mm)




 Multifocal short segment biliary strictures involving both intrahepatic and extrahepatic ducts with intervening sites of normal or mildly dilated ducts
Multifocal short segment biliary strictures involving both intrahepatic and extrahepatic ducts with intervening sites of normal or mildly dilated ducts – Mural irregularity of ducts common (50%), ranging from a fine, brush-border appearance to coarse, shaggy, or frankly nodular appearance
 Intraluminal filling defects (5-10%) usually represent intraductal calculi particularly when small (2-5 mm)
Intraluminal filling defects (5-10%) usually represent intraductal calculi particularly when small (2-5 mm)Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree